Pneumonia is something we hear of commonly and it can be concerning or serious, thereby requiring the right awareness and timely action.
UNDERSTANDING IMPORTANT TERMS
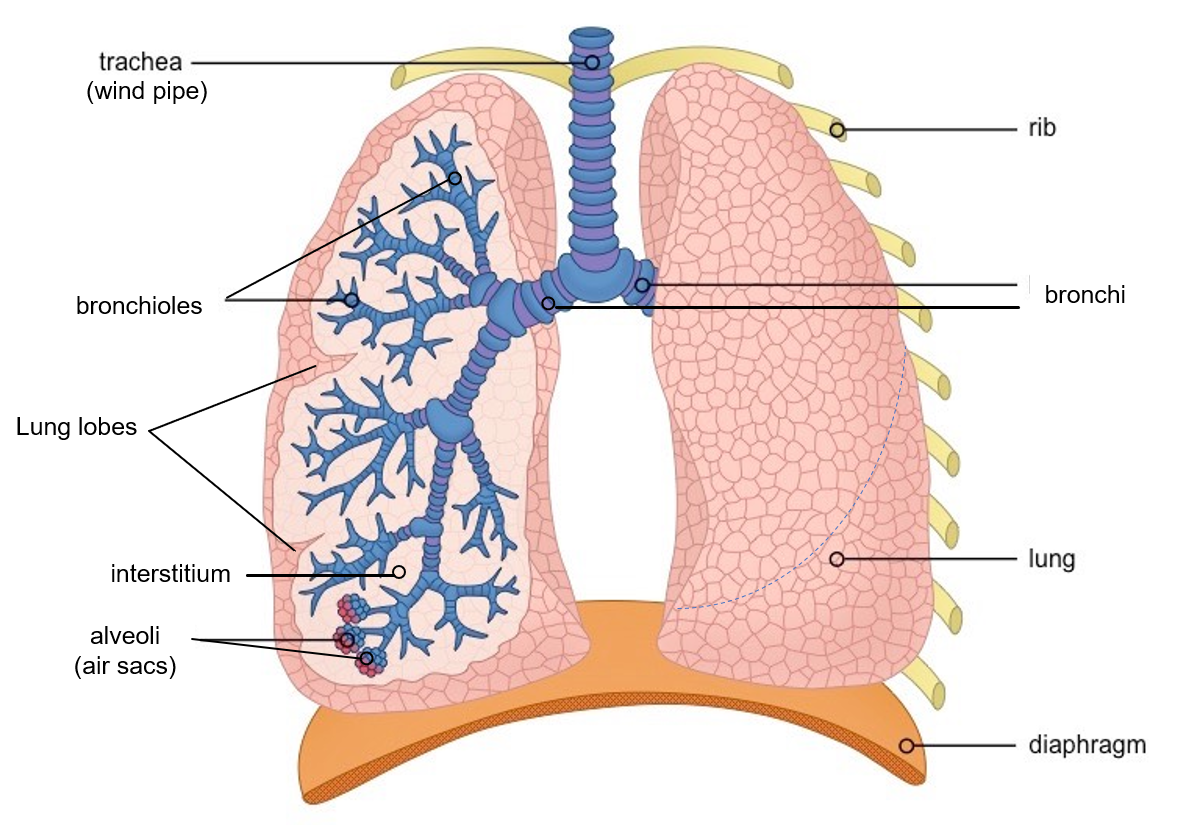
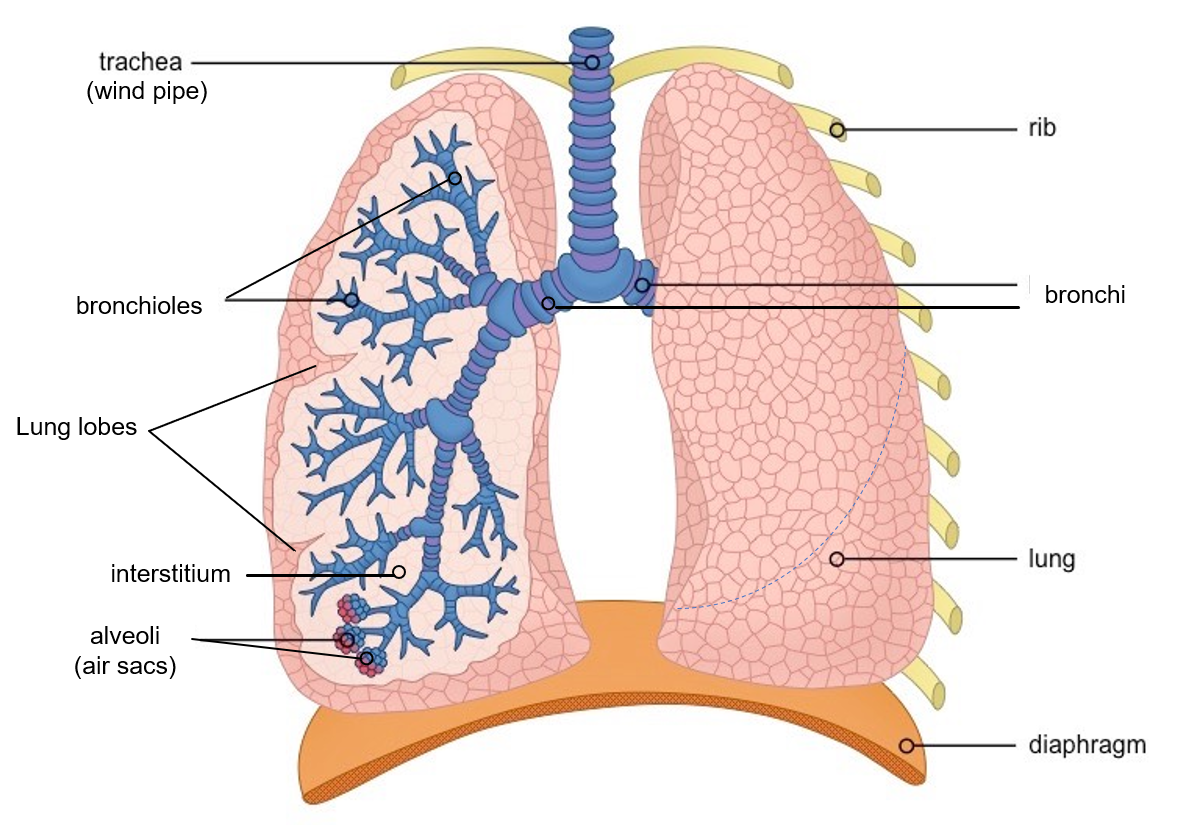
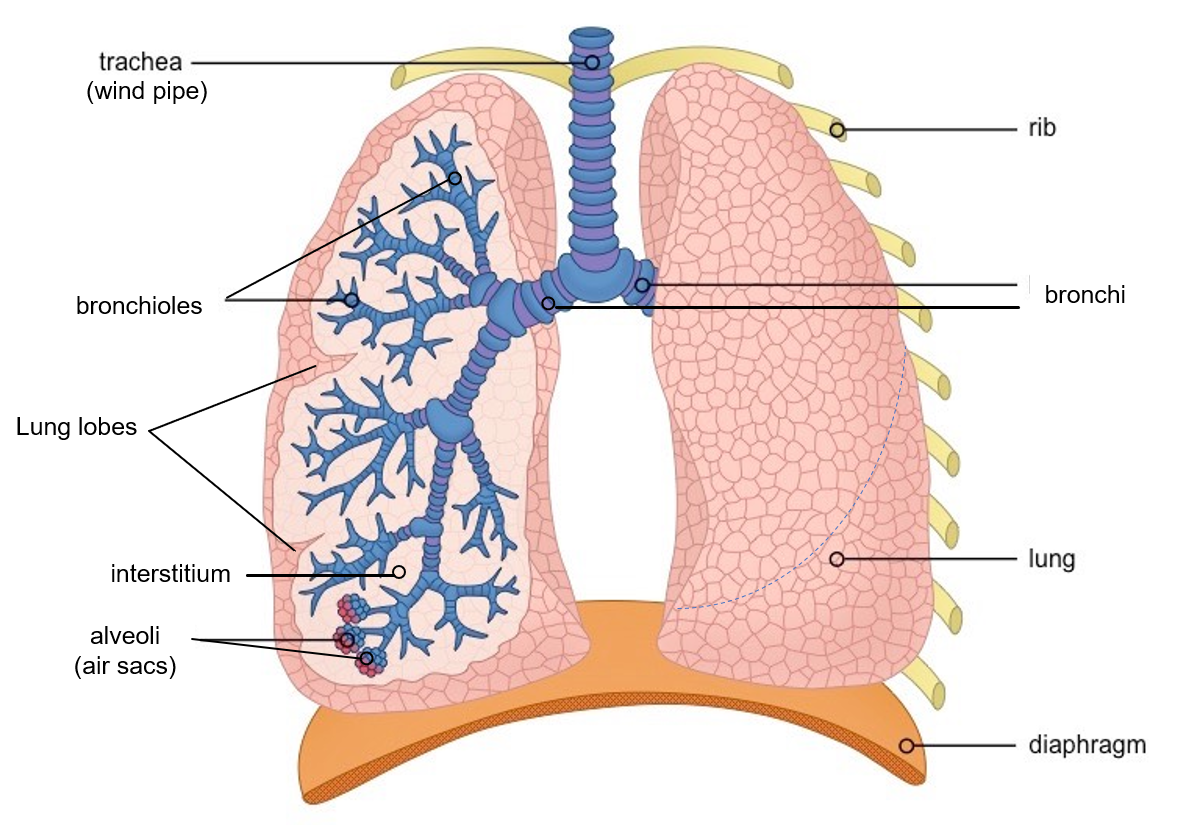
The term pneumonia (pneumon – lung) is actually a broad term that means inflammation of the lung, however, in usual medical terms and common language, it implies inflammation of the air sacs (alveoli) of the lungs due to infection (bacterial, viral or fungal).
The term pneumonitis also means inflammation of the lung, therefore technically pneumonia is a type of pneumonitis. However, in common medical terms, pneumonitis implies inflammation of the air sacs of the lungs due to irritant/toxic substances, or allergic/hypersensitivity reactions to certain bacteria, fungi (molds) or other substances.
So, when we say pneumonia alone, it is taken as the infection of the lung air sacs (alveoli).
There is also the term interstitial pneumonia, which means inflammation of the interstitium (the region between the air sacs) of the lung. These can be of several types due to different causes and come under the umbrella of the group of conditions called interstitial lung disease (ILD).
