A cough is a protective and a physiological response or reflex that involves rapid and forceful expulsion of air from the respiratory tract through the mouth to help remove irritants and excessive mucus from our airways.
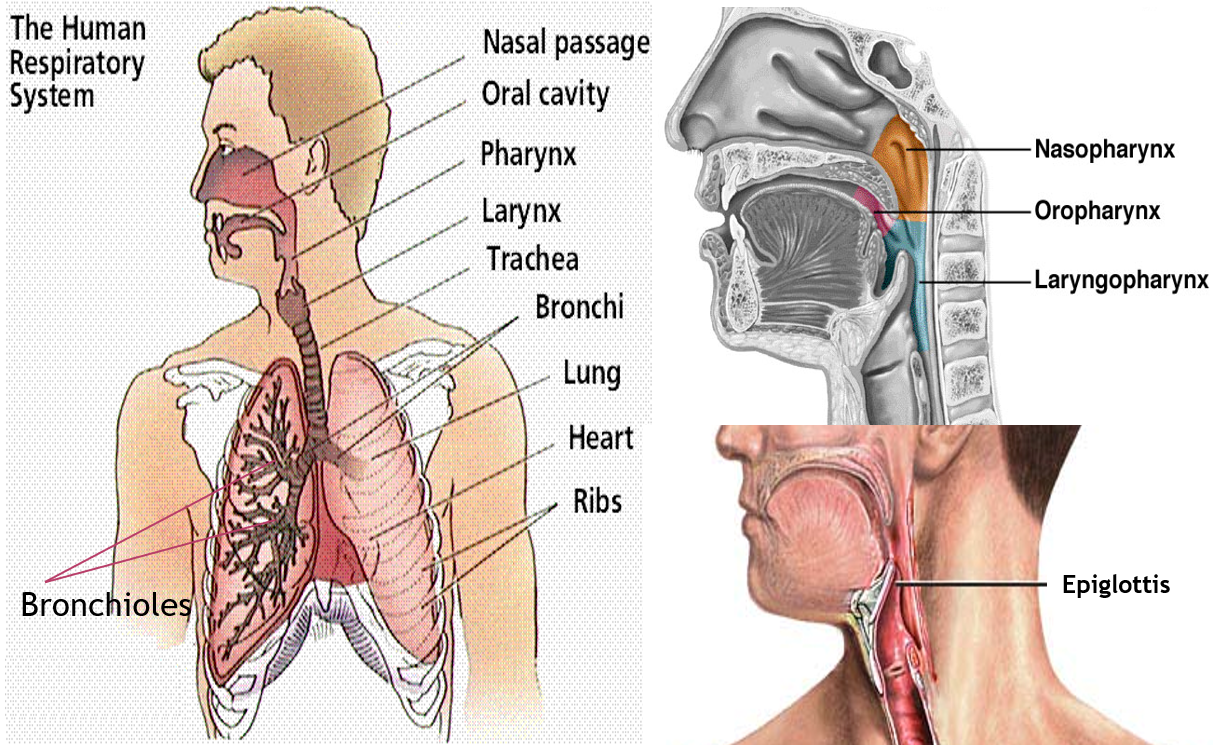
AIRWAY STRUCTURE
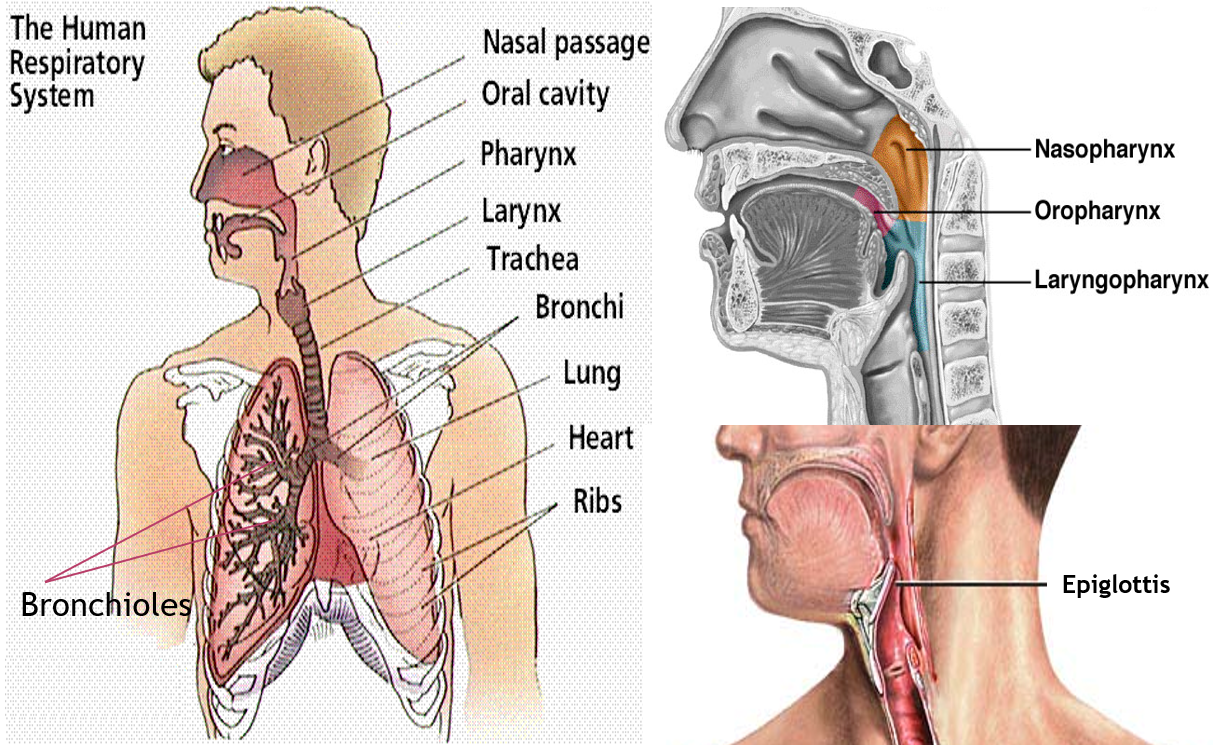
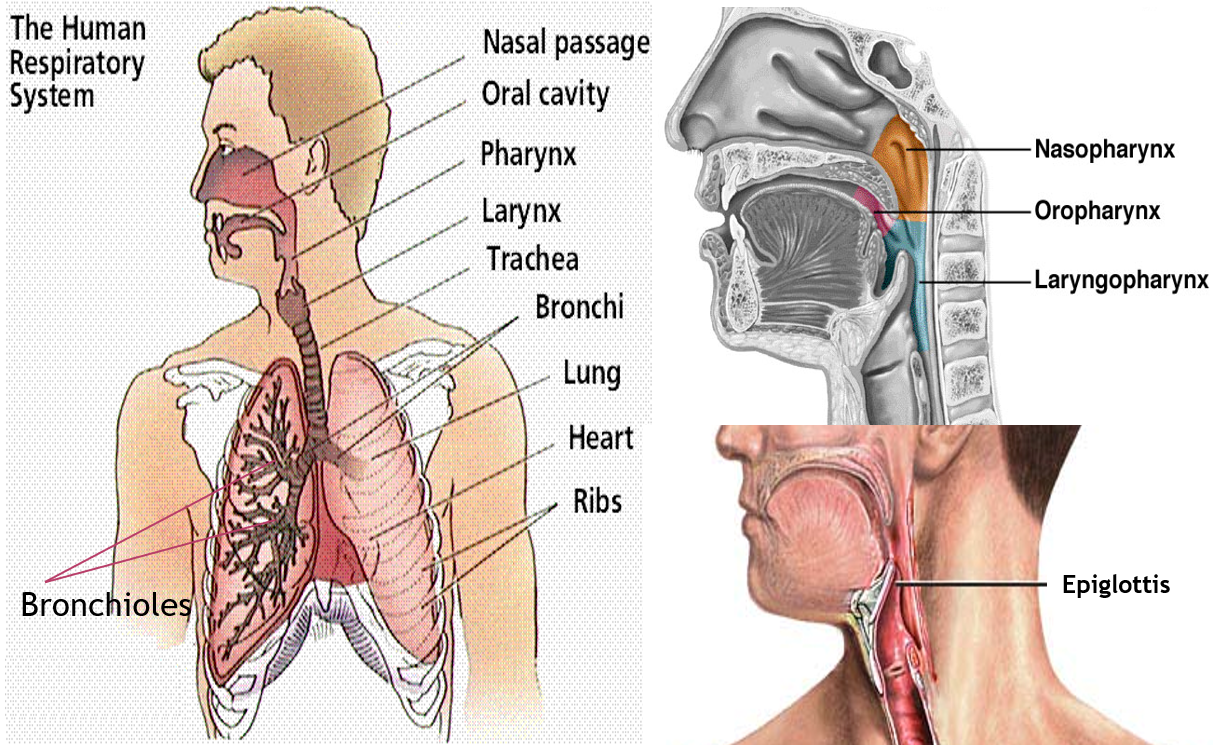
An important part of our respiratory tract (airway) is the pharynx (the throat) that connects to the back of the nose (nasopharynx), back of the mouth (oropharynx), and then proceeds into the larynx (laryngopharynx). The junction of the throat (pharynx) and voice box (larynx) is guarded by a lid like structure called epiglottis, that is open during speaking and closed while eating, to prevent food from entering the airway.
