Quick Read – Tips for planning Diet in Diabetes
DIABETES TYPES AND RISKS
Diabetes, as we all know, is a condition of impaired glucose metabolism and the presence of increased blood glucose (hyperglycemia). The utilization of glucose is regulated by a hormone called Insulin produced by the pancreas.
Type 1 Diabetes
It occurs due to the lack of insulin production by the pancreas. It has a genetic predisposition, sets in rapidly and at an early age (commonly in childhood itself), and is usually not related to lifestyle factors and weight. The cause is linked to the destruction of the insulin-producing cells of the pancreas by the body’s immune system due to an inherent recognition error (autoimmune disorder). The treatment requires taking Insulin (so also called Insulin Dependent Diabetes Mellitus: IDDM).
Type 2 Diabetes
It is the more common type constituting >90% of Diabetes cases globally, and is a metabolic disease seen in adults. The cause here is linked to the impaired response of the body to insulin (insulin resistance or decreased insulin sensitivity) which leads to ineffective utilization of glucose by the body cells.
The most recognized risk factors include
- age >45 years
- male gender
- women who had gestational diabetes (diabetes during pregnancy)
- family history
- high BMI/obesity
- presence of high blood pressure
- sedentary lifestyle
- Race: African, Asian and Hispanic or Latino races are more at risk than Europeans or Americans.
- Associated conditions: Abnormal lipid profile (high triglycerides, low HDL), heart disease or history of stroke, and conditions like polycystic ovarian syndrome (PCOS) and depression.
Type 2 Diabetes can be treated by medicines to reduce blood glucose, and increase glucose utilization, insulin production, and insulin sensitivity. (So it is called Non-Insulin Dependent Diabetes Mellitus: NIDDM).
DIAGNOSIS
Symptoms of diabetes include increased urination, thirst, and hunger, sometimes with weight loss, fatigue, moodiness, vision changes, and increased healing time of infections/wounds. While Type 1 Diabetes presents with more pronounced and definite symptoms, Type 2 Diabetes usually gets picked up on routine screening of blood glucose (also called blood sugar) or during a health checkup, as often no definitive symptoms may be present. The diagnostic criteria are as below.
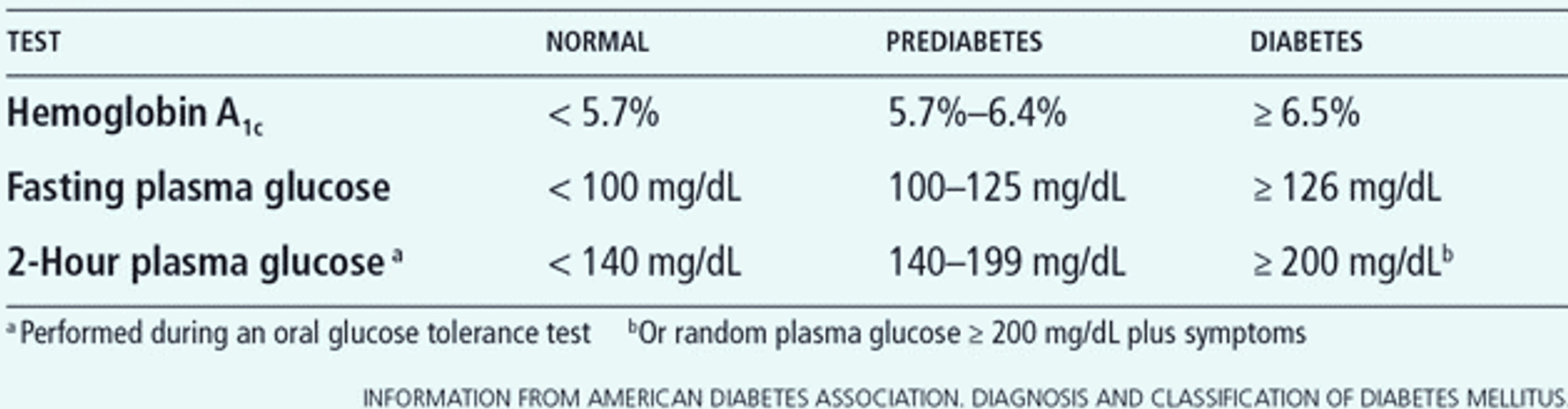
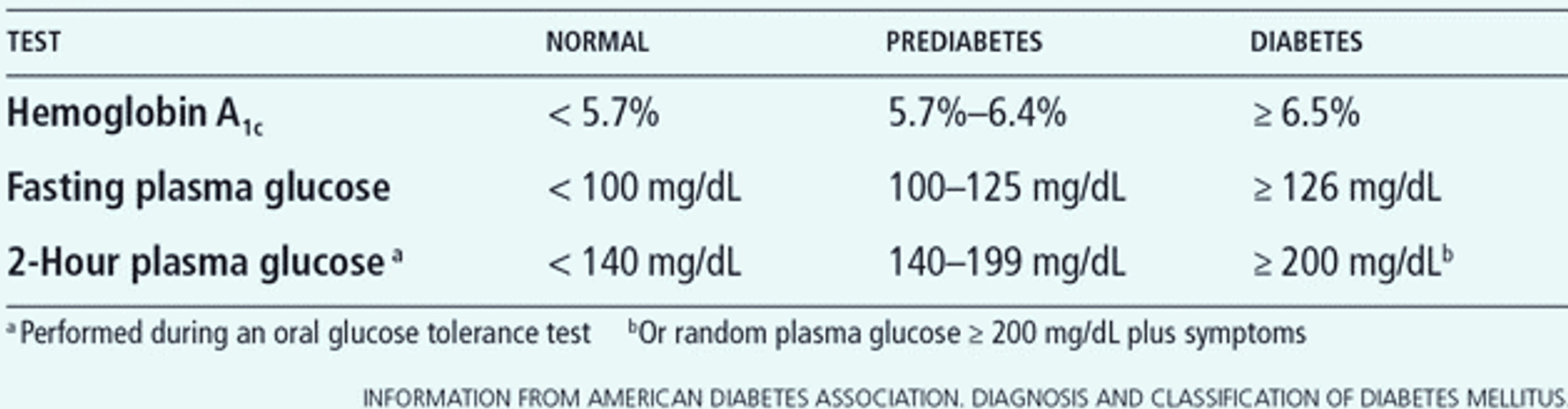
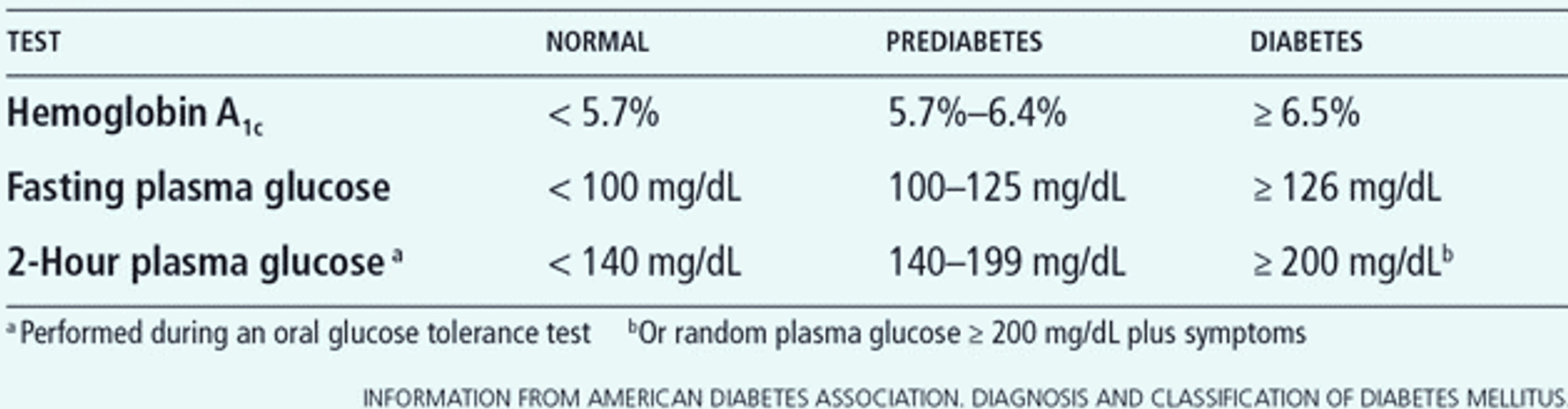
Prediabetes (also called Impaired Glucose Tolerance) is a state when blood sugar is raised but not enough to qualify as diabetes, but increasing the risk of developing diabetes. An oral glucose tolerance test (OGTT) checks fasting sugar followed by 75 gms glucose intake and a post-2-hour blood glucose test, and helps to confirm diabetes in cases in whom fasting blood sugar is persistently in the pre-diabetic range. OGTT is also done to confirm or diagnose gestational diabetes (diabetes in pregnancy).
The term Post Prandial Glucose refers to the rise of blood sugar after meals and is tested 2 hours after a regular meal. Though this has importance in monitoring and assessing response to treatment in diabetics, it has low evidence of a strong correlation with the diagnosis of diabetes and is not used for the same. Personalized glycemic response (PGR) refers to differences in postprandial rise in blood sugar between two people after consumption of the same food.
Glycated hemoglobin, (or glycosylated hemoglobin) is a form of hemoglobin that is chemically linked to a sugar. Several types of glycated hemoglobin measures exist, of which HbA1c, is a standard single test. for diabetes
Blood sugar fasting (F), OGTT, and Post-meal (Post Prandial: PP) show current blood glucose status, and HbA1c test gives the blood sugar over the past 2-3 months.
