Everyone has suffered from itching at some time or the other. Itching is an unpleasant, irritating feeling or sensation on the skin which urges and makes you scratch. For some, itching is a chronic problem and can be a cause of great distress especially in the night-time compromising sleep and quality of life.
TYPES OF ITCHING
Itching (medically called pruritus; plural-pruritis) can be acute (sudden onset – lasting for a short duration of < 6 weeks) or chronic (has been present on and off, or continuously for > 6 weeks).
Itching can be localized (in particular parts of the body) or generalized (all over the body). For localized itching, a skin problem (dermatological disorder or disease) is usually the cause, however in generalized itching, one may need to investigate for non-skin causes (due to diseases in other organs – systemic causes).
IS THE ITCHING DUE TO A SKIN PROBLEM OR NOT?
DRY SKIN
It is the most common cause of generalized itching. Sometimes the skin hardly looks dry but when you scratch across it, to your surprise a white line will appear indicating underlying dryness! Dry skin can occur in all age-groups, increases with age, and is a very common problem in the elderly population. Dry skin is not considered a skin disease per se but can cause a distressing amount of chronic itching disturbing sleep.



SKIN INFLAMMATION
Localized itching in particular parts of the body, is usually due to skin disease or irritation and may have some obvious signs on the skin like a rash (a change in skin color and texture where the involved part looks red and inflamed, with a patchy or raised appearance, sometimes with blisters, cracks, scales, or swelling). A rash may or may not be painful but is commonly itchy.
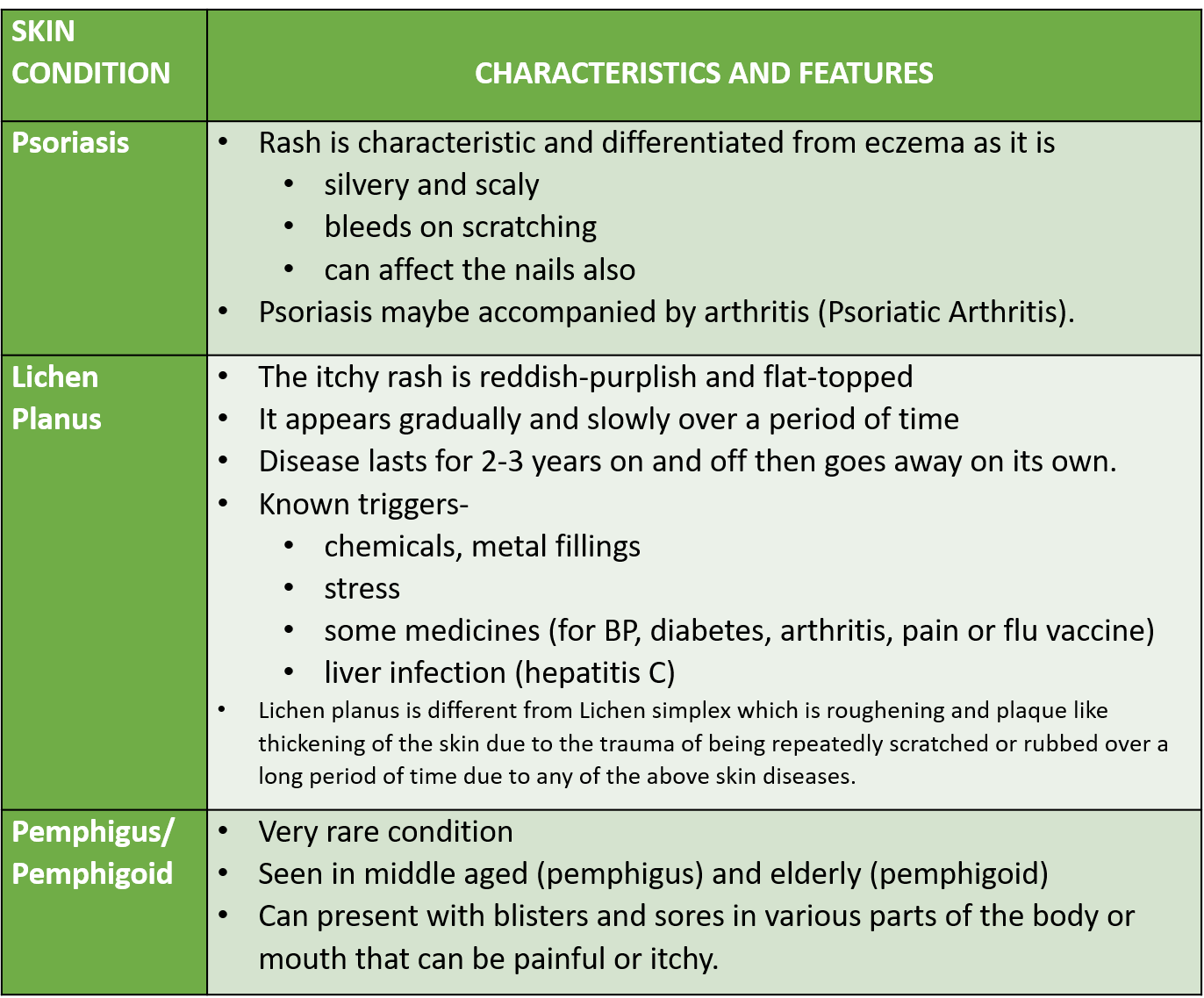
Skin diseases causing rashes and itching are tabulated below.
