Heart rhythm problems (cardiac arrhythmias) occur when the electrical impulses that coordinate our heartbeats don’t work properly, causing the heart to beat either too fast, or too slow, or sometimes irregularly
WHAT ARE THE COMMON HEART RHYTHM DISORDERS?
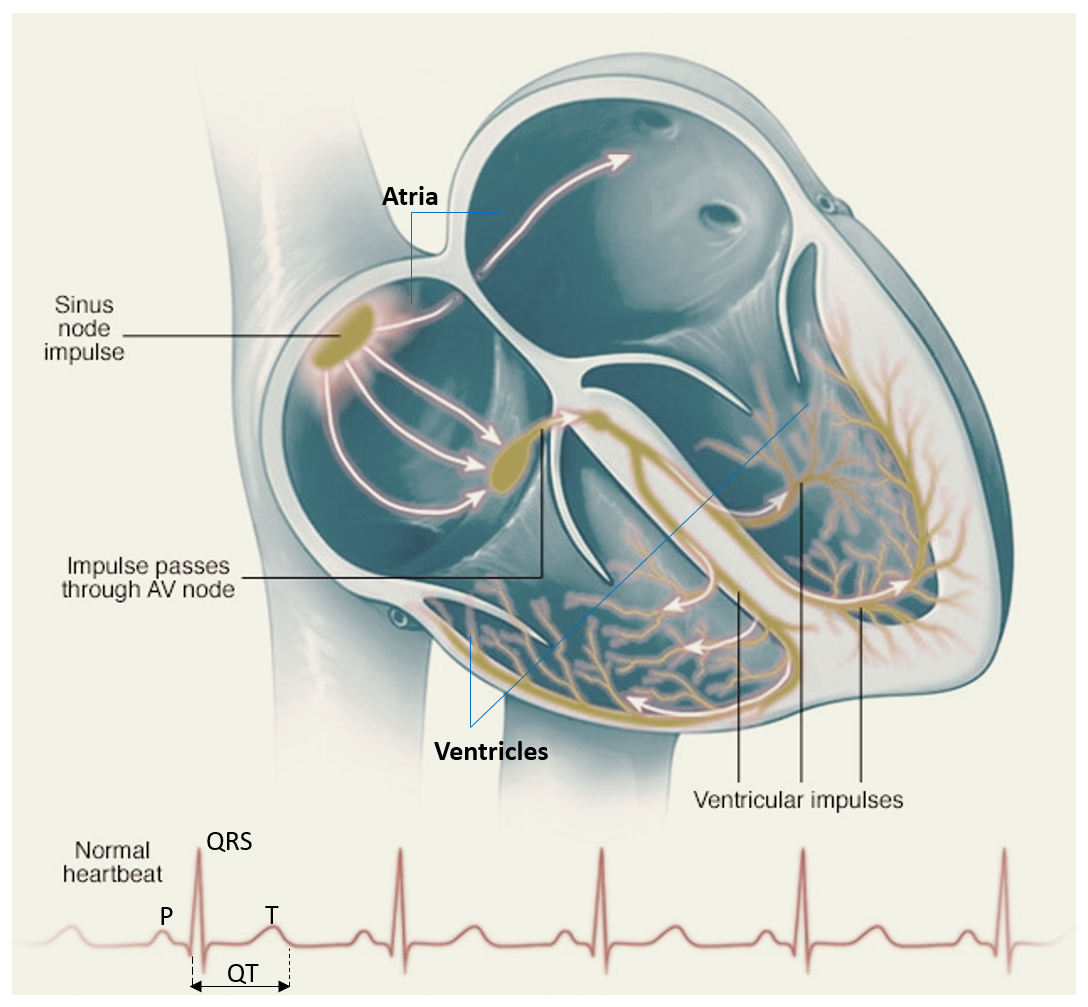
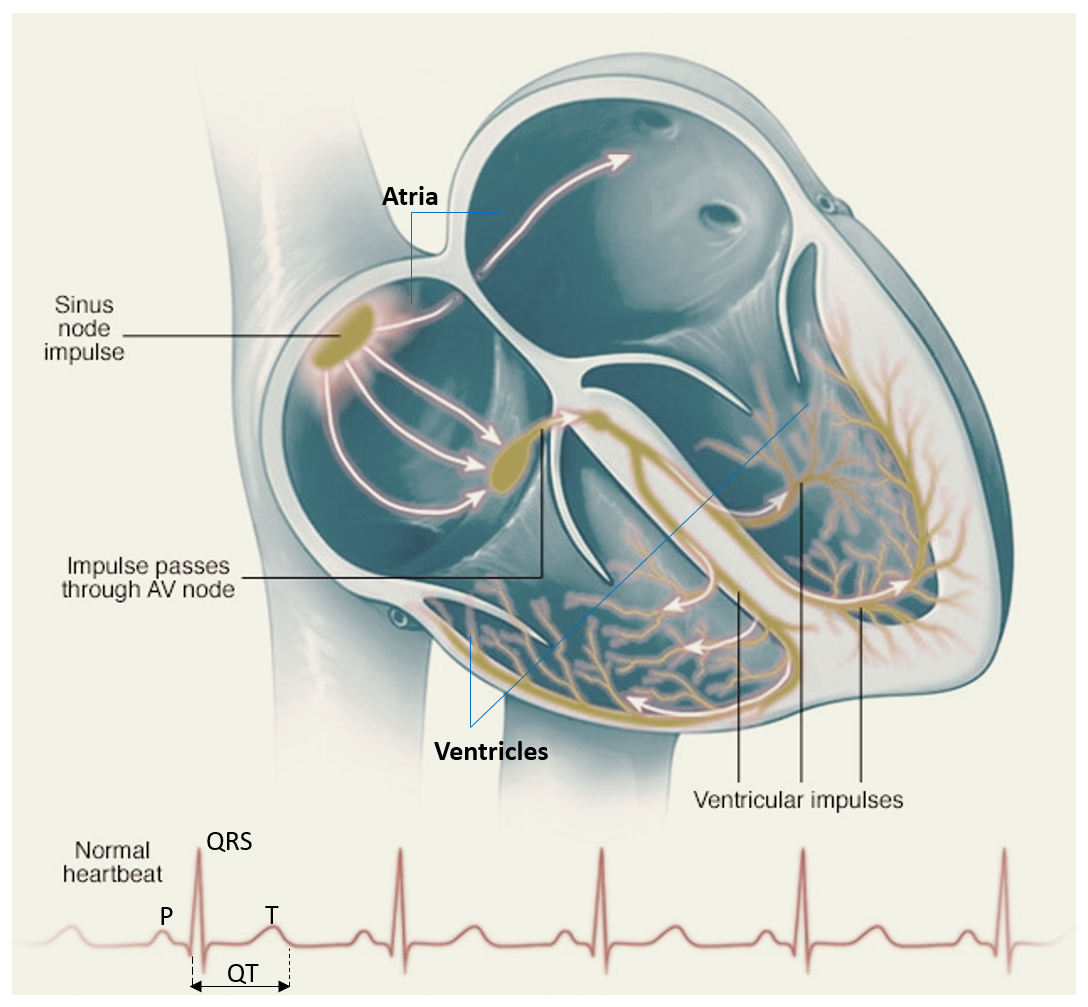
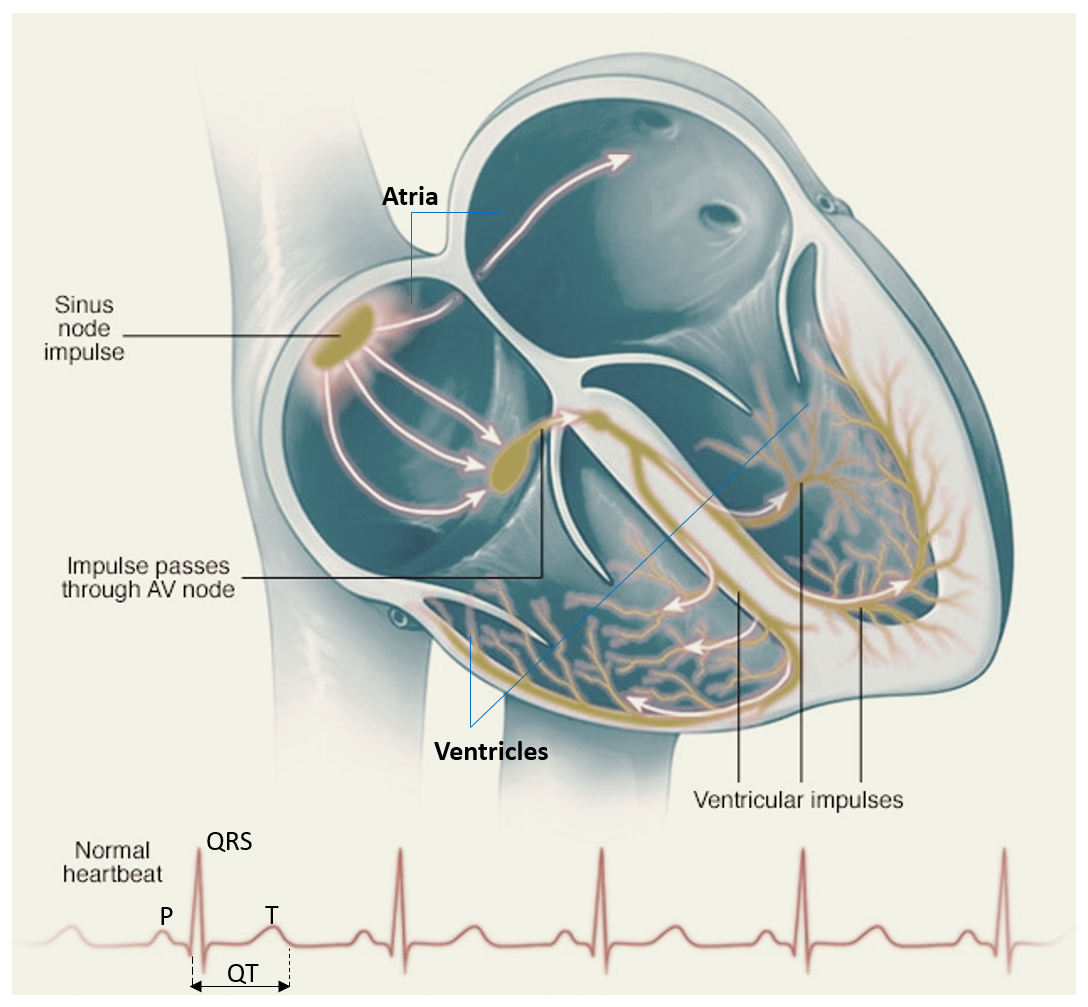
A normal heart rate is between 60-100 beats per minute. The normal heart has 4 chambers – right and left atria (upper chambers) and right and left ventricles (lower chambers). The heart has special cells (normal pacemaker of the heart) located in the ‘sinus node’ (SA node) of the right atrium which generates electrical impulses automatically at the rate of 60-100 beats per minute. These impulses are transmitted to the ventricles via the ‘atrioventricular node’ (AV node) located at the junction of the atria and ventricles.
A resting heart rate greater than 100 beats per minute is called tachycardia while a resting heart rate less than 60 beats a minute is called bradycardia. Not all tachycardias or bradycardias mean that one has heart disease. For example, during exercise, due to the increased need for oxygen by various body organs, it is normal to develop a fast heartbeat as the heart speeds up to meet this increased demand. During sleep or times of deep relaxation, it’s not unusual for the heartbeat to be slower.
Tachycardias in the atria
- Atrial fibrillation (AF): It is the rapid and irregular heart rate caused by irregular electrical impulses in the atria. These signals result in fast, uncoordinated, weak contractions of the atria. When such impulses are transmitted to the ventricles, it leads to fast and irregular heart-beats. AF can result in stroke (interruption of blood supply to a part of the brain), especially in the presence of other risk factors like high blood pressure, diabetes, heart failure, and advanced age.
- Atrial flutter: This is similar to atrial fibrillation except that in atrial flutter the heartbeats are less irregular and more organized. Atrial flutter may also lead to serious complications such as stroke.