MANAGEMENT
While type 1 Diabetes is treated with Insulin, Type 2 Diabetes is managed by a combination of Diet, Lifestyle modifications and Medicines, with Insulin usage in specific individuals and situations. The target should be to maintain fasting/pre-meal sugars between 80-130mg% and post-meal sugars less than 180mg%.
Diet
Diabetics should eat a healthy diet rich in vegetables, fruits, legumes, and whole grains, low on calories, and fat, and devoid of refined sugars. In fact, such a diet would benefit the health of the whole family in general as it helps cut down the risk of developing diabetes in predisposed people and maintain weight, BP and a healthy heart. The DASH diet is an example of a diet benefitting people with high blood pressure diabetes, obesity or high BMI and heart disease. Weight loss of 4 to 5 kg over a few months can cut diabetes risk by 50%.
It is good to remember a 3-point solution for Diet in Diabetics
Selection of Food Items
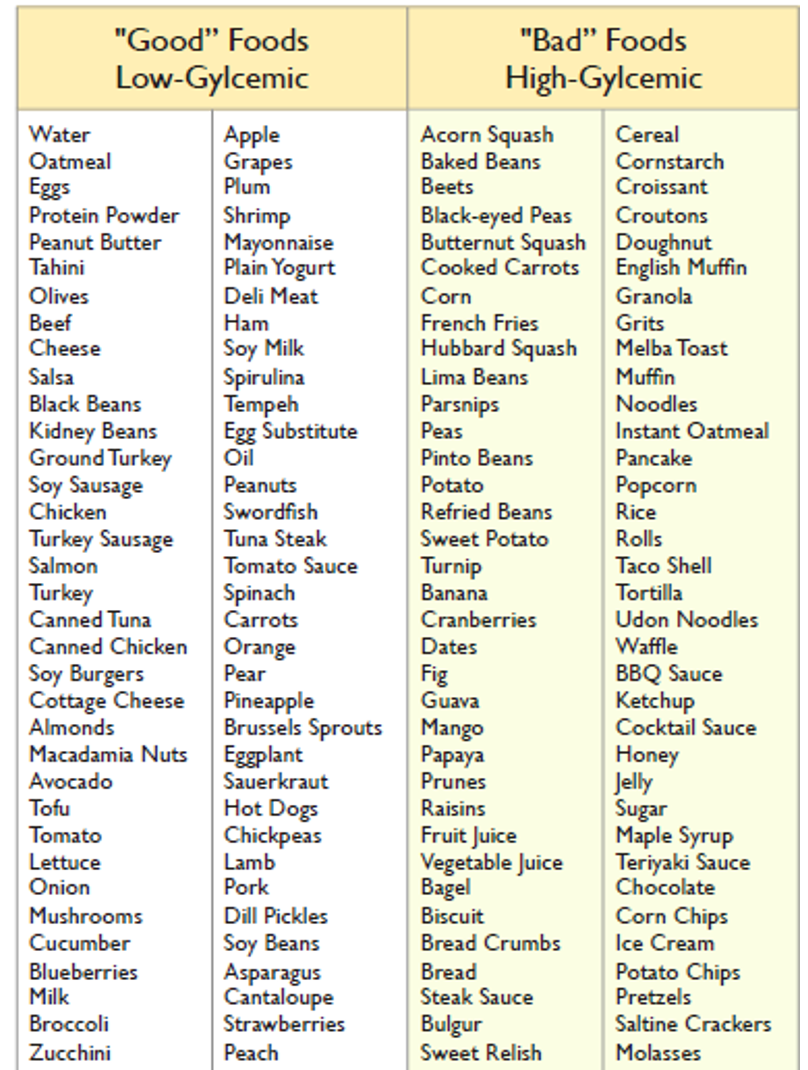
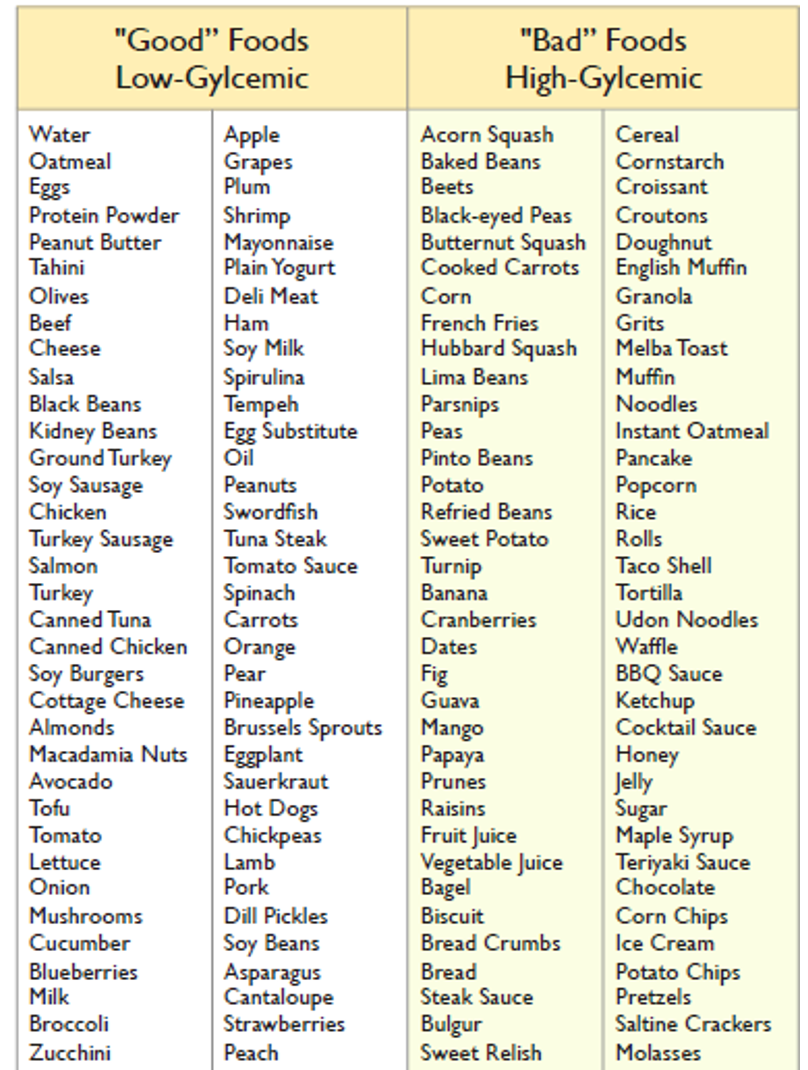
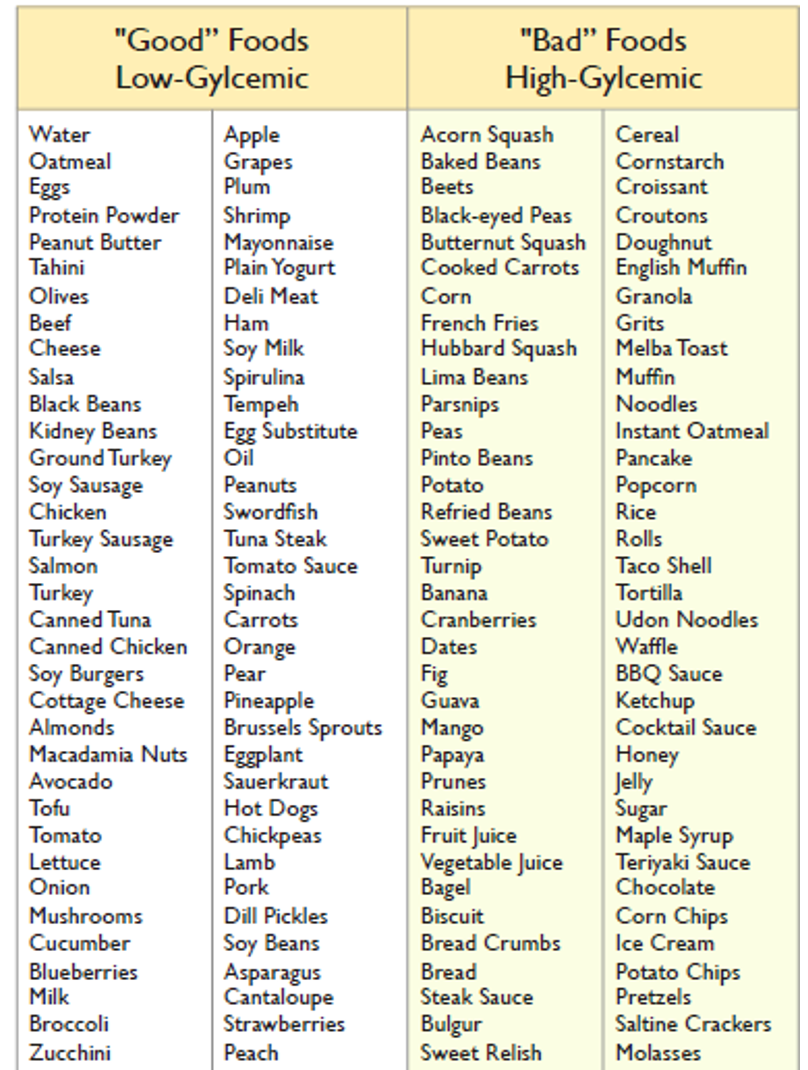
This should be done according to the Glycemic Index (GI) of the food which is a ranking according to glycemic load (ability to raise blood sugar). One can select from various food lists and should include Good – low GI (55 or less) foods and avoid Bad – high GI (>70) foods in the diet.