Inflammatory skin conditions like eczema, atopic dermatitis and urticaria (hives) are considered to be allergic in nature or due to irritant substances (contact dermatitis).
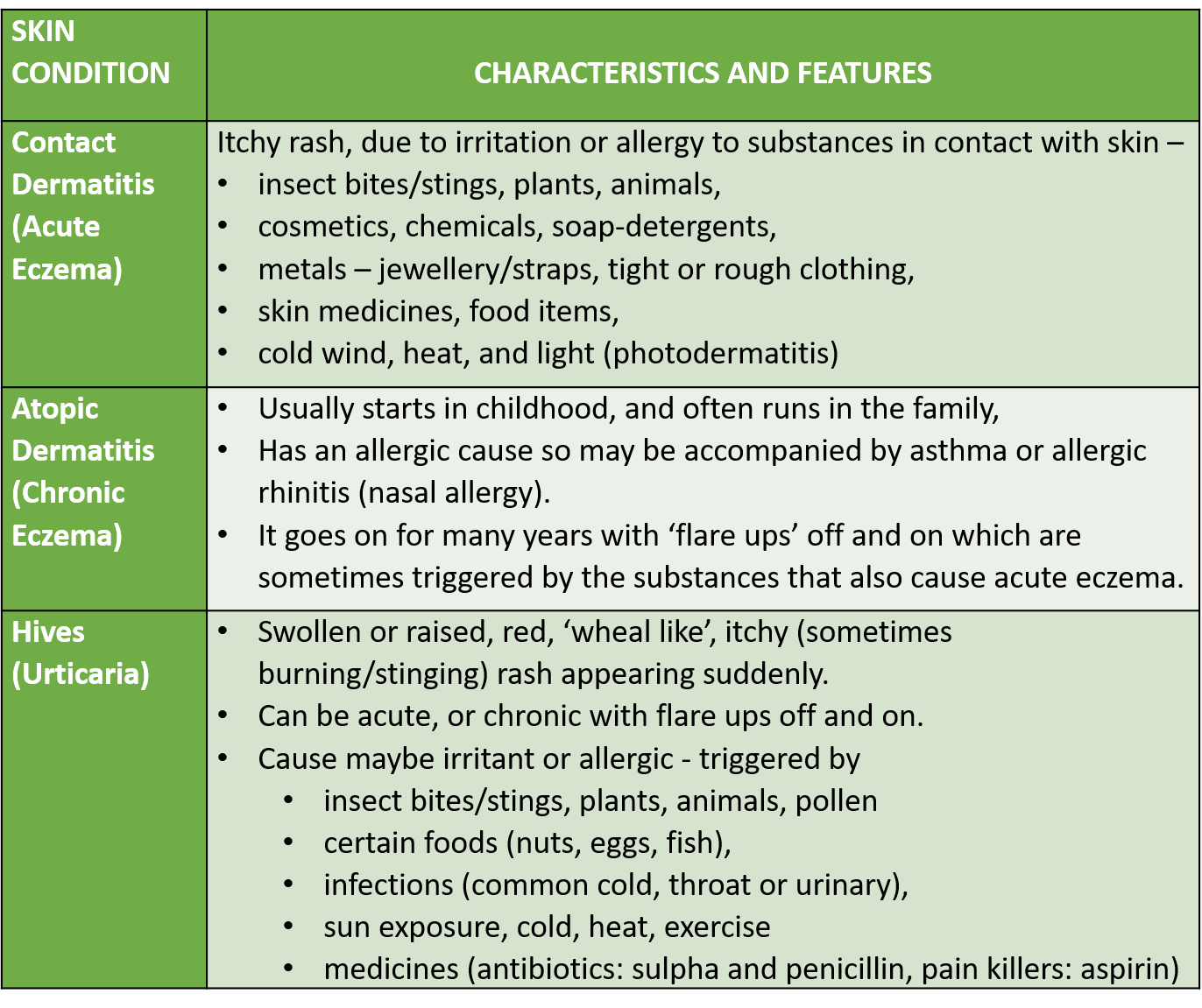
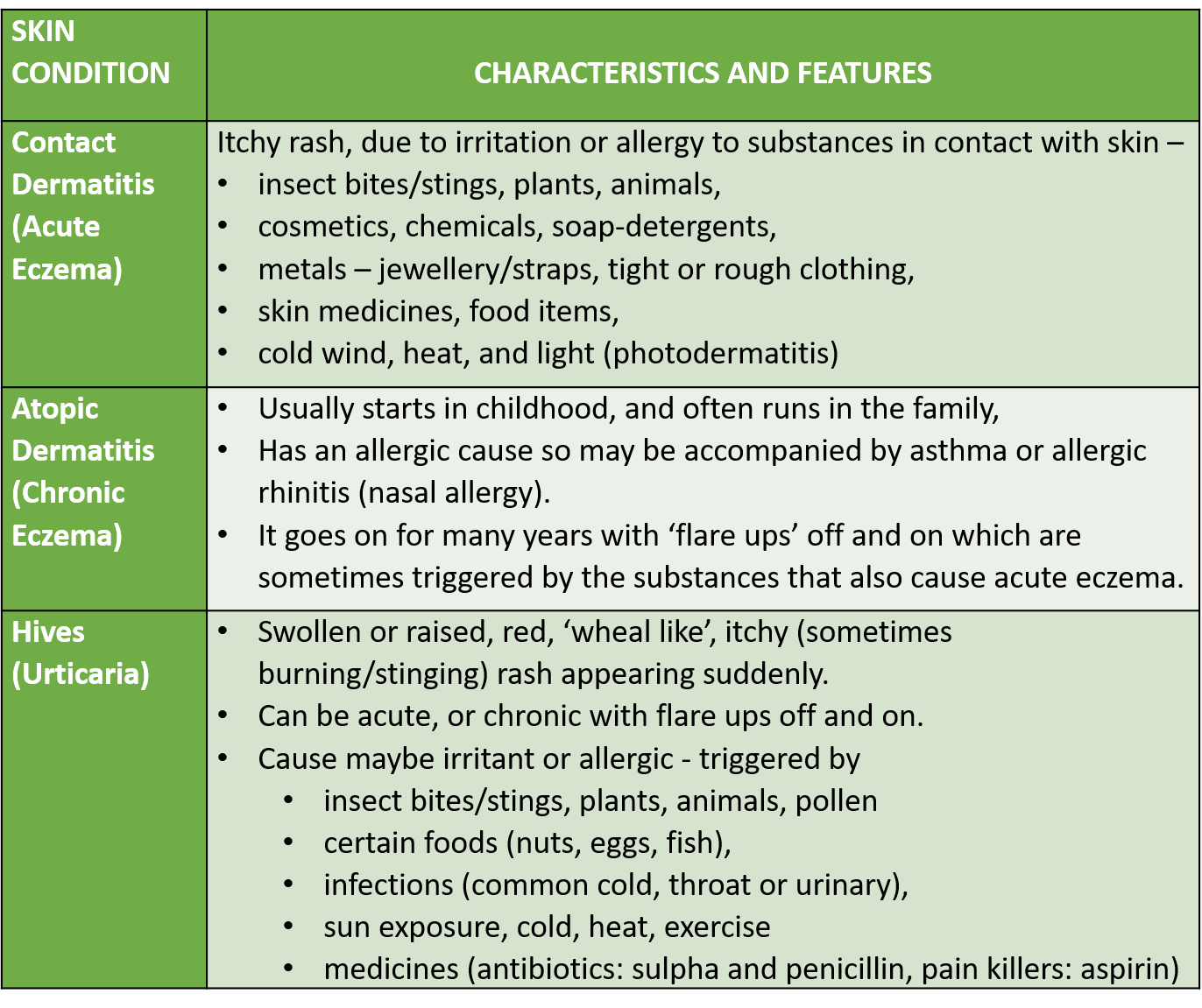
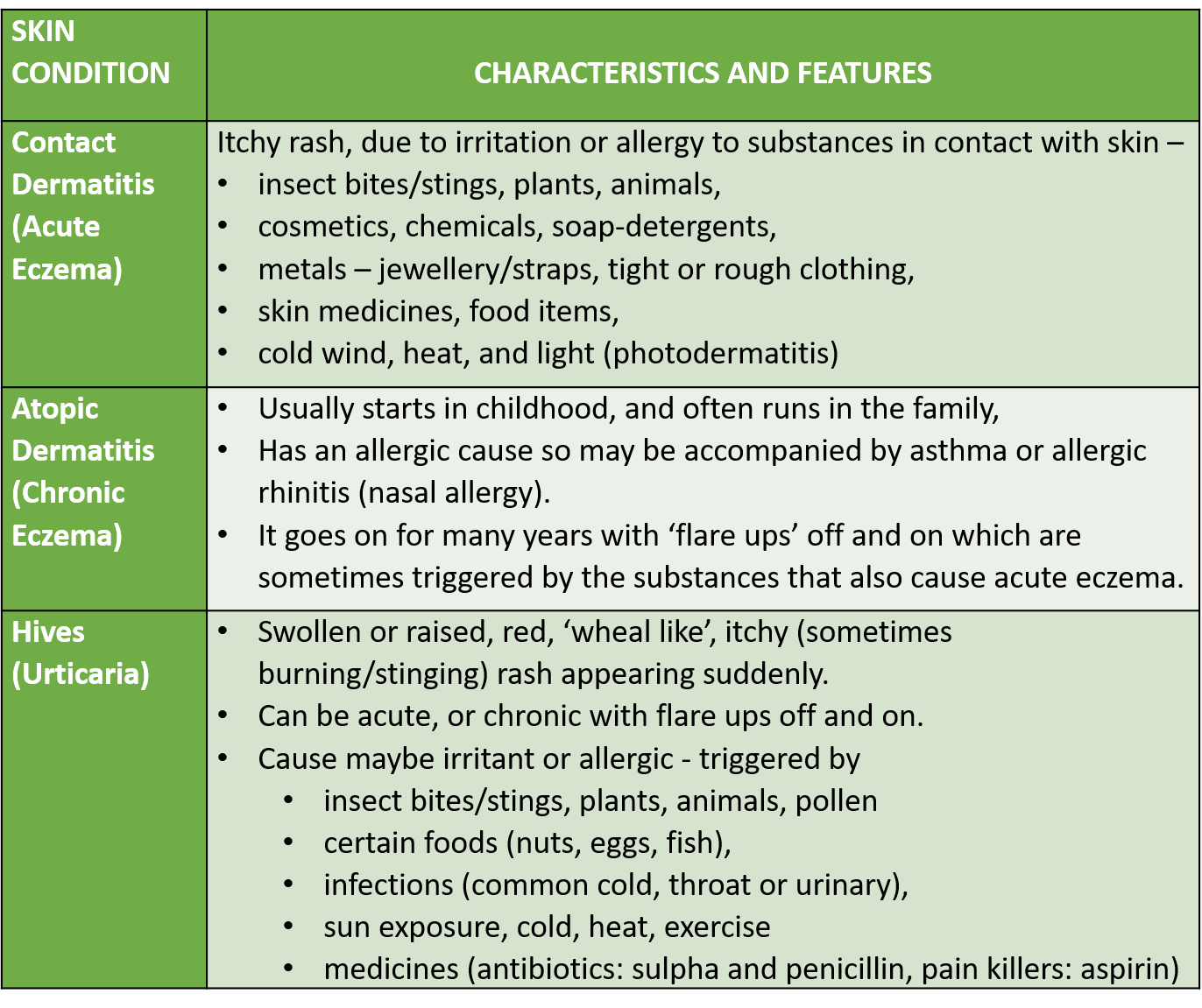
Photodermatoses are skin conditions producing skin inflammation (itchy, red rashes, and eruptions), that are caused by an abnormal reaction of the skin to sunlight (usually UV component, but sometimes visible light also). This could be photodermatitis, also called sun poisoning or photoallergy which is a skin reaction to an allergen that is activated by light, or it could be phototoxicity, also called photo-irritation, which is a chemically induced skin irritation, requiring light. Phytophotodermatitis is a condition causing skin inflammation and rash resulting from contact with light-sensitizing botanical (plant-derived –phyto) substances, called furanocoumarins, that contain particles called psoralens that are sensitive and activated by UV light.