PNEUMONIA
In pneumonia, the infection and inflammation can cause the air sacs to swell up and get filled with fluid or pus. This can decrease the effective gaseous exchange of oxygen and carbon dioxide that occurs here. Pneumonia generally refers to community-acquired pneumonia (CAP), while other specific nomenclatures are mentioned below.
Who is at risk?
- Newborns (neonates), infants, and children, due to the easy spread of infections from the upper airway to the lungs resulting from a shorter airway and underdeveloped immunity.
- Elderly, (especially 65 years and above), due to waning immunity as well as weaker and more damaged lungs as a result of age and a long period of exposure to environmental irritants.
- Smokers and those with respiratory conditions like chronic obstructive pulmonary disease (COPD/ chronic bronchitis) and asthma, or cystic fibrosis (CF- a rare genetic inherited disorder that leads to the production of thick and sticky mucus that plugs the airways and greatly increases the frequency and severity of respiratory infections).
- Comorbid conditions like diabetes, heart failure, and compromised kidney or liver function.
- Decreased immunity like with HIV, post transplants, cancers, hemoglobin abnormalities, spleen removal, etc, or prolonged exposure to antibiotics, corticosteroids, or other immune-suppressive drugs and anticancer chemotherapy/radiotherapy.
- Malnutrition, crowded living conditions, chronic illnesses, and alcohol abuse.
- Hospitalized patients and those intubated or on a ventilator are high-risk groups for pneumonia with opportunistic and resistant organisms, and the pneumonia is designated hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP) respectively.
- Aspiration (mouth or stomach contents entering lungs) can cause pneumonia (aspiration pneumonia) especially in people with decreased consciousness (like due to alcohol abuse), swallowing problems, poor oral hygiene and those on tube feeds.
CAUSATIVE ORGANISMS
Majority of pneumonia especially CAP is caused by bacteria or viruses, while rarely fungi and parasites can also be the cause.
Bacteria
Among bacteria, Streptococcus pneumoniae (Pneumococcus) is the most common bacteria. Other less common ones include Haemophilus influenzae, Staphylococcus aureus, and atypical bacteria like Chlamydia pneumoniae (common in household/institutional outbreaks in children and younger adults), Mycoplasma pneumoniae and Legionella pneumoniae.