Deciding the Proportion of Nutrients
Your meal plate should be proportional as well as optimal in all nutrients:
- Fill half the plate with vegetables (all green vegetables, tomatoes, and carrots).
- One quarter with a starchy item like whole wheat (as roti/bread), brown rice, potato, corn, or any of the pulses (beans, peas or lentils).
- One quarter should have a protein item like lean meats, chicken, egg or fish. (vegetarian protein sources – paneer/tofu/cottage cheese, yogurt, soybean, almonds).
For vegetarians, pulses are good sources of proteins as well as starch, so one can go with half plate non-starchy vegetables, 3/8ths pulses, 1/8th non-pulse protein source. Include at least one fruit daily either as a snack or part of the vegetable half of your meal plate. Also, include one unsweetened beverage and at least 1.5-2 liters of water as part of your daily diet.
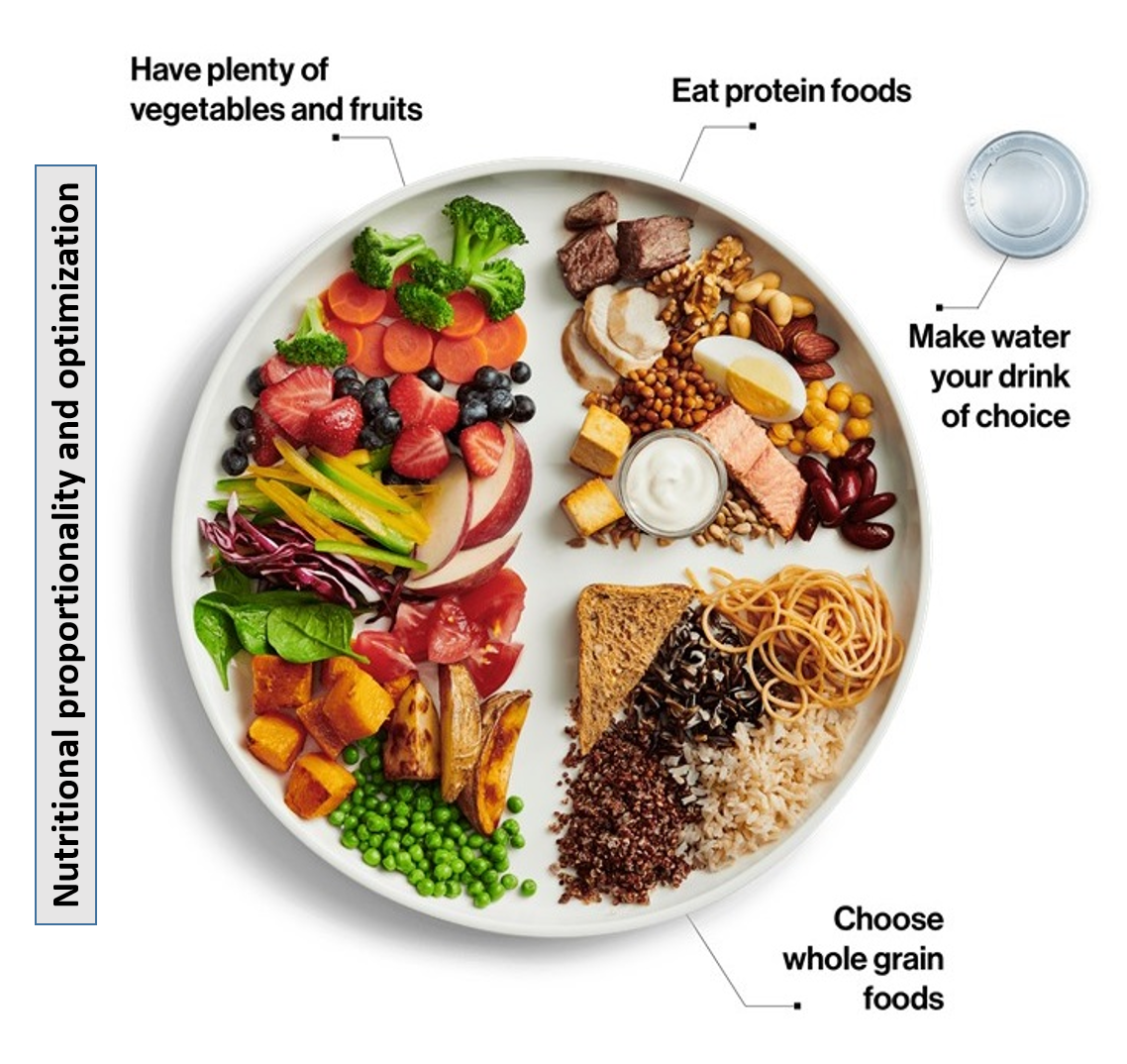
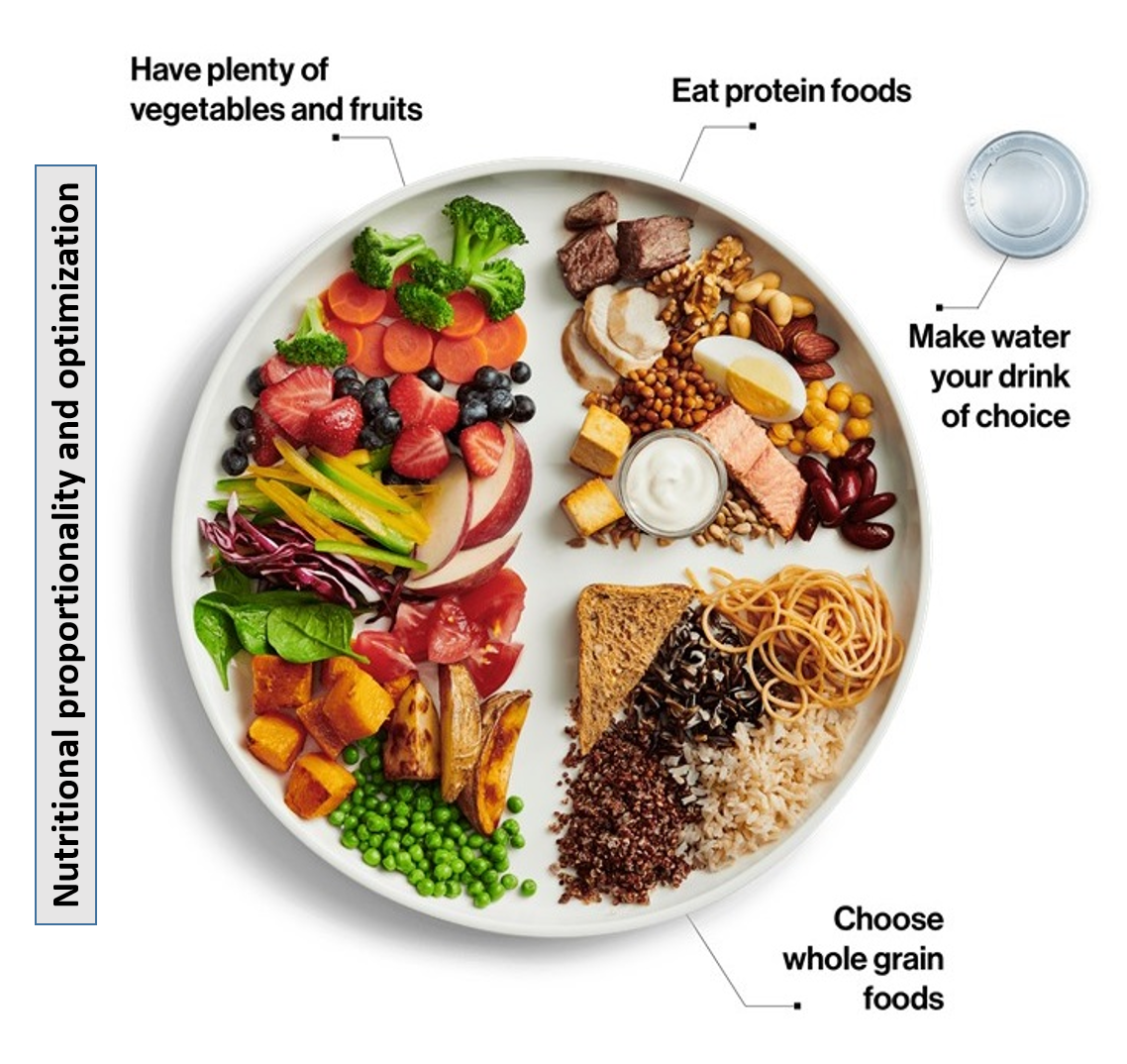
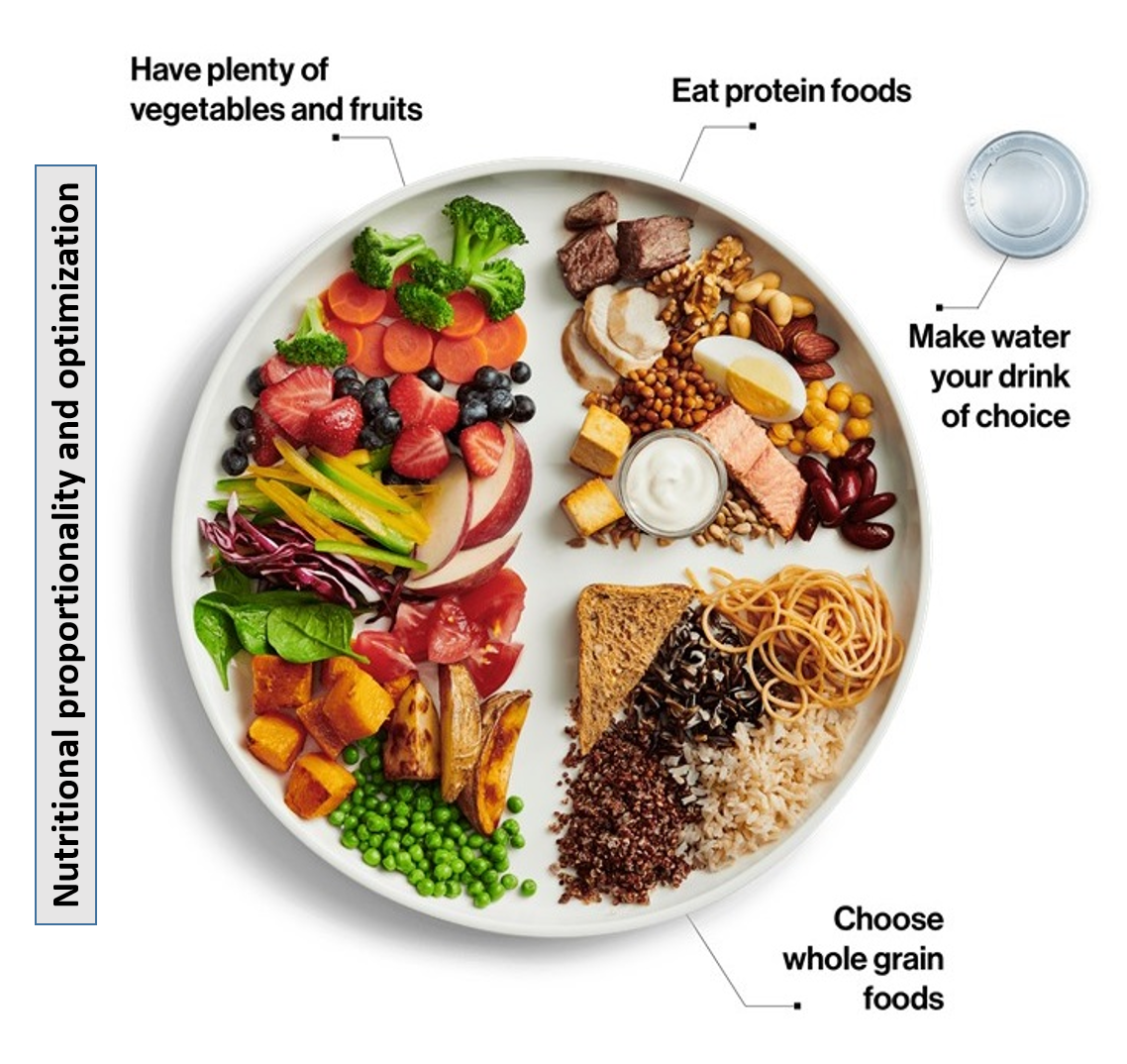
The above plate distribution assures the appropriate glycemic index of food, balanced nutrition as well as adequate fiber. One should ideally design one’s diet with the help of the diabetologist and nutritionist who take into account the personalized glycemic response (PGR) of various foods.
Cooking oil and fat should include good fats – cis unsaturated fats along with some amount of specifically omega 3 fats and some amount of medium-chain saturated fats.