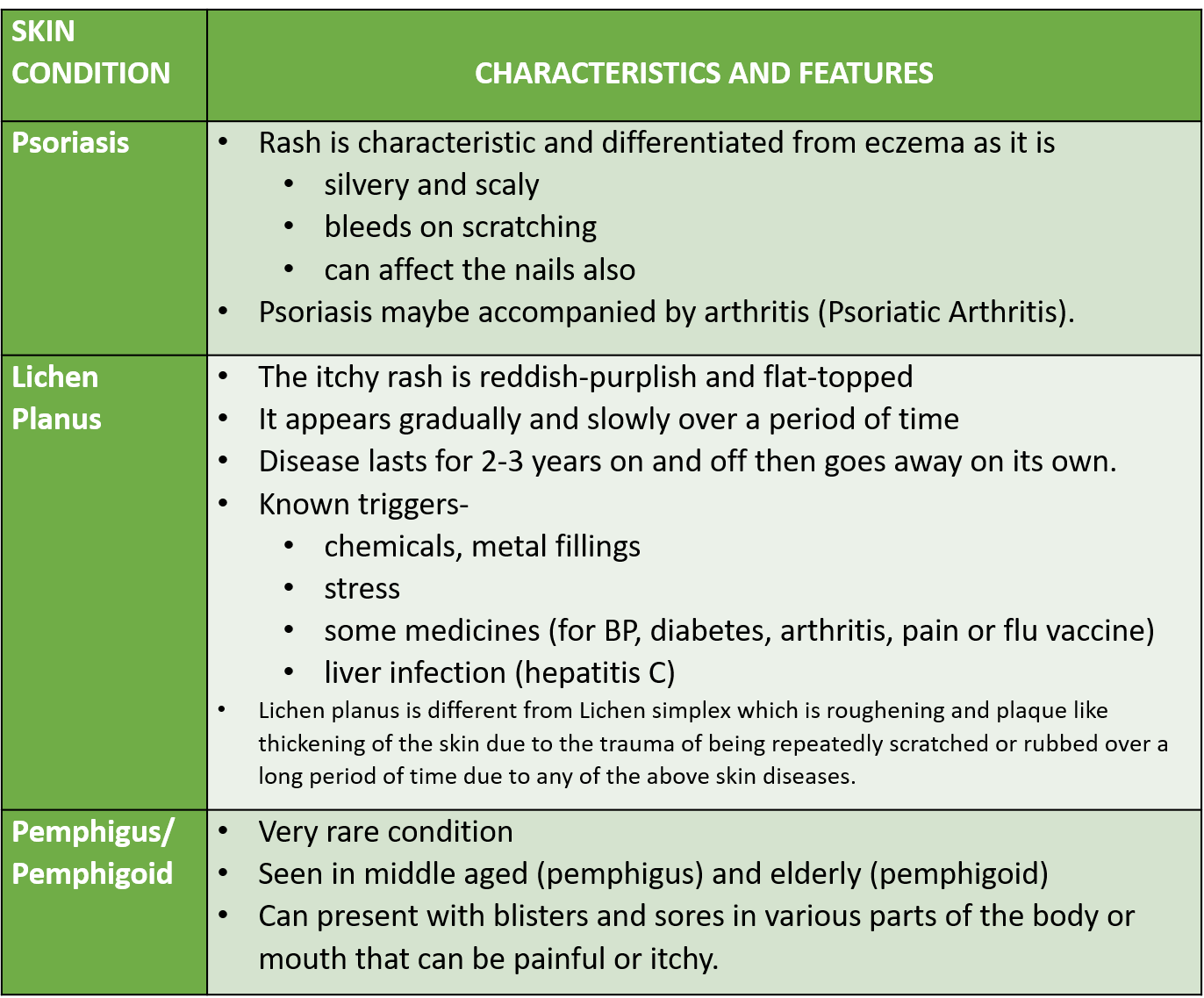
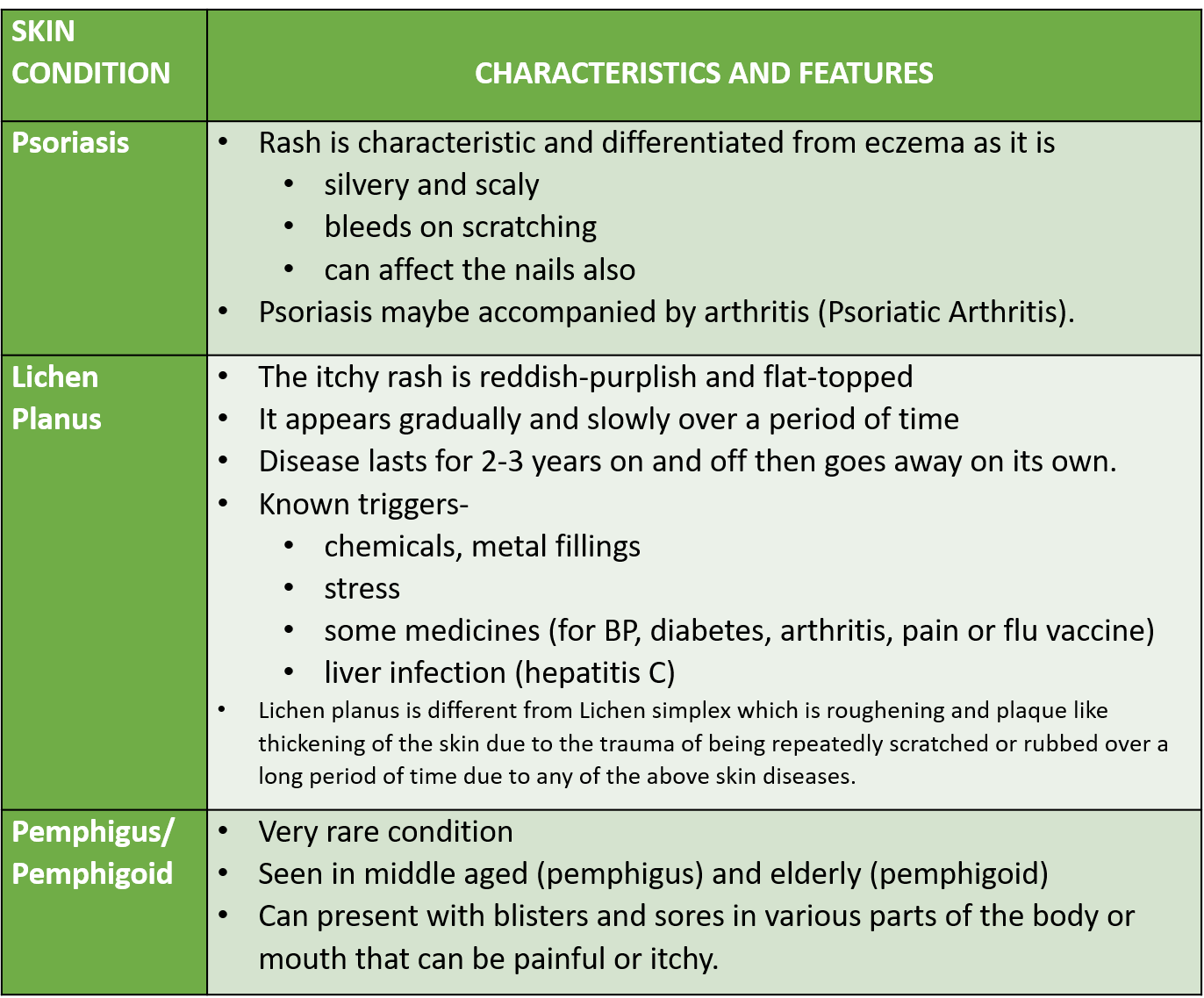
Other conditions like psoriasis, lichen planus and pemphigus/pemphigoid may have an autoimmune etiology (error in the body’s immune recognition and response).
Sometimes skin scars from wounds, burns or surgery can also be itchy.