The larynx leads into the trachea (wind-pipe) that branches into 2 bronchi (one for each lung). The bronchi branch into smaller bronchioles that end in the air sacs (alveoli) of the lungs where gaseous exchange takes place.
The airway is lined by thread like structures called cilia, and protected by a layer of mucus. The cilia have a broom-sweeping action that help regularly clear excess mucus or foreign particles, irritant, pathogens etc. from the airways, and prevent entry into the lungs. Sputum a mixture of saliva and mucus coughed up from the respiratory tract.
The airway is also lined by ‘receptors’ that are sensors connected via nerves to the central nervous system (spinal cord and brain).
MECHANISM OF COUGH
There are two types of receptors in the respiratory tract. The mechanoceptors are stimulated by irritants, dust or other foreign particles, pathogens, inflammatory mediators (like histamine, bradykinin, etc.), and by changes in airflow (or diameter of the airway – constriction). The chemoreceptors are stimulated by chemicals and their odors.
Once these airway receptors are stimulated, they trigger and electrical impulse, carried by the nerves to the spinal cord, and then the ‘cough center’ in the brain which processes the information and sends back responses to the muscles of the airway (throat and chest), abdomen and diaphragm, to initiate the cough and forcefully expel the air and irritants from the airway through the mouth.
TYPES OF COUGH
Cough that lasts for less than 3 weeks is said to be acute, beyond which it is said to be chronic. Some physicians recognize a period of 3-8 weeks as subacute cough, and beyond that call it chronic.
Cough is usually classified depending on its nature, as dry or wet.
Dry cough
It does not express or contain much mucus (phlegm), and is due to persistent airway irritation. It is hacking and scratchy in nature, and can cause lot of fatigue and strain. It is commonly seen part of common cold and flu, COVID, airway allergy, sore throat due to upper respiratory infections (pharyngitis, laryngitis, tonsillitis), and post-viral cough, acid reflux disease (GERD), and initial stages of pneumonia and tuberculosis (TB).
Some medicines like ACE inhibitors used to treat high BP, can also cause dry cough by increasing some inflammatory mediators in the airway. Rarely, persistent cough maybe one of the presenting symptoms of lung cancer, especially when associated with coughing up blood (hemoptysis).
Such cough therefore needs to be suppressed (by cough suppressant or anti-tussive agents), as it can be very disturbing to the person interfering with daily activities and sleep, and also detrimental to those in post-surgical care or with conditions like hernia.
Wet cough
It is associated with plenty of mucus (phlegm) and occurs with the purpose of expressing and bringing out the mucus. This is commonly seen in smokers, lower respiratory tract infections (bronchitis, bronchiolitis), chronic obstructive pulmonary disease (COPD), bronchiectasis, and later stages of pneumonia and TB.
Such cough should be assisted with agents that help break and thin down the mucus (mucolytics) and help express the mucus (expectorants). Sometimes adding a low dose of a bronchodilator, helps to further ease out the expression of mucus.
