Inflammation and allergy are common terms used in conversations but it is interesting to understand what exactly they mean.
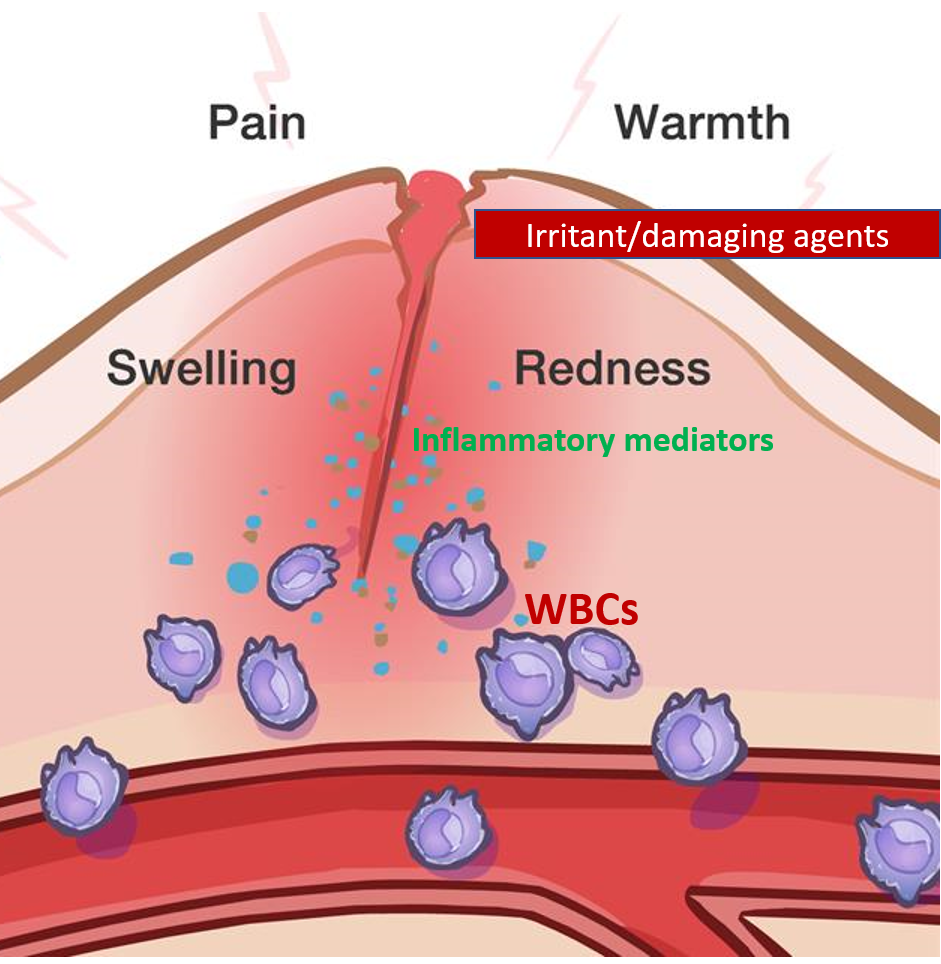
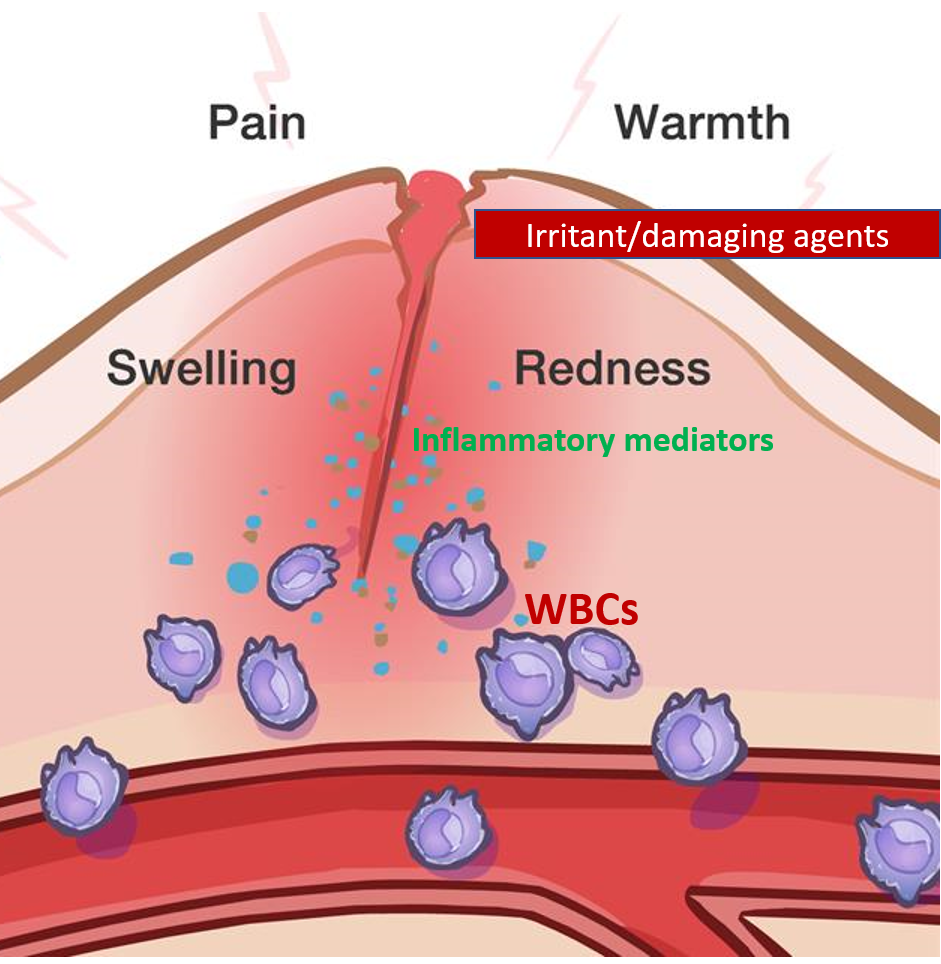
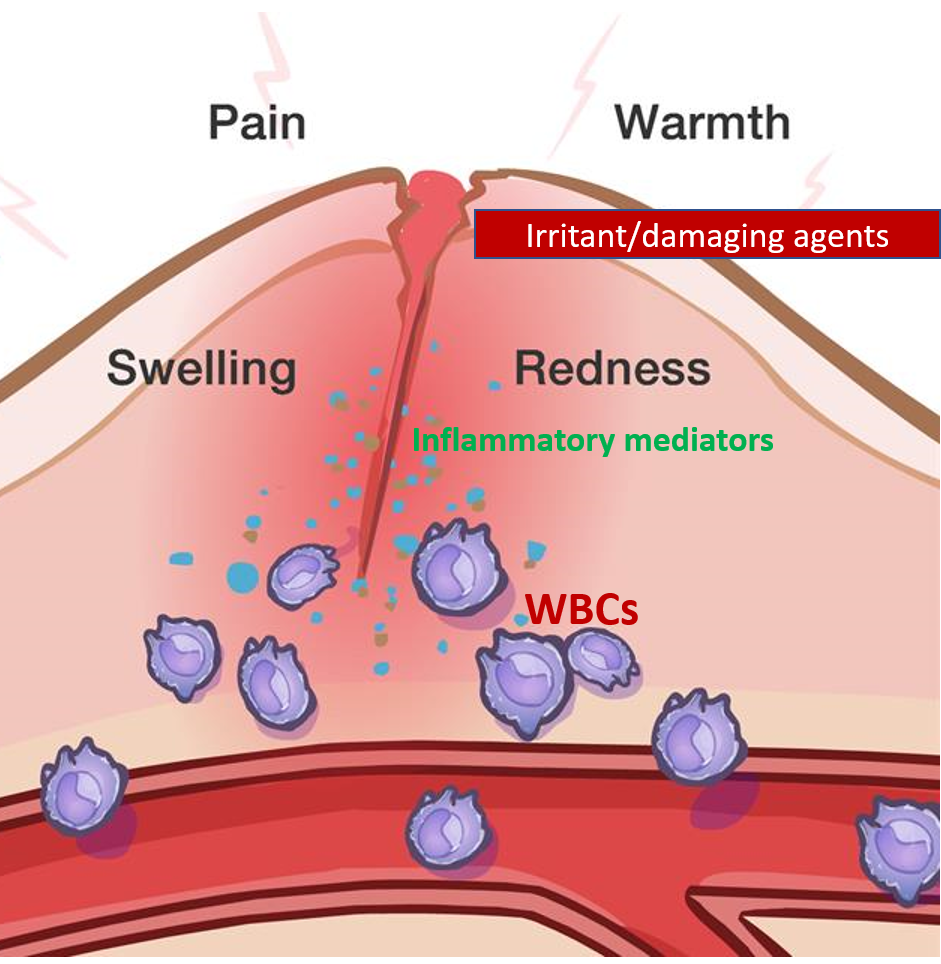
Whenever the body is confronted or attacked by a foreign damaging or irritating agent, there is a reaction or a defensive response by our body’s cells and tissues as well as the immune system. This is observed by us as local symptoms like redness, pain, swelling, itching, irritation and warmth of the affected part, and sometimes generalized symptoms like fever, weakness and body ache. Let us understand how this happens.