- Paroxysmal Supraventricular tachycardia (PSVT): These are called paroxysmal since they come in paroxysms (suddenly and abruptly), and thereafter heartbeats become normal and regular. Patients usually complain of fast regular heartbeats which comes and ends suddenly. However, at times it may persist for longer periods requiring injectable medications for reversion to a normal heartbeat. These heart rhythm disorders are usually well tolerated by the patient and are very seldom life-threatening.
- Wolff-Parkinson-White syndrome: This is a type of supraventricular tachycardia, where there is an extra electrical pathway between the atria and the ventricles, which is present at birth itself. However, patients may not experience symptoms until adulthood. This pathway may allow electrical signals to pass between the atria and the ventricles without passing through the AV node, leading to short circuits and rapid heartbeats.
Tachycardias in the ventricles
- Ventricular tachycardia (VT): This is a rapid, regular heart rate that originates with abnormal electrical signals in the ventricles. The rapid heart rate doesn’t allow the ventricles to fill and contract efficiently to pump enough blood to the body. It may lead to a sudden fall in blood pressure and can be life-threatening if not treated on time. A VT developing in a person with poor heart function is a more serious condition when compared to a person with normal heart function.
- Ventricular fibrillation (VF): This occurs when rapid, irregular impulses in the ventricles lead to severe inefficiency of the ventricle to pump necessary blood to the body. This is a very serious problem and can cause death within minutes if not immediately treated. It is a common cause of sudden cardiac death. Most people who experience ventricular fibrillation have underlying heart disease.
- Long QT syndrome: This is a heart disorder that carries an increased risk of fast, irregular heartbeats. The rapid heartbeats, caused by changes in the electrical system of the heart, may lead to fainting and can be life-threatening. In some cases, it can cause sudden death. It can be congenital (a person born with a genetic abnormality) or acquired (certain medicines and drugs can cause long QT syndrome). Torsades de pointes is a specific form of rapid, irregular ventricular tachycardia with long QT, which can severely compromise the blood circulation, and be fatal. It may cease spontaneously or progress to ventricular fibrillation.
Bradycardia — A slow heartbeat
Although a heart rate below 60 beats a minute while at rest is considered bradycardia, a low resting heart rate doesn’t always signal a problem. If you’re physically fit, you may have an efficient heart capable of pumping an adequate supply of blood with fewer than 60 beats a minute at rest. Many athletes and marathon runners may have a low heart rate which may be absolutely normal.
Sick sinus syndrome
If your sinus (SA) node, which is responsible for setting the pace of your heart, isn’t sending impulses properly, your heart rate may alternate between too slow (bradycardia) and too fast (tachycardia). Sick sinus syndrome can also be caused by scarring near the sinus node that’s slowing, disrupting or blocking the travel of impulses. Sick sinus syndrome is most common among older adults though it can occur in young and middle-aged individuals also.
Conduction block
A block of your heart’s electrical pathways can occur in or near the AV node, which lies on the pathway between your atria and your ventricles. A block can also occur along other pathways to each ventricle.
Depending on the location and type of block, the impulses between the upper and lower halves of your heart may be slowed or blocked. If the signal is completely blocked, certain cells in the AV node or ventricles can generate a steady, although usually slower, heartbeat.
Some blocks may cause no signs or symptoms, and others may cause skipped beats or bradycardia.
Premature heartbeats
Although it often feels like a skipped heartbeat, a premature heartbeat is actually an extra beat (also called ectopic beats). Even though you may feel an occasional premature beat, it seldom means you have a more serious problem. Still, a premature beat can trigger a longer-lasting arrhythmia, especially in people with heart disease. Frequent premature beats that last for several years may lead to a weak heart. Premature heartbeats may occur when one is resting or may sometimes be caused by stress, strenuous exercise or stimulants, such as alcohol, caffeine or nicotine.
WHAT ARE THE KNOWN CAUSES AND RISK FACTORS FOR HEART RHYTHM DISORDERS?