Artificial sweeteners (also called high-intensity, non-nutritive sweeteners NNS or low-calorie sweeteners) approved as GRAS (Generally Regarded as Safe) by the country’s regulatory authority, may be used within ADI (acceptable daily intake). The USFDA has approved six NNS (saccharine, aspartame, sucralose, neotame, acesulfame-K, and stevia) for use in humans and has classified them under the GRAS category. The ADI for each NNS is usually set at 1/100 of the ‘no observed adverse effect level’ (the maximum level at which no adverse effects were seen in animal studies), and this is around 5mg/kg body weight/day.
Meal timings and frequency
Timely meals are important. If the gap between the meals is more than 3-4 hours, have a healthy mid snack like a whole grain cracker, a fruit, nuts/avocados, yogurt, low-fat non-fried items or buttermilk. The same type of snack can be had at bedtime if the gap between dinner and bedtime is more than 3 hours. Meals should not be unduly delayed or skipped. Also, do not eat very heavily in any single meal.
Lifestyle
Daily, at least half-hour of physical activity as brisk walking, jogging, swimming, cycling, yoga, or aerobics should be part of one’s lifestyle. If in a profession involving long hours of sitting, one should get up every 2 hours and take a 5-10 minute walk or do some simple hand and leg stretching. Smoking and alcohol are best omitted from lifestyle.