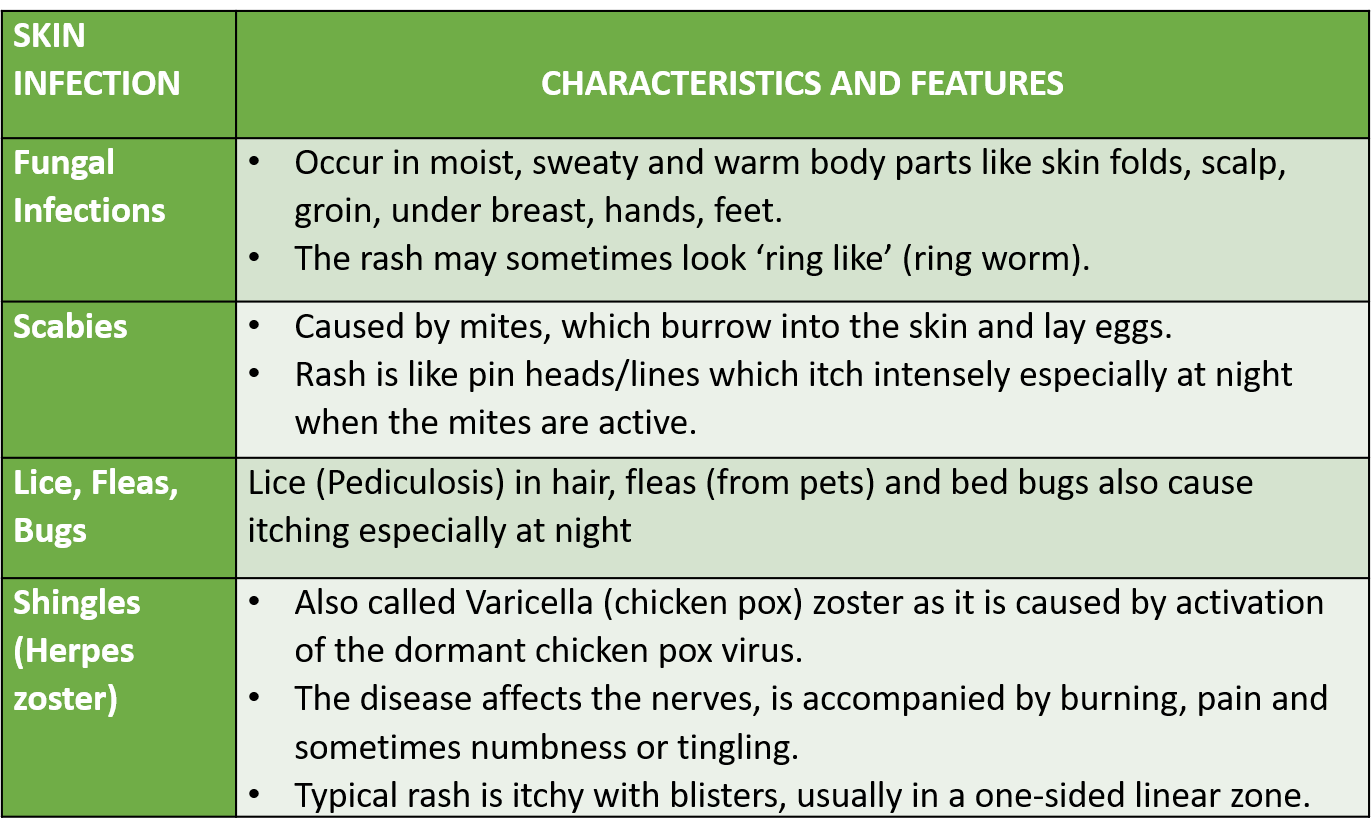
SKIN INFECTION
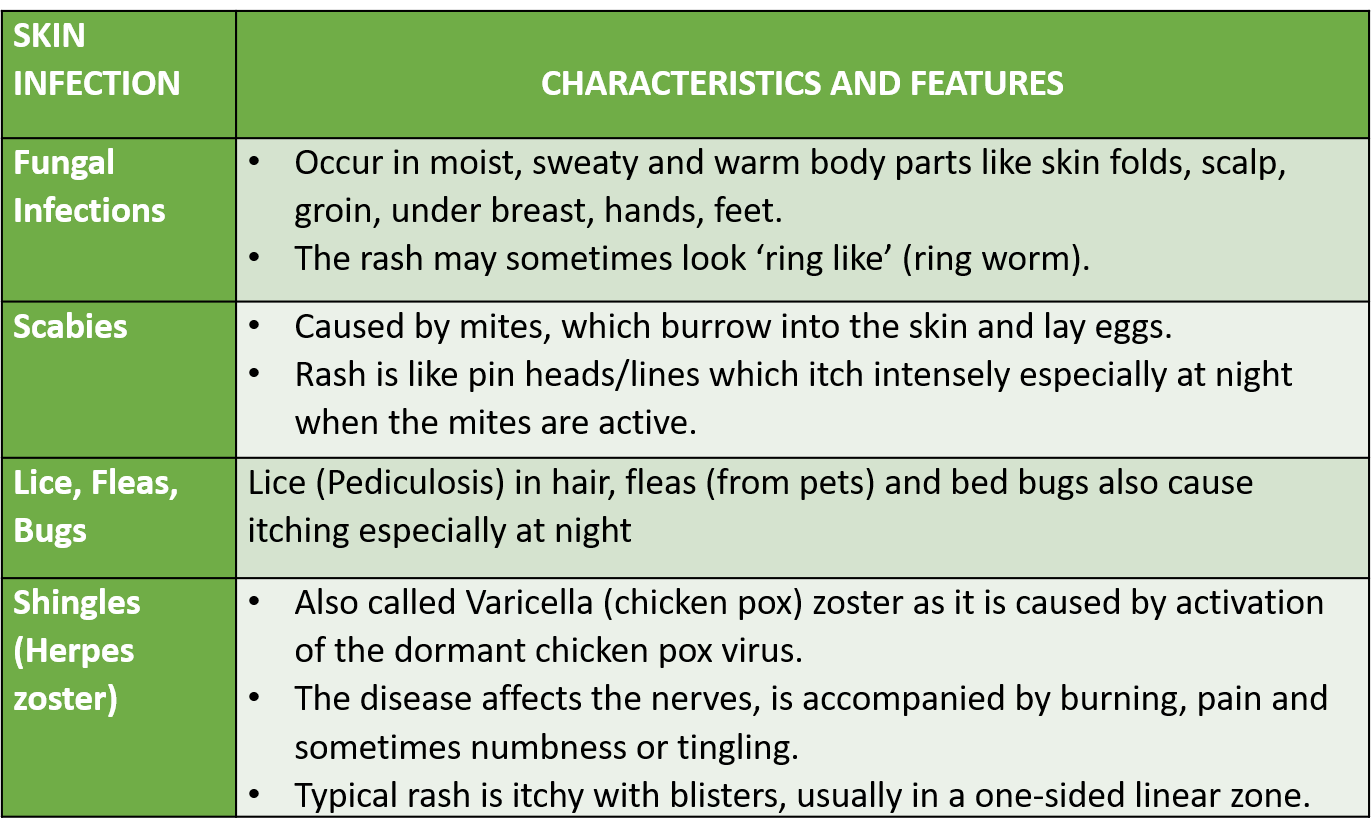
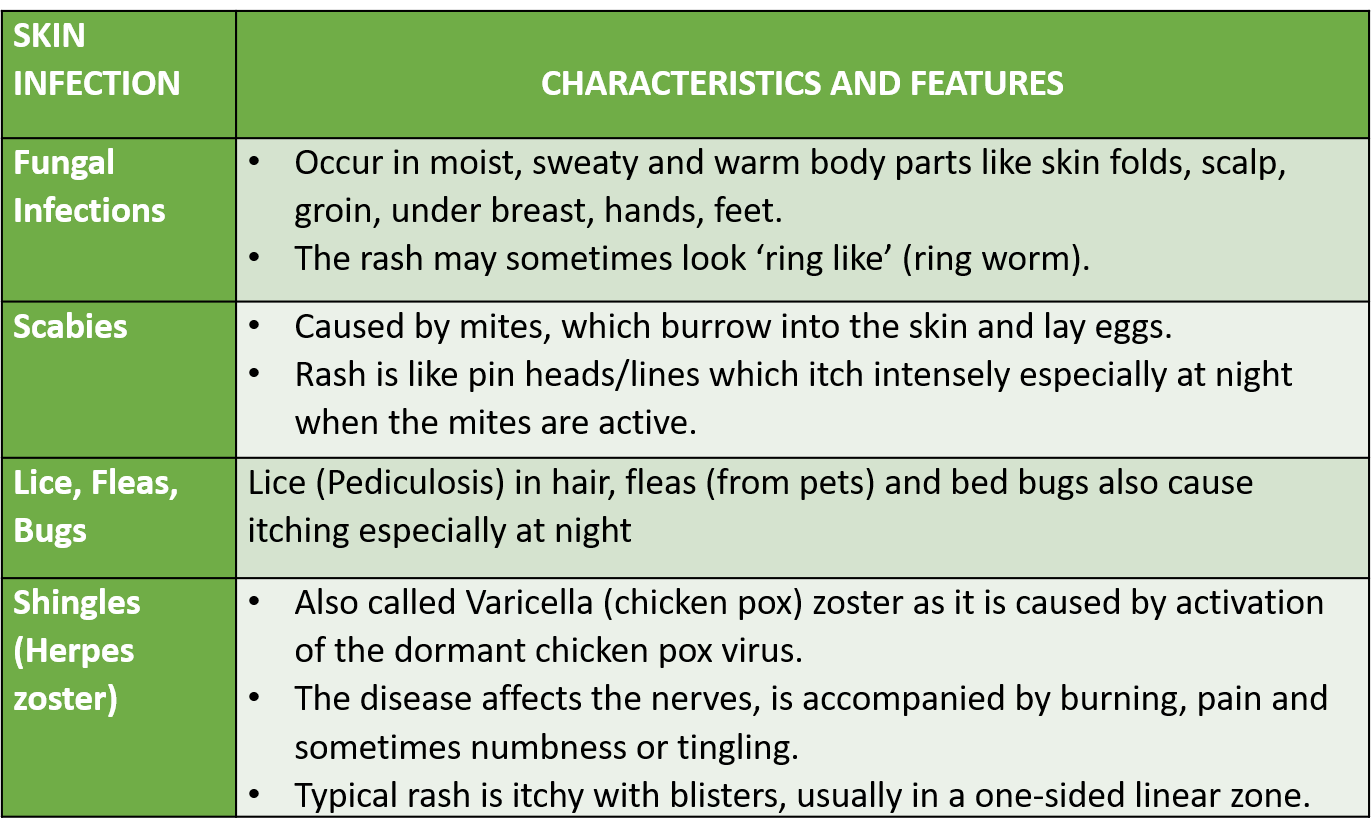
Skin infections that cause itching are often contagious like fungal infections, scabies, lice, and viral exanthems (chickenpox, herpes zoster, etc.) while others like eczema, psoriasis, hives (urticaria), and lichen planus are not.
Rash and Itch-Scratch cycle
Usually, skin diseases present with a rash before, along with, or just after the itching starts. Most skin diseases have a characteristic pattern and appearance of the rash, which can clinch the diagnosis for a doctor.
However, even if itching is not due to a skin disease, repeated, prolonged and forceful scratching of the skin induces a lot of trauma which can lead to a rash developing over a period of time, making it look like a primary skin disease by the time you visit a doctor! So, knowing the timing of the development of rash and itching is of importance. Scratching itself causes skin irritation leading to more itching (called the itch-scratch cycle). Severe itching and inflammation also increase the production of melanin (skin color pigment) causing the affected part to darken (post-inflammatory hyperpigmentation -PIH).
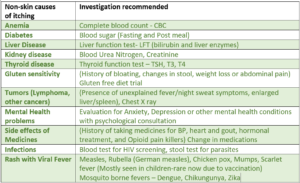
SYSTEMIC CONDITIONS
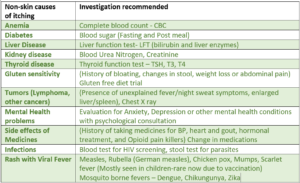
Apart from dry skin, generalized itching may not be due to a skin-related cause, and can be a symptom of other organ diseases (systemic causes). These conditions include diabetes, liver, kidney or thyroid disease, iron deficiency anemia, mental health causes like anxiety and depression, and rarely some tumors (like lymphoma). Such possible causes should be investigated, especially in the elderly. Some medicines can also have itching as a side effect like those for BP, heart, gout, hormonal treatment, and pain (opioid pain killers). During pregnancy, and around monthly menstrual time, hormonal changes occur which can in some women be a cause of generalized itching.
