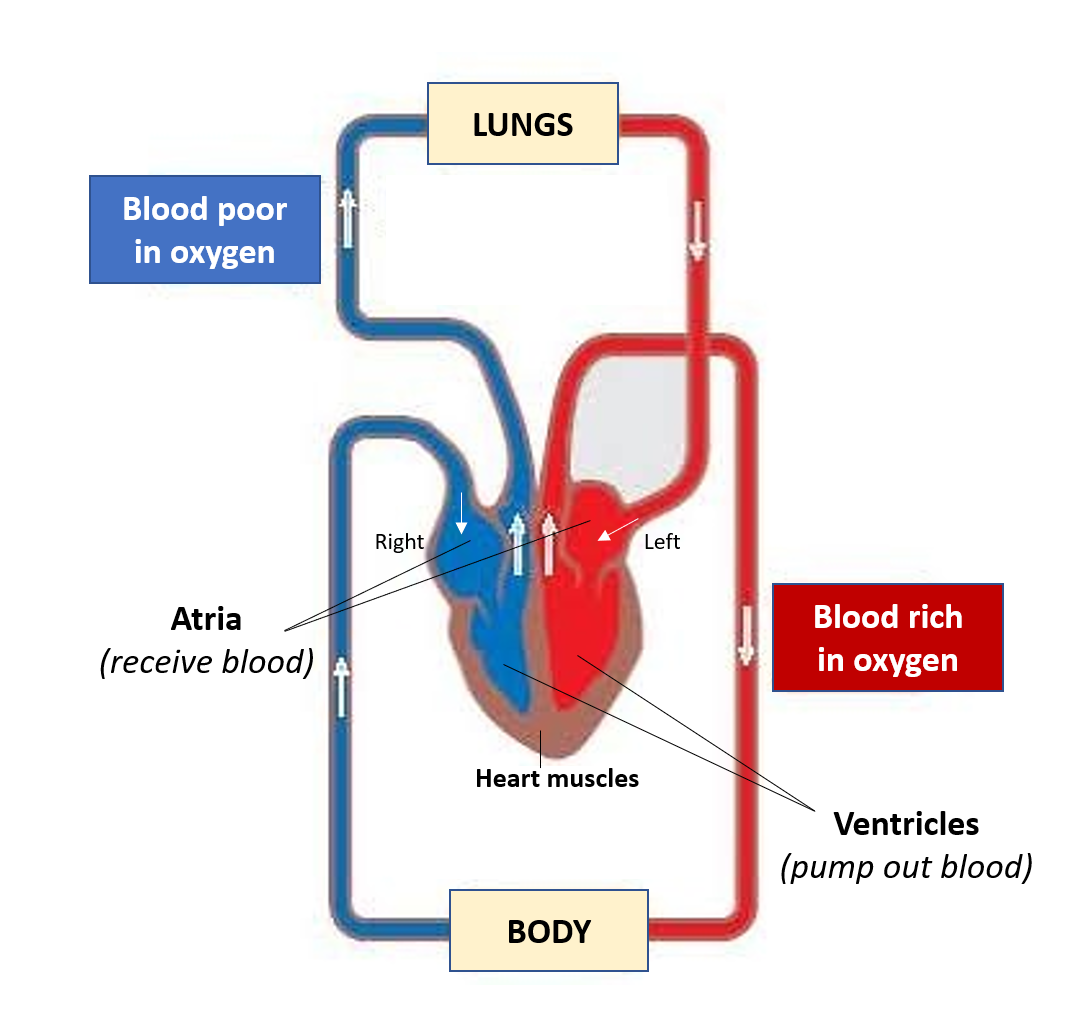
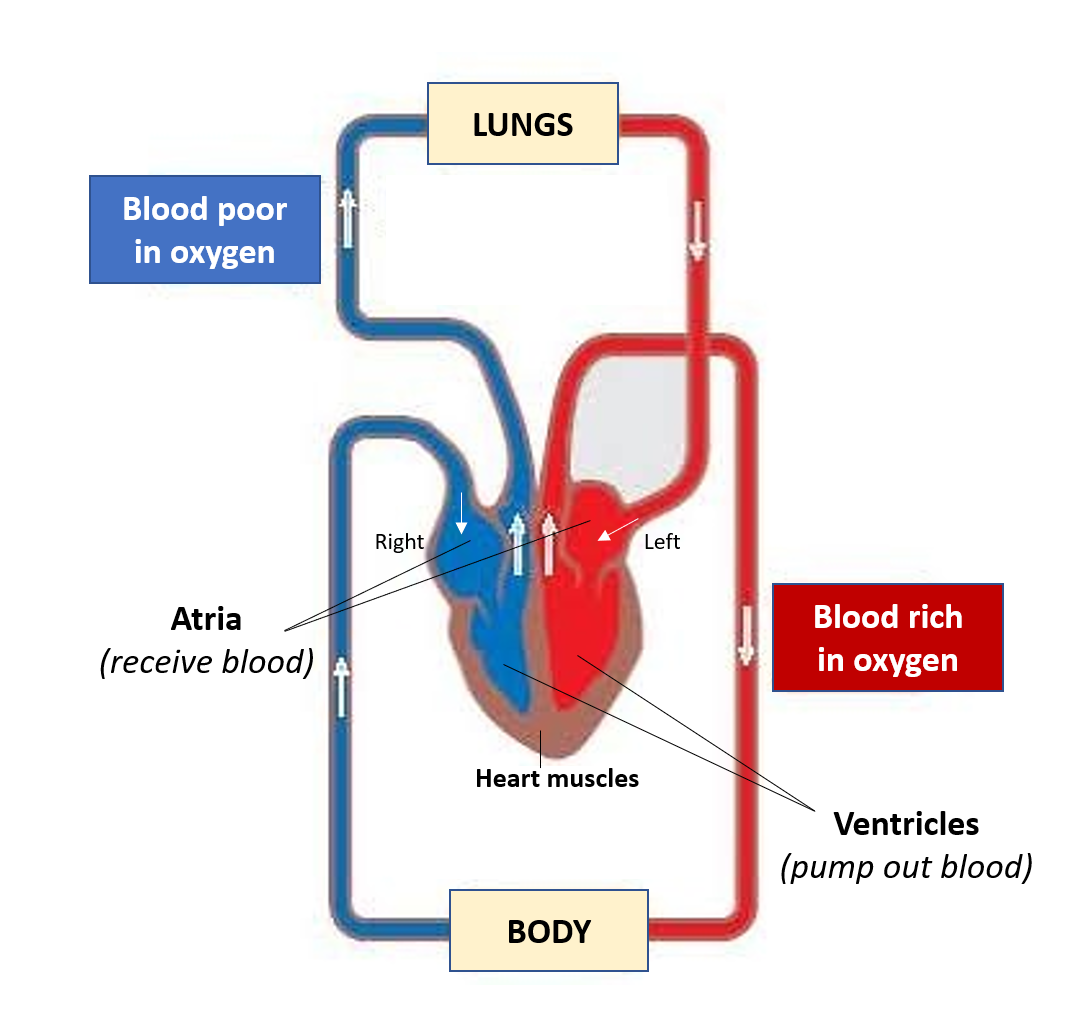
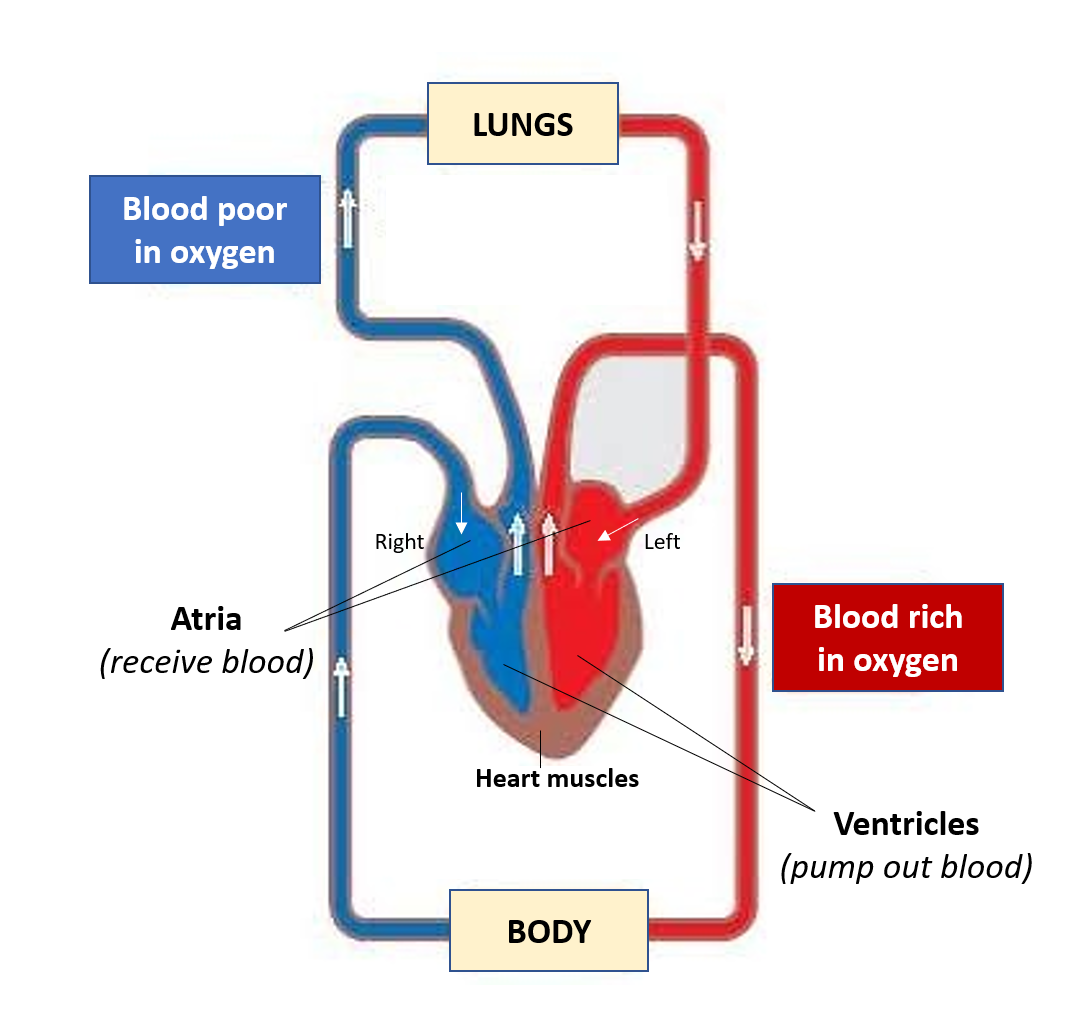
Our heart works tirelessly and quietly round the clock, so evidently if it gets ill in any way, the health impact can be serious and significant. Even though the cardiac chambers (atria and ventricles) are filled with blood, the cardiac muscles (myocardium) require blood supply and oxygen (provided by coronary arteries), to effectively contract and pump the blood to the entire body.
A lot of terms associated with heart (cardiac) conditions are used in common parlance but it is useful to be aware of what these terms really mean.
ATHEROSCLEROSIS
Atherosclerosis (Arteriosclerosis) refers to the buildup or formation of plaques in the blood vessels called arteries which carry oxygen-rich blood to all the body organs. These plaques (also called atheroma) are made up of fats, cholesterol, calcium, and some blood cells mainly platelets. These occur due to damage to the artery wall (endothelium) due to high blood pressure, high sugar (diabetes), smoking, and high LDL-cholesterol/triglycerides. These plaques can cause partial blockage and stiffening of the arteries, and sometimes a sudden complete blockage due to the plaque rupturing and causing clot formation (thrombosis).
CARDIOVASCULAR DISEASE (CVD)