INFLAMMATION
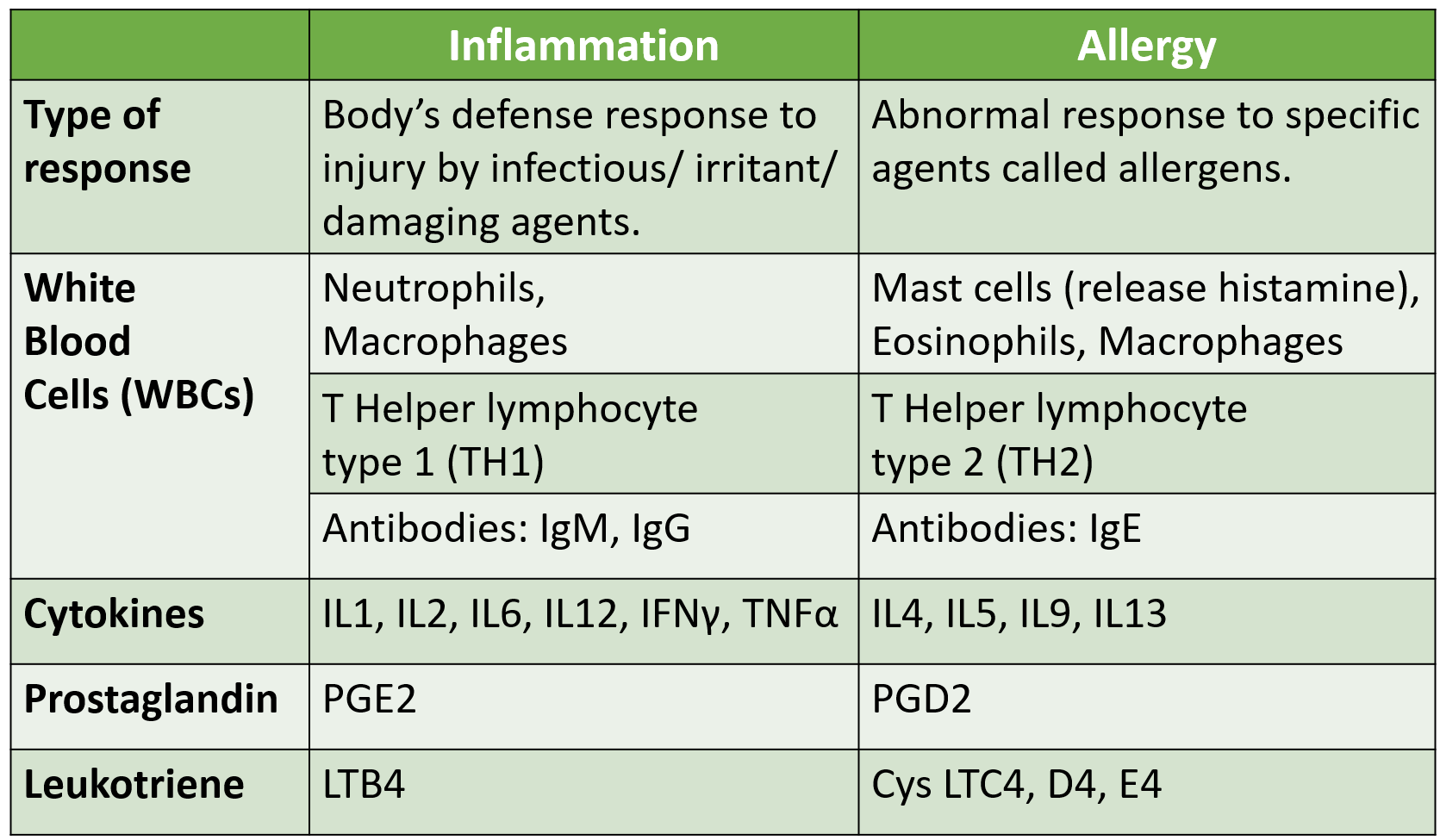
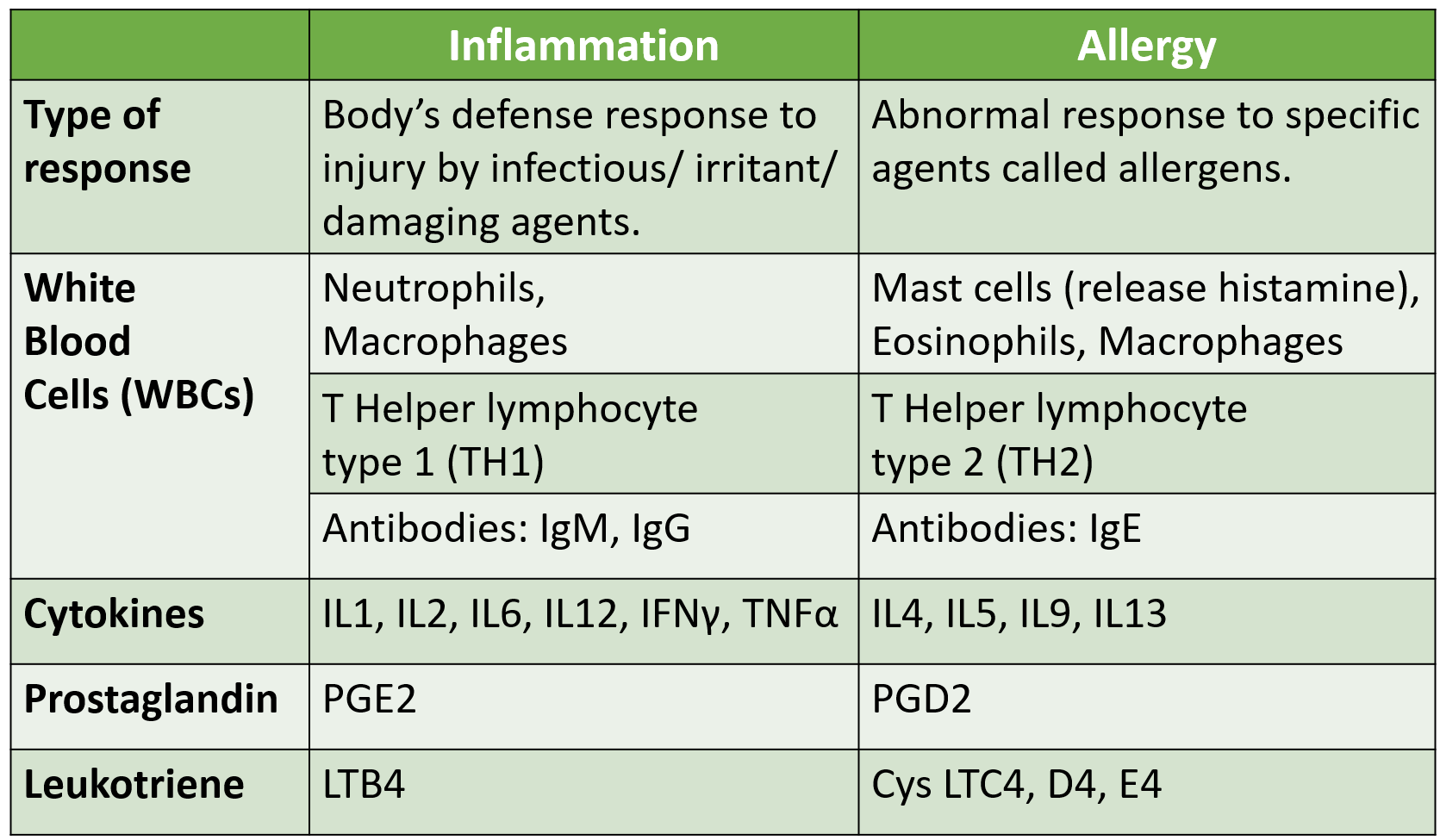
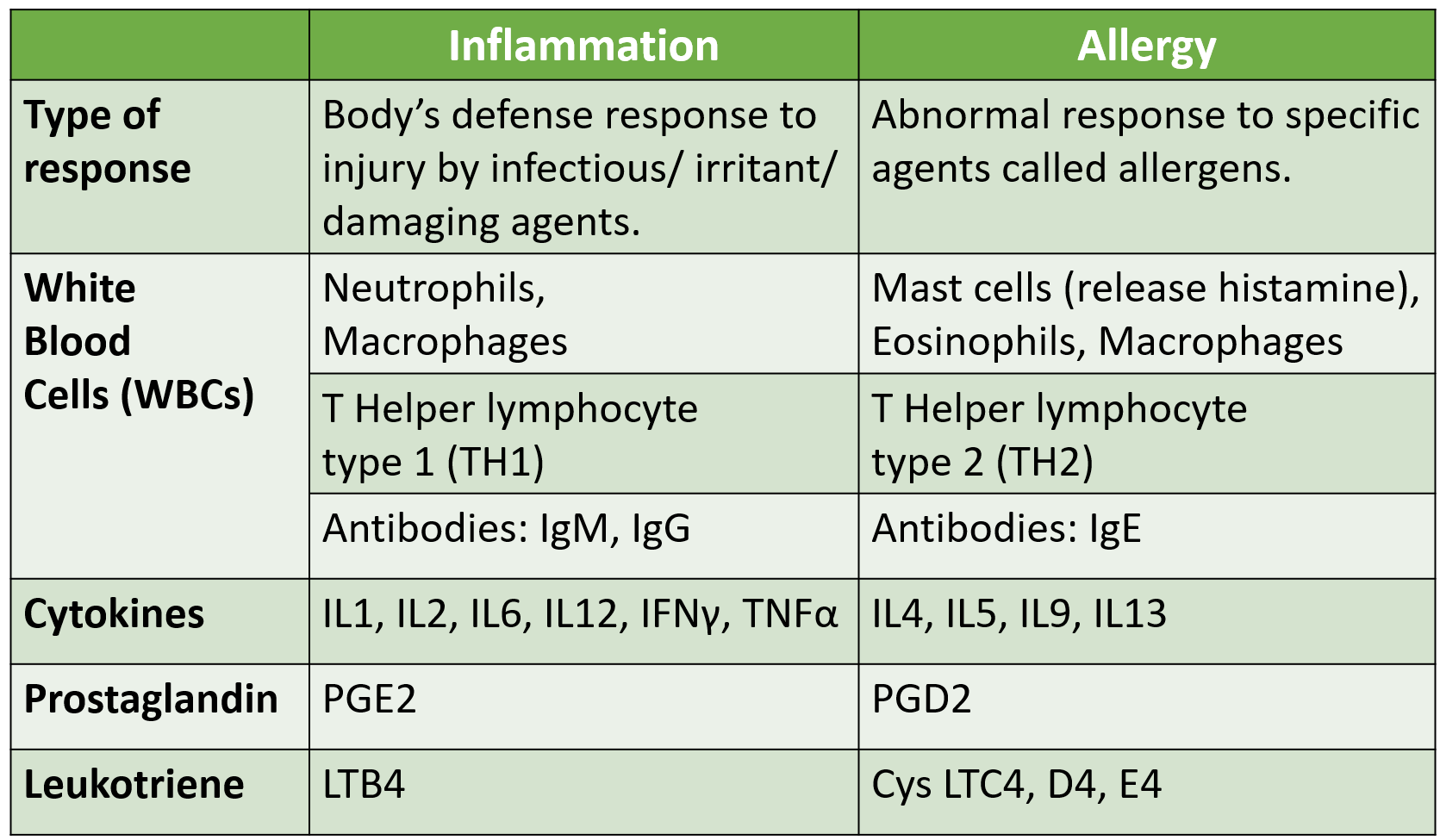
Inflammation is the body’s normal defense response or reaction to an irritant or damaging agent causing injury to the body cells/tissues. These agents can be infectious microbes (pathogens), chemicals, tobacco, smoke/exhaust, environmental toxins or mechanical injuries/accidents.
Inflammatory response: It consists of the following processes–
- Release of inflammatory mediators: The damage to the cell’s protective covering (cell membrane) leads to the release of its components called phospholipids, which are converted to inflammatory mediators called prostaglandins and leukotrienes by enzymes. Prostaglandins induce early symptoms of inflammation like pain, redness, swelling and fever, while the leukotrienes act over a period of time to sustain inflammation and produce more long-term sequelae.
- Immune system activation: Different types of white blood cells (WBCs) along with the plasma (fluid component of blood, with proteins) filter out of the blood vessels into the injured site.
White blood cells are of two types:
- Granulocytes: These include neutrophils, basophils and eosinophils in blood, and mast cells in tissues. These contain prominent ‘granules’ that release inflammatory mediators like histamine, kinins, or oxidase/peroxidase enzymes (produce free radicals) that act immediately and non-specifically to destroy the offending agent.