WHY IS ITCHING MORE PRONOUNCED AT NIGHT?
Irritation to the nerve endings in the skin is picked up by receptors and relayed as an itch sensation to the spinal cord and brain, which thereafter send back signals which cause us the urge to scratch. The commonest and most well-studied itch mediator is ‘histamine‘ but other mediators are also involved.
Many conditions (both skin and non-skin related) including dry skin, are associated with the itching being significantly more in the night. There are many reasons for this. There is an increase in skin temperature and more water loss from the skin during the late evening and night thereby increasing skin dryness. The levels of our body’s steroid hormones (which reduce itch and inflammation) are lower at night. There may be more release of certain substances in the evening/night like beta-endorphins (known to lower pain perception but increase itch sensation), and other mediators of itch and inflammation (enkephalins, IL2, PGD2, PGE2, TXB2). There are fewer distractions at night, cumulated mental stress of the day, sometimes with anxiety or depression, all of which increase itch perception.
Night-time (nocturnal) itching impacts sleep and the next day’s performance and can reduce efficiency in day-to-day life.
HEALTH SOLUTIONS
The specific disease (skin-related or systemic) is medically treated accordingly once diagnosed. The following therapies are generally used in treating itchy skin inflammatory conditions and rash.
MOISTURIZERS AND SOOTHING AGENTS
Lotions/creams and oils are the first line of management along with lifestyle modification especially when dry skin is present. Many lotion/creams have natural substances with moisturizing, soothing and anti-inflammatory/anti-itch properties which are not only beneficial for relieving symptoms but also suitable for long-term usage due to the absence of any significant side effects. Some of these substances include coconut oil, colloidal oatmeal, aloe vera, tea tree oil, turmeric, honey, shea/cocoa butter, wheat germ oil, and cetearyl alcohol.
Applying such moisturizing lotions/creams, especially at night, bathing in lukewarm water, along with using non-alkaline soaps or bathing oils are effective solutions.
Calamine is a soothing agent commonly used to relieve acute itching caused by exposure to irritants.
MEDICINES
Antihistamines are a class of oral drugs that may be prescribed to provide symptomatic relief from itching and allergy, and also help improve sleep.
Counterirritants are agents that produce a superficial irritation in one part to relieve irritation/itching in another part. This happens by stimulation of temperature receptors in the skin, which produce a sensation of heat or cold. Examples are menthol, methyl salicylate, camphor, thymol and capsaicin, which are commonly added to creams and lotions for itching.
Corticosteroids are immunomodulatory medicines that act by suppressing inflammatory mediators of our immune system and are therefore effective in relieving moderate-severe skin inflammation as well as itching. Corticosteroids are commonly part of creams and ointments given for itching and are the cornerstone of managing skin inflammations like eczema and psoriasis. Corticosteroids can range in potency from low (hydrocortisone), medium (triamcinolone, mometasone, beclomethasone) and high (clobetasol, halobetasol). In severe cases, they may be given orally (prednisone, methylprednisolone, dexamethasone) for a limited period.
Other immunomodulatory medicines available are calcineurin inhibitors tacrolimus/pimecrolimus (used in atopic dermatitis), and vitamin D analog calcipotriol (in combination with a corticosteroid for psoriasis), available as ointments. Methotrexate, cyclosporine, azathioprine, etc. are oral immunomodulators that may be prescribed in some severe cases of psoriasis.
Acitretin is an oral retinoid used in psoriasis that acts by decreasing the scale formation due to the abnormal growth, multiplication, and thickening of skin cells.
Note: Corticosteroid and immunomodulatory medicines should never be used without a doctor’s prescription as their dosing, and usage needs medical supervision to avert and minimize adverse effects. Acitretin should be used only after pregnancy has been completely excluded and contraception started.
Biologicals (monoclonal antibodies- MAbs) act by targeting specific components of the immune system that are causing the inflammatory or allergic reaction. These are reserved for severe and unresponsive cases like omalizumab (urticaria), dupilumab (atopic dermatitis) and infliximab, adalimumab, and secukinumab (psoriasis).
Infections like bacterial/fungal, herpes, scabies or lice are treated with specific drugs acting against the causative organisms. It is important not to cause skin damage and secondary infection due to the trauma of recurrent and forceful scratching. Such secondary infections will need to be treated with the application of antibiotics as cream/ointments which are also available in combination with corticosteroids.
In some cases, light therapy may be an option a dermatologist may offer.
Psychological intervention and medication in the form of behavioral modification therapy and antidepressant/antianxiety medicines can also help under appropriate medical monitoring, in select cases of generalized itching.
Also read-
Skin Infections – Types, Predisposing Factors and Health Measures
Understanding Viral Exanthems – Viral Diseases with Rash and Eruptions
For any query, additional information or to discuss any case, write to info@drvarsha.com, and be assured of a response soon.
References:
Diagnosis and management of chronic pruritus: An expert consensus review
Pruritus: Etiology and patient evaluation
A Diagnostic Approach to Pruritis