Bronchospastic cough
It refers to a cough associated with bronchoconstriction (narrowing of the lower airway). It can be dry as seen in asthma, or wet as seen in acute bronchitis or episodes of worsening of chronic bronchitis or COPD (AECB – acute exacerbation of chronic bronchitis).
This will need to be treated with bronchodilators in addition to anti-tussive or mucolytic-expectorants, depending on the presence of phlegm.
Cardiac cough
It occurs due to heart failure, and build up of fluid in the lungs. It is usually wet in nature, with the sputum being frothy, and sometimes blood tinged.
MANAMEMENT OF COUGH
It is important to understand that cough in itself is a protective mechanism, and a symptom. It needs to be treated only if it is causing distress and fatigue, interfering with sleep and daily activities, or worsening some other condition or hampering recovery. Medical preparations are available most commonly as syrups, but also as teas, lozenges and tablets.
Natural soothing agents are most suitable for dry cough as it occurs mainly due to persistent airway irritation. These include warm fluids and preparations containing tulsi (Indian basil), turmeric (curcumin), (jeshthmadhu) liquorice, honey, ginger, and mint (menthol). Use of a humidifier or a saline spray/gargle, can also help moisten and sooth the throat.
Cough suppressants are used for dry cough that is interfering, distressing, and needs to be suppressed. These are of two types:
Centrally acting: These act by suppressing cough center in the brain. They include opioid agents like codeine, and non-opioid agents like dextromethorphan. Codeine though very effective, is known to cause dependence and constipation, therefore most market preparations of cough syrups contain dextromethorphan.
Peripherally acting: These act at the level of the airway by reducing inflammatory mediators and the stimulation of cough receptors. This includes levodropropizine and levocloperastine, the latter having both central and peripheral action. Medicines called ‘antihistamines’ used for common cold and allergy, may also contribute to reducing peripheral airway irritation.
Mucoregulators are medicines that act on the excessive mucus or phlegm seen in wet cough. They include mucolytic agents that break down the mucus and make it thinner and easier to express, and expectorants that increase mucus volume by making it dilute, and help in the ciliary action (mucokinetic action) to bring out the mucus more easily. Mucolytic agents include ambroxol, acebrophylline, bromhexine, N-acetyl cysteine (NAC), and carboxymethyl cysteine (CMC), while expectorants include guaiphenesin and ammonium chloride.
Bronchodilators are agents that relax the involuntary muscles of the lower airway (bronchi/bronchioles) and help to dilate the airway, making both breathing and expression of phlegm easier. They are used mainly for bronchospastic cough, and in a lower dose for wet cough. These include salbutamol, levosalbutamol, and terbutaline.
Treating underlying and associated conditions
A cold may be associated, presenting with sneezing, running nose or nasal congestion. In such cases, antihistamines, and decongestants orally or nasally may be given.
Most acute dry cough is due to upper respiratory tract infections that are commonly viral, and resolve on their own. However, if throat pain, or pain on swallowing is prominent, and mouth-throat examination suggests a bacterial infection, then antibiotics may also be prescribed.
Additional symptoms like fever, chest pain, body ache, weight loss, weakness, and breathlessness should always be enquired for. High fever, with chest pain, and/or breathlessness can be suggestive of pneumonia. Flu and COVID should be ruled out if seasonal outbreaks are ongoing. Presence of fever or body ache may necessitate prescribing paracetamol.
Presence of episodes of breathlessness or wheezing with dry cough especially in the early morning (2-4 am), should be evaluated for asthma. Any cough lasting more than 3 weeks should raise suspicion for tuberculosis especially in India. Gastro-esophageal reflux disease (GERD) is often the cause of a chronic dry cough, that often worsens on lying down, and should be evaluated for. A history of medications being used for other conditions should always be taken.
An acute wet cough is most likely due to lower respiratory tract infections. In some cases, antibiotics may be required. Wet cough with high fever should be evaluated for pneumonia, and treated with antibiotics. Chronic wet cough is most commonly due to COPD and smoking. COPD should be evaluated for in all cases of chronic wet cough especially if lasting over 2 years. Any wet cough with breathlessness worsening on exertion or lying down, especially with a cardiac history should be assessed for heart function.
Also read:
Common Cold and Flu- Know the difference, effective care and 10 alert signs


1 Comment
Good afternoon thanks for the information.