- Agranulocytes: These include monocytes (have fine granules – transform into macrophages in tissues) and lymphocytes that do not have granules. Lymphocytes are T or B type, the latter producing antibodies against infectious agents and allergens, take some time to come in and, are specific with memory.
Plasma proteins belong to the complement system (C1-9) that assist the granulocytes and antibodies in clearing the infectious/irritant agent, or are clotting proteins to wall off and heal the injured site.
Cytokines are intermediary messaging proteins released by various immune system cells, and also play a role in the inflammation and immune process.
Read: Immunity, the functioning of the immune system, and types of immune responses
The signs and symptoms of inflammation are –
- dilation of blood vessels (redness – erythema, and local warmth)
- leakage of plasma and WBCs out of the blood vessels at the site of injury (swelling – edema)
- stimulation of the nerves of the area (pain/irritation/itching)
- rise in temperature (warmth of site or fever) seen in some cases.
The term ‘itis’ is added to denote inflammation like hepatitis (inflammation of the liver), gastritis (inflammation of the stomach), arthritis (inflammation of the joint), etc.
Acute versus Chronic Inflammation
The inflammation can be acute that is sudden over a short period of time (often called a reaction), or it can be chronic that is over a prolonged period of time due to ongoing damage. Acute inflammation is seen due to infections, injuries or exposure to irritating/toxic substances (like gastritis-food poisoning, conjunctivitis, common cold, sore throat-pharyngitis, pneumonia, skin rashes, wounds, accidents, etc.)
Chronic inflammatory conditions have acute periods where the inflammation is exaggerated (called exacerbations or flare-up episodes) and symptom-free periods when the inflammation is in control (remission) as seen in arthritis, inflammatory bowel disease (IBD) and chronic bronchitis (COPD- chronic obstructive airway disease).
Treatment of Inflammation
General treatment like rest especially resting the affected body part which would involve appropriate movement restriction or diet modification, along with improved sleep and care is recommended. To reduce inflammation after injuries the RICE treatment is given: rest, ice application, compression bandaging and elevation of the part, to reduce swelling and pain.
NSAIDs (Nonsteroidal Anti-Inflammatory Drugs) are medicines that act by inhibiting the enzyme (cyclo-oxygenase- COX) which forms prostaglandins. These are the most commonly prescribed medicines for inflammation (ibuprofen, diclofenac, aceclofenac, naproxen, etc.).
Analgesics (medicines to reduce pain) like paracetamol is effective for pain and fever but does not reduce redness and swelling, so it is usually given in combination with NSAIDs. Sometimes stronger analgesics like tramadol belonging to the opioid class are given under medical supervision.
Proteolytic enzymes often in combination with NSAIDs are sometimes given in inflammation to break down debris, clean up, and help in healing the damaged tissues. (like trypsin, chymotrypsin, rutoside, bromelain, serratiopeptidase, etc.)
Corticosteroids are medicines that inhibit the formation of both prostaglandins and leukotrienes from the phospholipids and suppress activation of immune cells. These are used when inflammation is severe and causing significant damage. Examples include prednisolone, hydrocortisone, dexamethasone, betamethasone, etc.
Immune-suppressants drugs apart from corticosteroids (like methotrexate, azathioprine and cyclosporine) may have to be used in severe cases of inflammation.
Monoclonal antibodies (MAbs) are biological agents acting against a specific cytokine or antibody. These are reserved for inflammation which is severe and non-responsive to other medications. For example, infliximab, adalimumab (anti-TNF alpha cytokine) and tocilizumab (anti IL6 cytokine) for severe inflammation in IBD and arthritis.
Antioxidants act by eating up free radicals which are produced by enzymes of some of the granulocytes and cause ongoing inflammatory damage to cells and tissues. A number of herbs and natural substances also have anti-oxidant properties. These are used as supplementary long term therapy. Examples are omega 3 fatty acids, vitamin C and E, beta carotenes, turmeric (curcumin), flavonoids, glutathione, etc.
ALLERGY
Allergy is the body’s abnormal inflammatory response or reaction in certain people to a specific agent (allergen). Allergens can include dust (house dust mite- HDM), pollen/grass, animal dander, fungus, insects or some food items and drugs/medicines. Therefore, allergy is a similar response to inflammation but only in some people and that too to specific allergens which are normally not damaging or irritating to most people.