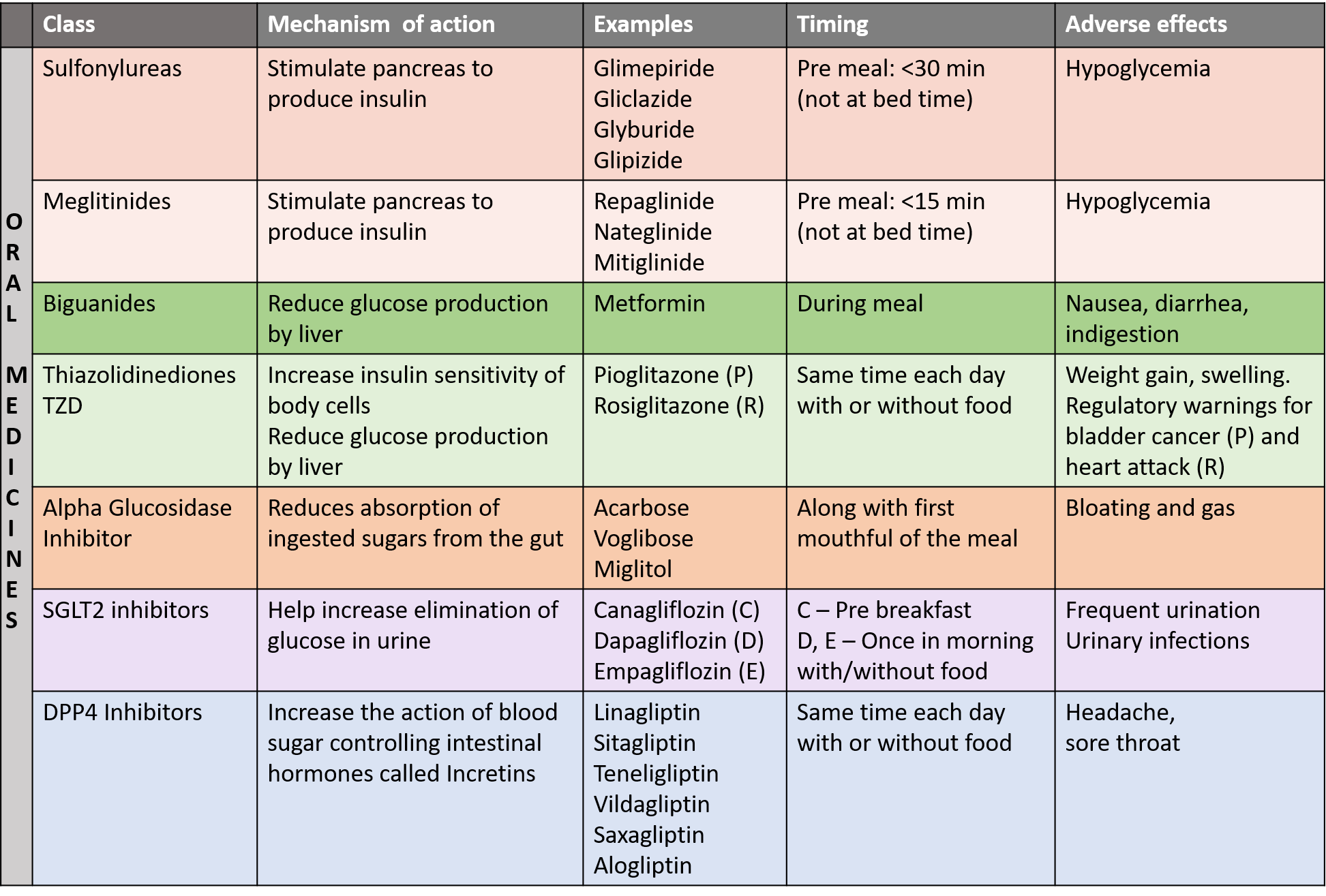
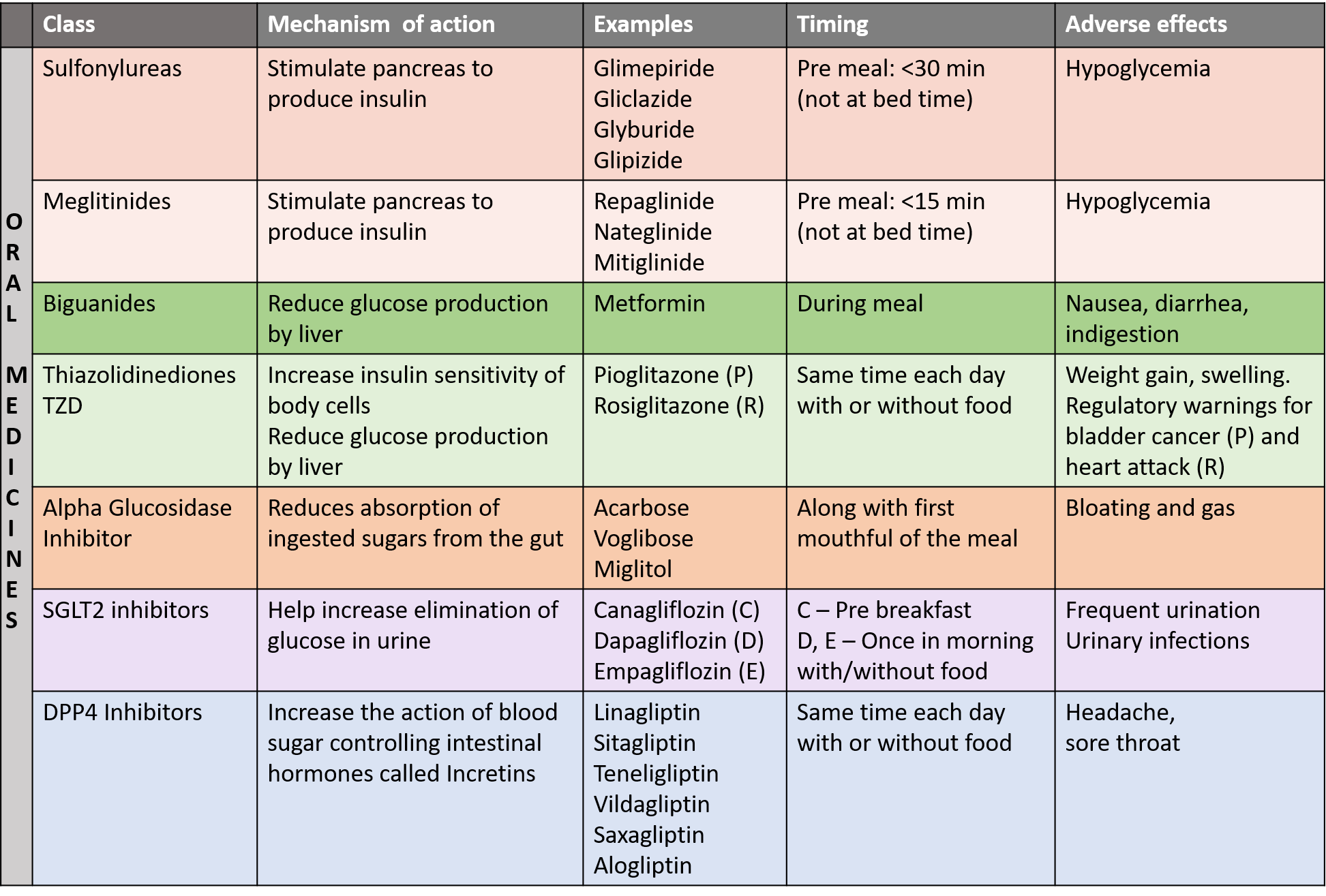
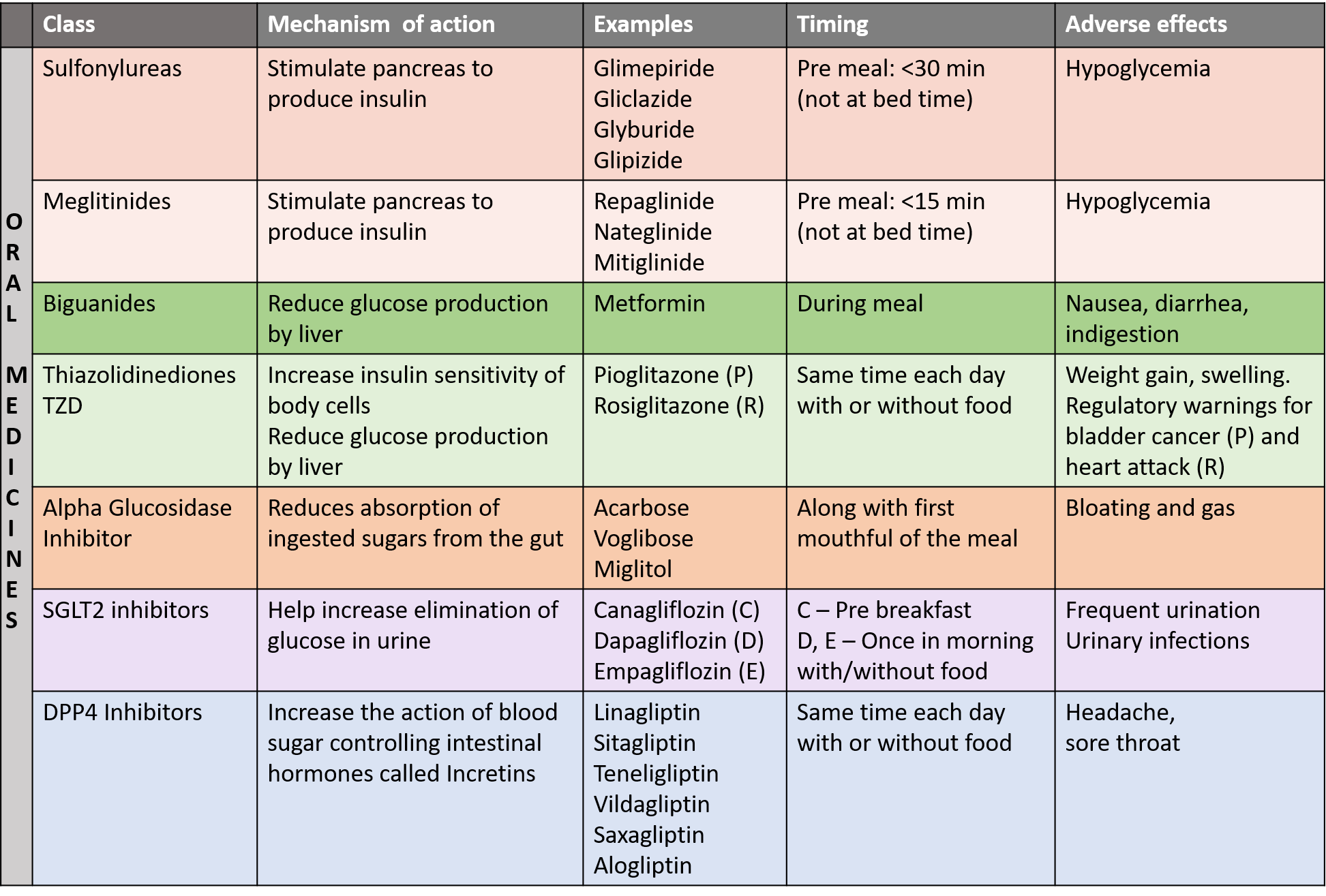
MEDICINES FOR DIABETES
They should be taken in strict accordance with dose, frequency, and relation with meals as prescribed medically. Doses should not be skipped or changed on one’s own. Dietary and lifestyle solutions have to continue with medicines also. Medicines may be prescribed singly or as appropriate combinations.
ORAL MEDICINES
New oral drugs
Lobeglitazone is a new antidiabetic drug in the thiazolidinedione class, with a lower risk of hypoglycemia (low blood sugar), launched in India in 2022. Finerenone is a new oral drug approved in July 2021 to treat chronic kidney disease in diabetes as well as reduce the risk of kidney failure and heart disease. It belongs to the class of drugs called mineralocorticoid receptor (MR) antagonists, and works by blocking the activity of certain types of steroid hormones that can damage the heart and kidneys. Imeglimin is a new oral anti-diabetic drug approved in Japan in June 2021, belonging to a new class that acts by inhibiting hepatic glucose synthesis, increasing muscle glucose uptake, and restoring normal insulin secretion. Bexagliflozin is a new SGLT2 inhibitor approved in 2023 for the treatment of type 2 diabetes (T2D) dosed once daily in the morning, with or without food.