Cardiovascular disease refers to a group of conditions occurring due to blockage of blood vessels more specifically arteries (coronary artery disease-CAD) due to atherosclerosis and clots, and its resulting impact (that can cause angina and heart attack) and other organs (stroke, peripheral artery disease). CVD is also known as atherosclerotic cardiovascular disease (ASCVD).
Read:
Cardiovascular Disease (CVD) – Understanding Atherosclerosis and Coronary Artery Disease
HEART FAILURE (HF)
It is also called Congestive Cardiac Failure (CCF/CHF) occurs when the heart is unable to pump adequate blood into the arteries, and the backlog of blood leads to congestion and backpressure into the lungs and the veins.
Read:
Sometimes defects may be present from birth (Congenital Heart Defects) and can also progress to cardiac failure.
CARDIAC ARREST
Cardiac arrest implies that the heart has stopped pumping blood. A related word is sudden cardiac death (SCD).
Cardiac arrest is the sudden stopping of heart function, revivable by CPR and/or defibrillation, while SCD is a subset of cardiac arrest that results in death, usually within an hour of symptom onset, or 24 hours from last being seen healthy. Essentially, SCD is a cardiac arrest from which a patient could not be revived, and which caused death.
One should perform CPR (Cardio-Pulmonary Resuscitation) which should be ideally initiated within 2-5 minutes in a person with cardiac arrest. This can help restart the cardiac pumping action and revive the patient while emergency services are on their way. After 6-8 minutes, permanent brain damage is inevitable with patients often going into a coma. After 10 minutes, the chances of survival are extremely low.
Cardiac arrest is always the final cause of death in patients with cardiac diseases like myocardial infarction, heart failure or electric rhythm disturbances. It is also the ultimate cause of death in drowning, electrocution, poisoning/drug overdose, as well as massive – injuries, blood loss, and infections (causing shock).
Often in conversations, the words heart attack, cardiac arrest, and heart failure are used interchangeably, but the awareness that they refer to three different clinical situations is important. Also, a heart attack can be the cause of heart failure which eventually causes cardiac arrest, or a massive heart attack can be the direct cause of cardiac arrest, which is the final cause of death.
Also read –
High Blood Pressure (BP) – Risks and Solutions for Hypertension
Diabetes: Understanding health risks, treatment, and taking effective diet-lifestyle measures
Inflammation of Heart Layers (Carditis) – Pericarditis, Myocarditis, Endocarditis
Post-COVID Cardiovascular Effects – Know the 3 Types and Management
For any query, additional information or to discuss any case, write to info@drvarsha.com and be assured of a response soon
References
2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease