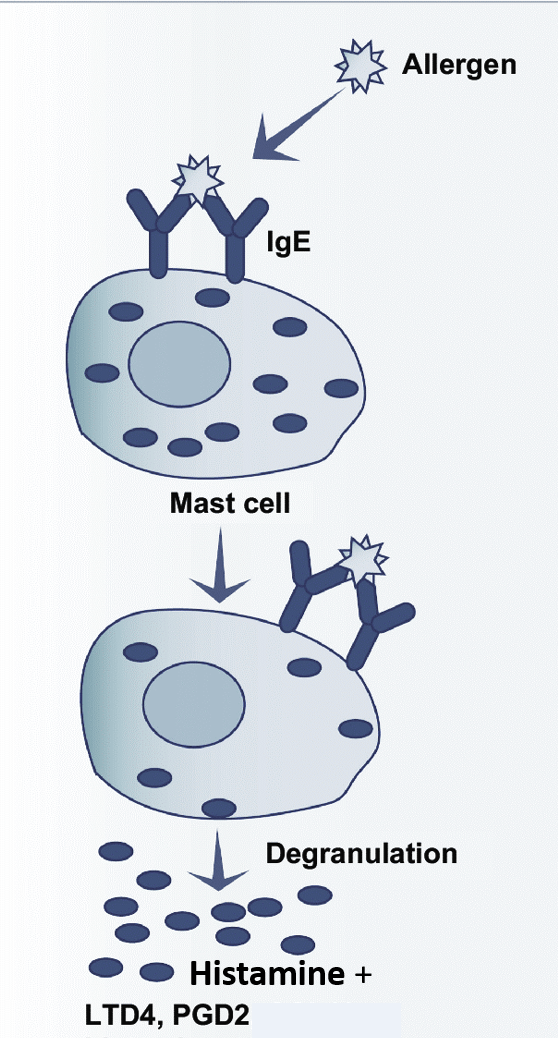
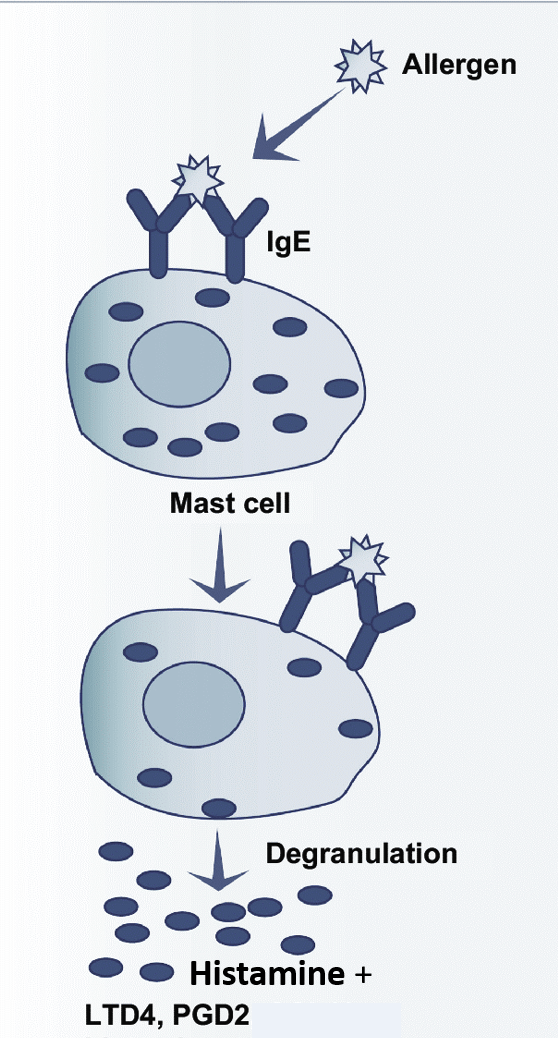
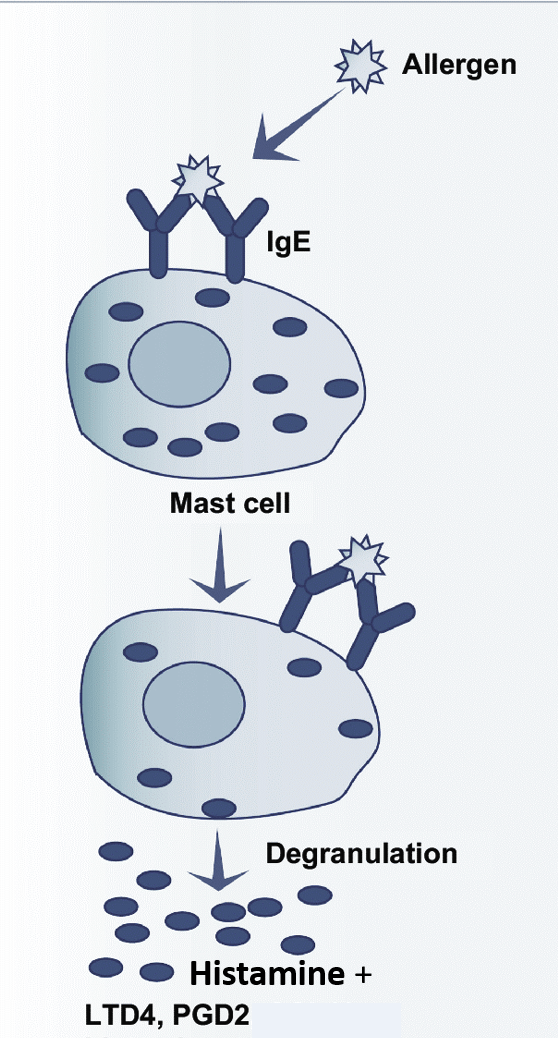
The cause of allergies is linked to the development and balance of the immune system, and sensitization to one or more allergens. In allergies, the type of immune response, cells and mediators are different as compared to the inflammatory response to infections/irritants. Mast cells releasing histamine stimulated by IgE antibodies is the central mechanism in allergies. In the blood, the eosinophils may show a rise. Atopy refers to the genetic tendency to develop allergic diseases and immune responses to common allergens.
While redness, swelling and discomfort are seen in both the allergic or inflammatory response, itching/irritation is more prominent in allergies, whereas pain, fever and other general symptoms like weakness or body ache are more common in inflammation.
The effect of exposure to irritating and damage-causing substances (like smoke, chemicals, tobacco, infections or cold) can be much worse in people with allergies as compared to the general population, and can lead to exaggeration of their allergic condition and symptoms.
Examples of allergic conditions are allergic rhinitis (nose), and allergic conjunctivitis (eyes), asthma (lower airways), atopic dermatitis/eczema (skin) and various food/drug allergies.
Sudden or acute, often unexpected allergic response is often called an allergic reaction as seen with food items, drugs/vaccines or contact with allergens. While chronic allergic conditions like asthma, eczema (atopic dermatitis) and allergic rhinitis have periods of flare-ups in between long intervals of being under control.
Anaphylaxis is a severe allergic reaction that can occur within seconds or minutes of exposure to an allergen. Symptoms include skin rashes, vomiting, shortness of breath, weak pulse and shock. If not treated immediately (adrenalin – also called epinephrine), it can result in unconsciousness or death