INJECTIONS
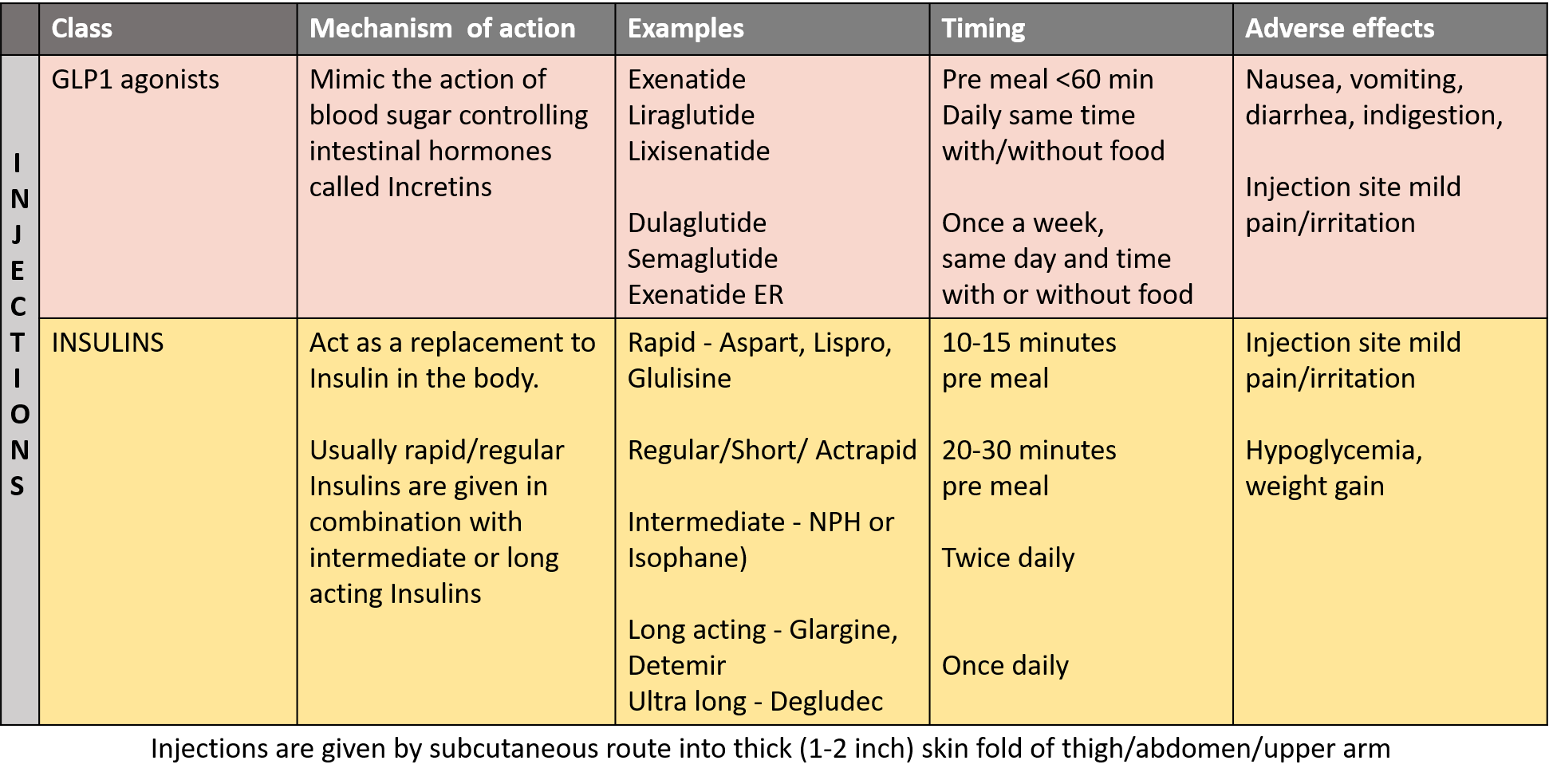
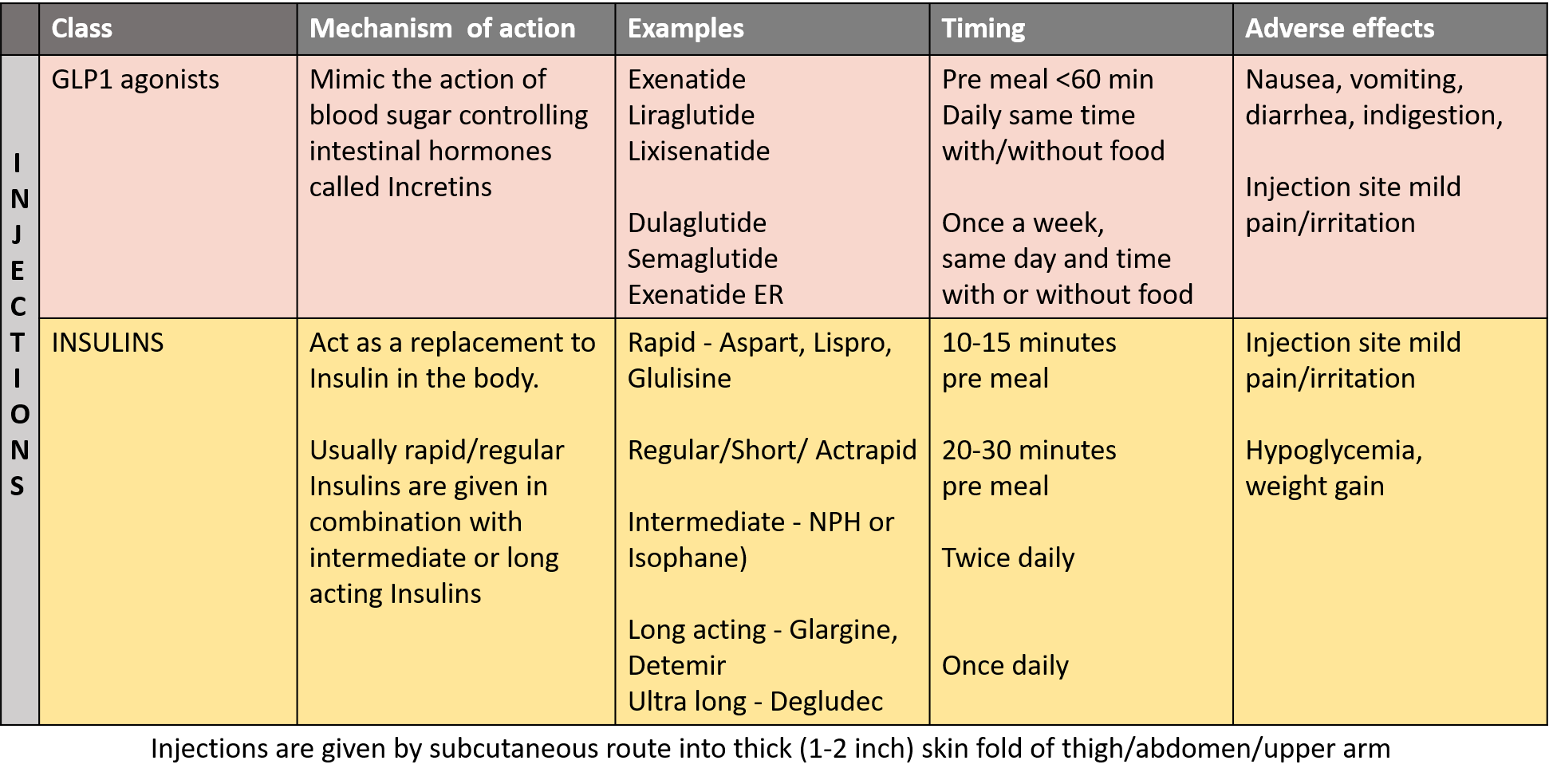
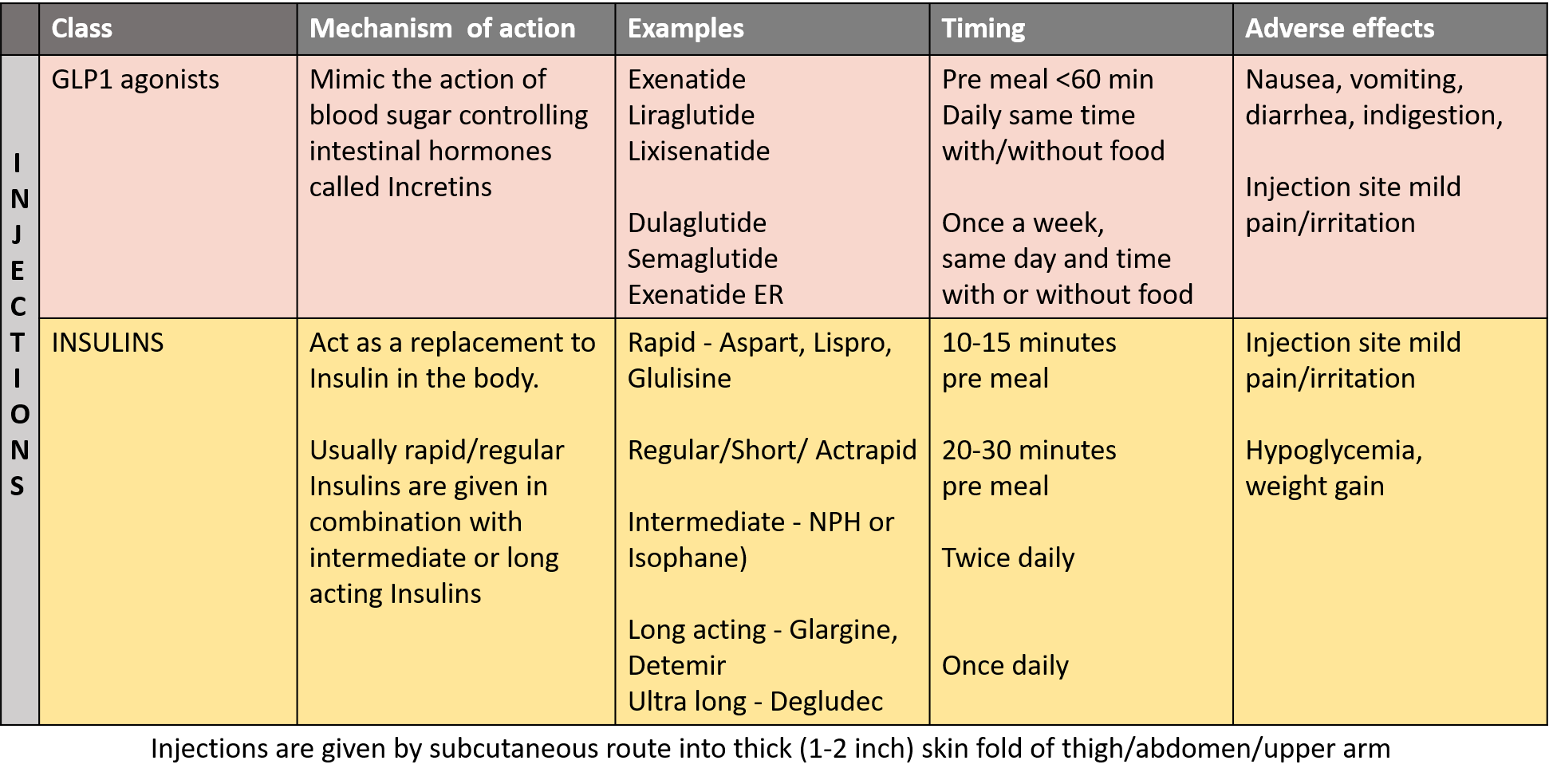
GLP1- agonists
Among these drugs, semaglutide is available as injection (which is also approved for weight management in overweight/obese) and also as oral once-daily tablet for type 2 diabetes. Tirzepatide injection is the first and only dual action GIP (glucose-dependent insulinotropic polypeptide) and GLP-1 agonist approved for type 2 diabetes as well as weight loss.