In the newborn (neonates), bacteria causing pneumonia include group B Streptococcus, Listeria monocytogenes, or gram-negative rods (E coli, Klebsiella pneumoniae).
Bacteria like Pseudomonas aeruginosa and Acinetobacter baumanii can cause severe pneumonia in immune-compromised or hospitalized patients.
Psittacosis (parrot fever or ornithosis) is a rare cause of pneumonia caused by the bacterium Chlamydia psittaci and contracted from infected parrots and other birds like pigeons, sparrows, hens, macaws and ducks.
Anaerobic bacteria (those that can survive without oxygen) which frequently cause oro-dental infections, can be the cause of aspiration pneumonia.
Viruses
Coronavirus (SARS CoV 2) causing COVID, and Influenza (Flu) virus have emerged as important causes of pneumonia especially during pandemics/epidemics. Other viruses, some of which are also associated with the common cold, can sometimes cause pneumonia, like respiratory syncytial virus (RSV), adenovirus, rhinovirus and parainfluenza virus.
A preceding upper respiratory infection like a cold with dry cough before onset of pneumonia symptoms may suggest a viral cause. Viral infections also increase the risk of secondary bacterial pneumonia.
Fungi
Fungi can more commonly be a cause of pneumonia in people exposed to and inhaling spores in fields, soil, and bird/bat droppings like seen in the countryside, farms and rural areas. Histoplasma, Coccidioides (valley fever) and less commonly Blastomyces and Paracoccidioides are known causative fungi.
Fungal infections are also known in those with compromised immunity like in HIV-AIDS, or those on immune-suppressive treatment for cancer or transplants. Pneumocystis, Cryptococcus and rarely Candida are the causatives here. Aspergillus is a fungus that can cause invasive pneumonia especially in people with weakened immunity and pre-existing respiratory conditions.
Parasites
Rarely parasites/worms can also cause pneumonia especially in those with compromised immunity.
SYMPTOMS AND SIGNS
- Fever sometimes with chills (temperature can be normal or even low in elderly or immune-compromised people)
- Fatigue, weakness, muscle aches and headaches
- Cough (usually dry in viral, and with phlegm in bacterial)
- Chest pain (usually present in the region of underlying infection, and aggravated by coughing)
- Shortness of breath (usually on exertion, not at rest)
- Rapid shallow breathing (tachypnea)
- Nausea, vomiting, inability to feed, and diarrhea (sometimes)
- Irritability and restlessness, or sometimes lethargy (seen in infants)
- Bluish discoloration of the skin, lips/tongue (cyanosis – seen more in infants)
- Disorientation and confusion (more in the elderly)
DIAGNOSIS
A well-taken history can help in both diagnosing pneumonia and its type.
On chest examination, crackling sounds (crepitations) and high-pitched loud breath sounds (bronchial breathing) may be audible to the doctor on chest examination with a stethoscope. ‘E’ sound may sound like ‘A’ when heard on the stethoscope (known as egophony- increased resonance of the voice due to preferred transmission of high frequency sounds through fluid).
The investigations ordered will usually include the following:
Blood tests
These include complete blood counts and blood urea nitrogen BUN, creatinine.
Chest X-ray
X-ray may reveal haziness of the lungs, due to infiltrates and consolidation (air being replaced by fluid/pus).
Based on infection patterns observed and parts of the lung involved, pneumonia is called-
- lobar or multilobar (affecting a specific lobe or multiple lobes of the lung respectively)
- bronchopneumonia (involving lower end of bronchioles and lung air sacs around it).
High-resolution computerized tomography (HR-CT)
This is the imaging test recommended especially if clinical suspicion is high and X-ray and other tests are inconclusive.
A CT severity score out of 25 is sometimes given based on the lung involvement seen. Each lobe (3 right and 2 left) could be awarded a CT score from 0 to 5, depending on the percentage of the involved lobe: score 0 (no involvement)
- score 1 (<5% involvement)
- score 2 (5-25% involvement)
- score 3 (26-49% involvement)
- score 4 (50-75% involvement)
- score 5 (>75% involvement)
A score of 7 or less signifies mild, 8-17 moderate, and 18 or above signifies severe pneumonia respectively.
Other tests
Pulse oximetry is done to check blood oxygen saturation, and sometimes an arterial blood gas analysis may be ordered.