Treatment of Allergy
For allergy, maintaining an allergy diary to understand and avoid the responsible allergens is useful.
Antihistamines are agents that prevent the action of histamine once released, by blocking the target receptors (H1) through which it acts. These include first-generation sedative ones like chlorpheniramine, and second-generation less/non-sedating ones like cetirizine, levocetirizine, loratadine, desloratadine, fexofenadine, ebastine, bepotastine and bilastine. Antihistamines are the first-line medicines for managing allergies.
Corticosteroids are medicines that have multiple mechanisms of action. They can stabilize mast cells, reduce histamine release, inhibit the formation of both prostaglandins and leukotrienes from the phospholipids, and suppress activation of immune cells. Therefore, these are used to tackle both inflammation and allergies of moderate-severe nature. Examples include prednisolone, hydrocortisone, dexamethasone, betamethasone, etc.
LTRA (Leukotriene receptor antagonist) drug montelukast prevents the action of cys-leukotrienes and is a useful anti-allergy drug especially in allergic rhinitis and asthma.
Monoclonal antibodies (MAbs) as mentioned are biological agents acting against a specific cytokine or antibody and have been developed for allergies and inflammation, especially when severe and non-responsive to other medication. For example, omalizumab (anti-IgE) and mepolizumab (anti IL5) for conditions like asthma.
Allergen immunotherapy, also known as desensitization or hypo-sensitization, involves exposing a person to regular small doses of an allergen in an attempt to ‘acclimatize’ and reduce the immune system’s response against it. This is done after a process of allergy testing to identify the involved allergen/s.
Also read:
For any query, additional information or to discuss any case, write to info@drvarsha.com, and be assured of a response soon.