Insulin therapy
Insulin treatment is available as recombinant human insulin (regular insulin- short acting), and now as the more preferred manmade insulin analogs.
- Rapid-acting insulin analogs (aspart, glispro, glulisine) have a very fast onset of action (10-15 minutes), peak (1-2 hours) and a short duration of action (2-4 hours), as their main purpose is to prevent blood sugar rise associated with meal intake. So, they are dosed 10-15 minutes before meals.
- Regular insulin is short-acting. It starts working within 30 minutes, peaks in 1.5–3 hours, and lasts 4–8 hours.
- Intermediate insulin is prepared from rapid insulin analogs and regular insulin by precipitation with protamine peptide in a 5:1 ratio at neutral pH (neutral protamine hagedorn NPH or isophane insulin). These start working in 2–4 hours, peak in 4–12 hours, and last 12–18 hours.
- Long-acting or basal insulin analogs (glargine, detemir, and degludec) are of slow onset (2-4 hours) and have prolonged action (up to 24 hours, and >40 hours for degludec) that helps to maintain blood sugar levels between mealtimes and before bedtime (to control blood sugar outside of eating).
Diabetes treatment strategy is based on the dose being adjusted by titrating to target fasting blood glucose values of 90-130 mg/dL, post-meal blood glucose values below 180 mg/dL, and mid-morning and 2h-post-lunch or post-dinner values below 140mg/dL. According to insulin dose initiation in type 2 diabetes, it is done at around 0.3 units/kg. So, for a 60-70kg standard person, that comes to 18-21 insulin units/day, out of the total insulin 50-60% is given as basal (approximately 10 units/day).
When these mentioned sugar targets can no longer be achieved with reasonable doses of long-acting or basal insulin alone, a rapid-acting insulin analog should be added at meal times. It is recommended that initially, a single daily bolus of a rapid-acting insulin analog is administered before the meal which leads to the highest post-meal blood glucose excursions, and this particular dose can be combined with basal insulin for the day. Further boluses of rapid/short insulin can be added at other meal times as required if blood glucose is above the mentioned values.
This stepwise strategy may eventually lead to a standard basal-bolus regimen (RYZODEG 70/30 insulin degludec and aspart) before the main meal with injections of rapid-acting insulin analogs when needed before other meals, for achieving balance and sugar
Biphasic or mixed insulins that are combinations of intermediate NPH with regular insulin (70/30 and 50/50) and with rapid insulin analogs (like lispro, aspart) as protamine suspensions (lispro protamine/lispro 75/25) are also available for better blood sugar control.
Insulin icodec, an ultra-long-acting basal insulin analog recently developed, has the advantage of requiring only a once-weekly subcutaneous injection, a significant reduction from the once- or twice-daily injections of other basal insulins. Insulin icodec is engineered with a fatty di-acid side chain and amino acid substitutions, allowing it to bind strongly and reversibly to albumin in the bloodstream. This creates an inactive, circulating depot that slowly releases active insulin over a full week. It has received marketing authorization in the European Union, Canada, Australia, and Switzerland for the treatment of diabetes in adults. In type 2 diabetes, it can be used alone or in combination with other non-insulin medications.
Ultra-rapid-acting inhaled insulin is also now available for type 1 and 2 diabetes.
Combination drugs with Insulin.
Lixisenatide is the latest once-daily GLP-1 agonist (drugs that mimic the action of hormones called incretins) approved for treating patients with type-2 diabetes and is also available in combination with Insulin glargine. It has an onset of action of about 1 hour and a duration of action of 4-5 hours, so it is an in-between for rapid and basal insulin. Soliqua 100/33 (insulin glargine/lixisenatide) is used in those who prefer morning dosing and are non-compliant to immediate premeal dosing. It is given once daily, around an hour before breakfast or on rising in the morning. Additional rapid insulin may be given pre-dinner if needed. Insulin degludec is also available in combination with the drug liraglutide.