Specific antigen tests for pneumococcus, COVID and influenza are also performed.
Sputum samples for testing are sometimes taken (collected after a deep cough or saline nebulization).
In hospitalized patients, a bronchoscopy for procuring a sputum sample from the bronchi (broncho-alveolar lavage BAL) for testing, and a blood culture to look for possible spread of infection in the bloodstream (septicemia), are also performed.
MANAGEMENT
Pneumonia can be treated by outpatient visits, however severe cases with breathing difficulty, and reduced oxygen saturation should be hospitalized for oxygen therapy or ventilator support in ICU.
Babies in the first 2-3 months of life, children who are unable to feed orally and appear dehydrated or have breathing difficulty, as well as elderly patients especially those with associated comorbidities like diabetes, compromised heart, kidney, liver, or immune function, and pre-existing respiratory conditions should also be preferably hospitalized for closer monitoring.
The CURB-65, criteria is useful for decision making where 1 point is allotted for each of the following risk factors:
- Confusion
- Uremia (BUN ≥19 mg/dL) indicating declining kidney function
- Respiratory rate > 30 breaths/minute
- Blood pressure < 90 mm Hg systolic or ≤ 60 mm Hg diastolic
- Age ≥ 65 years.
The score signifies the following-
- <2 points: mortality risk is very low, and out-patient treatment is appropriate
- 2 points: mortality risk is almost 10% so hospitalization is recommended
- ≥ 3 points: mortality risk is 15 to 40% and strongly indicates hospitalization and consideration of intensive care
Treatment
Supportive care includes fluids and maintaining hydration, medicines for reducing fever and pain (antipyretics-analgesics), and phlegm/mucus (mucolytics-mucoregulators).
Antibiotics are the mainstay of treatment. It is not only difficult to differentiate viral from bacterial pneumonia in many cases but also viral pneumonia increases the chances of secondary bacterial pneumonia. Therefore, antibiotics are given in all cases. Antibiotic combinations from different classes may be used. The common ones include ampicillin/amoxicillin, 3rd generation cephalosporins (like ceftriaxone, cefotaxime), macrolides (like azithromycin), fluoroquinolones (like levofloxacin), and in resistant infections, reserve ones like clindamycin, meropenem and vancomycin.
Specific antiviral agents for Influenza including oseltamivir, zanamivir, baloxavir and favipiravir are approved and used in several countries. In 2020, several repurposed medicines have been authorized for use in COVID. Antifungal and antiparasitic drugs are given when such organisms are suspected/involved.
Other medicines considered in severe/hospitalized cases are corticosteroids to reduce inflammation, and drugs to decrease the risk of thrombosis.
Oxygen therapy and ventilator support is given in all severe hospitalized cases. Extracorporeal membrane oxygenation (ECMO) is a technique where blood is pumped outside the body to a heart-lung machine that removes carbon dioxide and sends oxygen-filled rewarmed blood back to the body. This is a bypass method to decrease the load on the heart and lungs thereby aiding earlier recovery.
COMPLICATIONS
Pneumonia may cause pleural effusion which is fluid or pus within the lining cover of the lung (pleura), or an abscess (pus trapped in a lung cavity). These may sometimes require drainage with needle/tube in case of non-resolution with conservative treatment.
The cause of death in pneumonia is usually respiratory failure due to extensive lung damage and reduction in blood oxygen, or due to the spread of infection in the blood (septicemia) causing multi-organ failure.
VACCINES
Vaccines are available to protect against the bacteria Pneumococcus (PCV-13 and PPSV-23), and Hemophilus influenza type B (Hib). PCV-13 and Hib are given to infants and children under 5 years of age as part of the immunization program in most countries. Older children and adults with risk factors mentioned above especially comorbid conditions and reduced immunity, and those aged 65 years or more, should also get the PPSV23 pneumococcal vaccine.
Influenza vaccine is to be taken annually and should be given to children, the elderly, and those with respiratory and other comorbid and immunocompromised high-risk conditions mentioned.
COVID vaccines have been introduced for in 2020-21 due to the pandemic.
Also read-
Common Cold and Flu- Know the difference, effective care and 10 alert signs
Interstitial Lung Disease (ILD) – Types, Risks, and Health Measures
Reference- Pneumonia manuals
For any query, additional information or to discuss any case, write to info@drvarsha.com, or leave a message in box below, and be assured of a response soon.