Some of the causes and known risk factors for arrhythmias include:
- Aging
- Thyroid disorders
- Heart conditions like heart attack, heart failure, heart infections, weak heart, blocked arteries of the heart or scarring of part of the heart due to previous a heart attack
- High blood pressure
- Diabetes
- Sleep apnea (a sleep disorder commonly present in obese individuals or ones with abnormal airways where there are frequent snoring and episodes of breathing pauses at night leading to increased risk of heart rhythm disorders, cardiovascular disease and high blood pressure)
- Stress and Anxiety
- Smoking
- Excess alcohol and coffee intake
- Drug abuse
- Certain prescribed medications including antibiotics, antidepressants/antipsychotics, over-the-counter cold and allergy drugs, and so-called health supplements.
- Electrolyte disturbances such as too high or low levels of potassium, sodium, calcium and magnesium
Note- COVID-19 infection can also cause heart rhythm disorders.
WHAT ARE THE COMMON SIGNS AND SYMPTOMS OF HEART RHYTHM DISORDERS?
Heart rhythm disorders at times may not cause any signs or symptoms. They may be incidentally detected on examination by a doctor or on the ECG.
The symptoms can be varied at times including:
- a feeling of a missed beat
- palpitations (a sensation that the heart is racing, fluttering or skipping a beat)
- shortness of breath
- pounding of heart
- loss of consciousness or fainting
- giddiness and lightheadedness
- excessive tiredness or fatigue
- anxiety and sweating
HOW ARE HEART RHYTHM DISORDERS DIAGNOSED?
A good clinical evaluation including a detailed history and physical examination is the key to a diagnosis of heart rhythm disorders. A 12-lead ECG is required in all cases. A 24-hour ECG monitoring (Holter test) may be advised. Further tests may include echocardiography to assess the heart function, and valvular structures of the heart, are also recommended. In addition, basic blood tests including thyroid function tests and electrolytes are also ordered.
In some patients recording of the heartbeats for a longer period of time (days to months) may be required using external loop recorders or implantable loop recorders. In cases where a clear-cut diagnosis cannot be established despite the above tests, electrophysiology studies of heart rhythm disorders may be required in the cardiac catheterization laboratory.
WHAT ARE THE TREATMENT MODALITIES AVAILABLE FOR THE TREATMENT OF HEART RHYTHM DISORDERS?
Antiarrhythmic drugs under the supervision of a cardiologist may be required in patients especially for tachycardia (fast) heart rhythm disorders. Patients with atrial fibrillation and flutter are at high risk of stroke and they may require anticoagulant medications (blood thinners) after assessment of their risk profile by a specialist.
Permanent pacemaker implants may be required for patients with heart blocks and those with bradycardia (slow heart rate) disorders. Pacemakers are implanted via a small surgery in the chest in which leads are placed in the heart chambers and connected to a battery (pulse generator). The battery gives electric supply which is transmitted to the heart by the leads during the times when the heart rate becomes low.
Certain devices like AICD (Automated Implantable Cardioverter Defibrillators) may be required to prevent sudden cardiac death arising from fast and unstable heart rhythm disorders like ventricular tachycardia (VT) and ventricular fibrillation (VF). These devices are implanted like a pacemaker device. They have algorithms like anti-tachycardia pacing and defibrillation and can give internal shocks to stop life-threatening arrhythmias like VT and VF.
Some tachycardic disorders like PSVT and scar VT may respond to catheter ablation procedures, which are procedure done in the cardiac catheterization laboratory by specialists, for by breaking abnormal circuits in the heart or destroying areas of the heart muscle that are triggering arrhythmias.
Dr Samir Kubba, MD, DNB (Medicine), MNAMS, DM (Cardiology) is a Fellow of the American College of Cardiology (FACC), Society for Coronary Angiography and Interventions (FSCAI), and the European Society of Cardiology (FESC). He is the Director and Unit Head, Cardiology at Dharamshila Narayana Superspeciality Hospital, Delhi. He is well acclaimed for both his clinical experience and academic contribution, and is a well-known speaker at medical forums, with several medical peer-reviewed publications. He is also an accomplished player of the guitar and keyboards, and as a doctor emphasizes the importance of pursuing hobbies to help manage stress and improve health.
Also read by Dr Kubba:
Post-COVID Cardiovascular Effects – Know the 3 Types and Management
Other useful reads:
Inflammation of Heart Layers (Carditis) – Pericarditis, Myocarditis, Endocarditis
High Blood Pressure (BP) – Risks and Solutions for Hypertension