As mentioned, all medications for diabetes should only be taken under the prescription and guidance of the treating physician.
In type 2 patients controlled on oral medicines, insulin may be prescribed if blood sugar levels are very high at initial presentation, during acute stress periods like surgery/hospitalization, and severe weight loss, especially in the elderly, or due to inability to tolerate side effects of medicines, inadequate sugar control with medicines, and in compromised liver or kidney function.
Self-Monitoring and Continuous Monitoring of Blood Glucose
Regular blood sugar monitoring is most important and patients may also be recommended SMBG (Self Monitoring of Blood Glucose) by home-based/portable glucometers on a daily basis, or certain days of the week. SMBG can help to show whether your medicines are working well, adjust insulin dosage, and also determine personalized glycemic responses.
The latest technology available is CGM-Continuous Glucose Monitoring which is non-invasive and enables one to know the sugar levels anytime along with trends and ranges over time. CGM devices measure the glucose level in the interstitial fluid (fluid between cells), just under the skin 24 hours a day while wearing the device. The CGM device has a sensor (usually a small pellet) that is inserted under the skin with an applicator to measure glucose levels. A transmitter wirelessly sends the glucose data from the sensor to a device where it can be viewed. Smart phone app or receiver displays the real-time glucose level and shows graphs of up-down trends and the history of previous levels. Some CGMs connect with insulin pumps to offer automated and measured insulin delivery.
Hypoglycemia or a sudden drop in blood sugar may happen occasionally but is rare with regularity, monitoring, and accuracy of taking medicines. One must have glucose powder/tablets handy if experiencing dizziness, shivering, ringing, sweating, hunger, palpitation, extreme irritability or anxiety-nervousness.
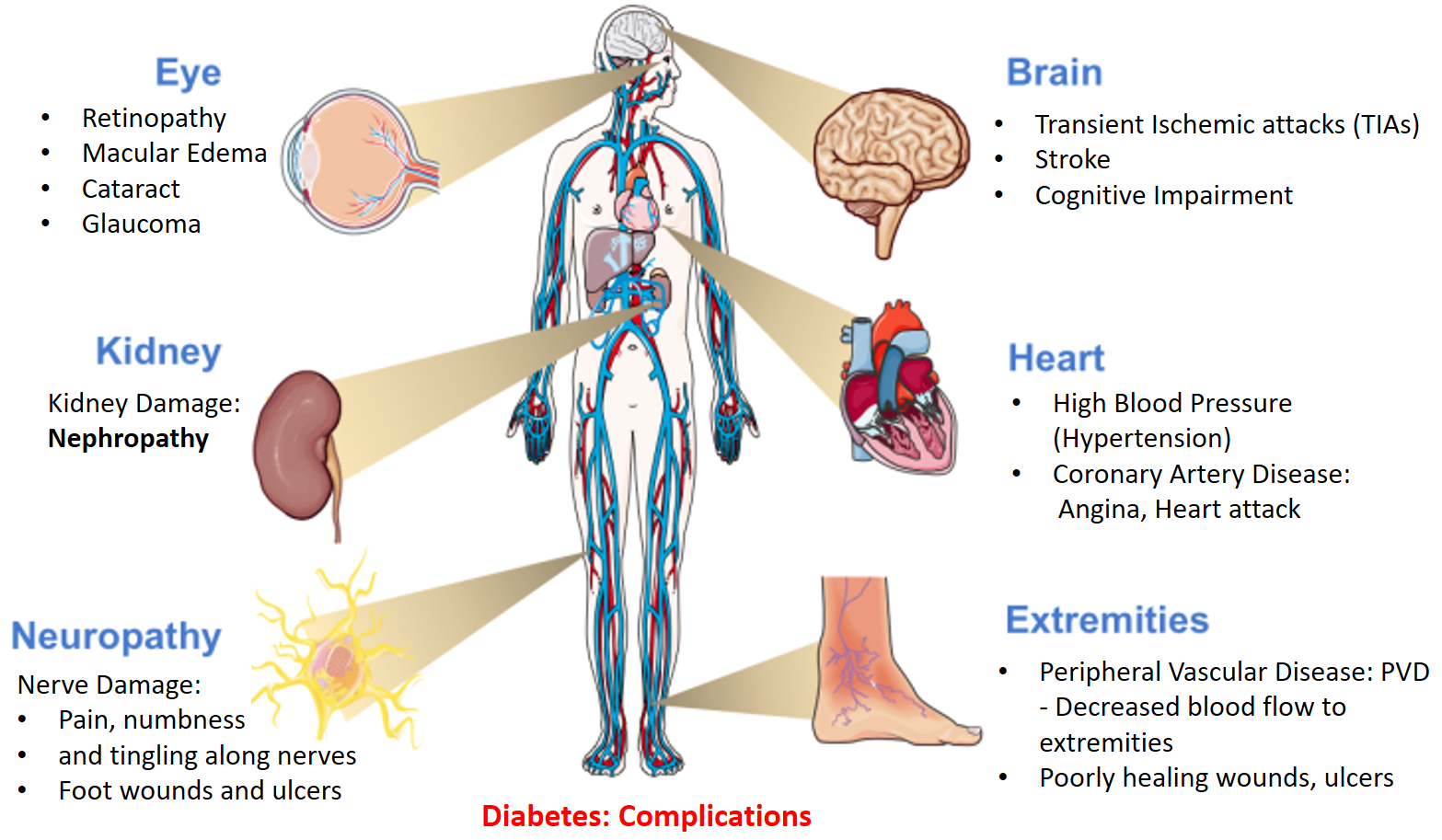
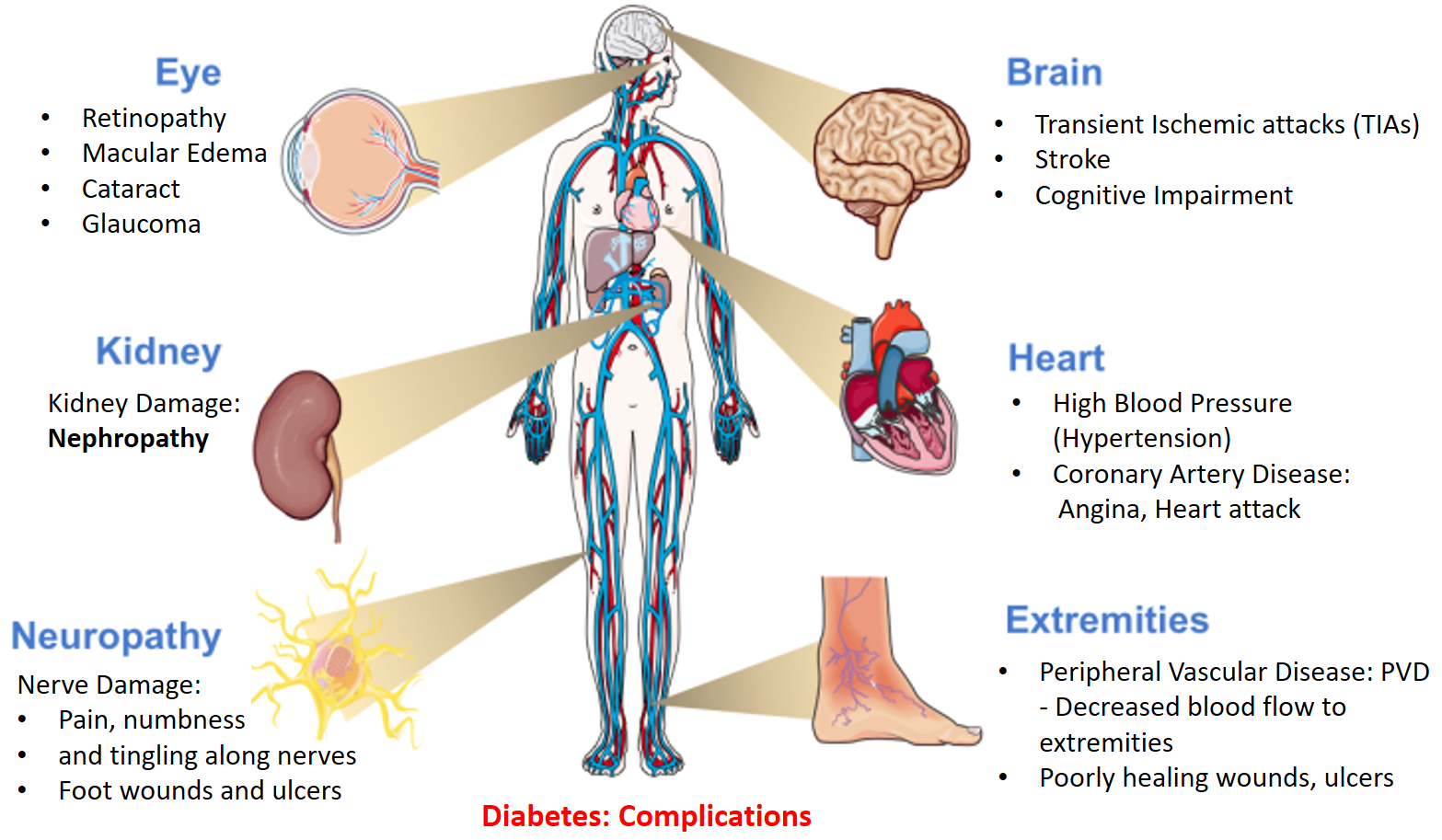
COMPLICATIONS
An increase in blood glucose over a period of time can cause damage to blood vessels and the nerves, resulting in complications most prominently Cardiovascular disease (CVD), Nephropathy (Chronic Kidney Disease), Neuropathy and effects on the Eye. Therefore, patients should undergo regular eye examination (including retina), blood pressure measurement, kidney function tests, lipid profile, and health assessment follow up checks along with blood sugar and HbA1C tests.
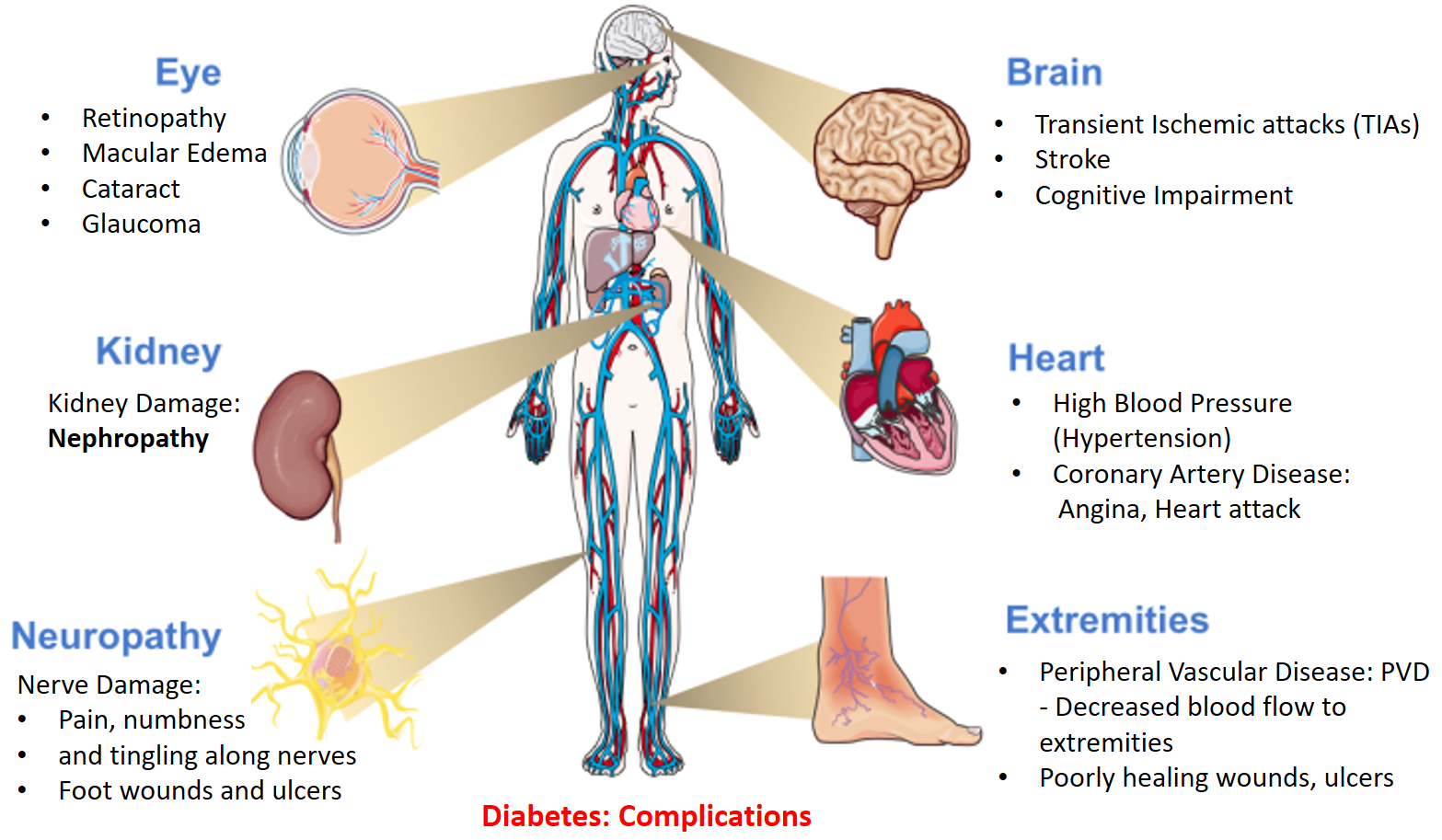
A dangerous complication called Diabetic Ketoacidosis, a medical emergency can occur due to excessive breakdown of fat by the body cells (in the absence of utilizing glucose) and release of acidic substances called ketones in the blood. This is seen more in Type 1 and is rare in type 2 diabetes as there is still some functioning insulin and glucose utilization. Symptoms include nausea, vomiting, abdominal pain, confusion, thirst-hunger, dry mouth, rapid breathing, urination, and a fruity breath odor along with high sugar and ketones in the blood.
Diabetes is a major risk factor for COVID-19. People with diabetes have a higher risk of developing severe COVID disease requiring hospitalization or ICU care, and also have a higher rate of both complications of Diabetes and COVID. Meticulous blood sugar monitoring and control is crucial during such pandemics.
Also read –
Incorporating the DASH diet to reduce BP, BMI and Cardiovascular risk
For any query, additional information or to discuss any case, write to info@drvarsha.com, and be assured of a response soon.
References


