Constipation is the difficulty in passing stool, which includes infrequent bowel evacuations, straining to pass stool, hard or lumpy stools, prolonged duration to evacuate, or a feeling of not having evacuated fully or adequately.
Quick read – 5 Dietary Tips to reduce Constipation
Everyone goes through such episodes once in a while but when this is present for most days in the month, for at least 3 months or longer, the person is said to have chronic constipation. Most international definitions (like Rome criteria), label chronic constipation as <3 bowel evacuations in a week but this may be a drastic cut off for many populations (like India), where at least one bowel evacuation daily is commonly seen. Constipation often leads to a feeling of abdominal discomfort, bloating, cramps, appetite loss and decreased well-being.
RISK FACTORS
The risk of developing constipation increases with age (risk doubling >75 years) due to the weakening of muscles and decreased physical activity. Women are 3-4 times at higher risk of developing constipation. Constipation is more common in Asian and African ethnicity.
Lifestyle factors such as type of diet (decreased fiber and increased processed items), low fluid and water intake, physical inactivity and sedentary lifestyle, improper bowel habits, psychological stress and intake of certain substances/medicines, all can lead to the development of constipation. Long-term illnesses and weakness, or prolonged bed rest due to surgeries/illnesses also predispose to developing constipation.
TYPES OF CONSTIPATION
These are based on the probable cause and mechanism of constipation.
Normal transit constipation
Also called functional constipation, here the bowel movements and the transit time of stool is normal. Constipation occurs due to reduced bulk of stool (seen with low fiber and fluid intake), suppressing urge or avoiding to pass stool (rushing to work/busy schedules, avoiding unpleasant/unhygienic toilets) or if there is a painful body condition making one avoid sitting for passing stools (hip/knee arthritis, injuries, recurrent boils, fissures in the anus, breathlessness on sitting/straining, etc.)
Slow Transit Constipation
Bowel movement (motility) has decreased leading to the increased transit time of stools in the large intestine. This is the result of the reduced contracting ability of the abdominal and bowel muscles as seen with ageing, injuries/trauma, nerve-related diseases, hormonal imbalances- pregnancy, and certain drugs/medicines. Sometimes the reduced motility maybe even seen throughout the gut leading to symptoms of dyspepsia (like acidity, bloating, abdominal fullness) along with constipation.
Dyssynergy of Muscles
Even though the strength and contracting ability of muscles may be intact, there may be in-coordination in their action. For effective bowel evacuation, muscles of the abdomen (area just below the chest around the belly button/navel) contract, while the pelvic floor (a group of muscles supporting the lower organs like urinary bladder, large bowels, and uterus) and the anal sphincter (a ring-like group of muscles surrounding the anus, controlling stool release) relax, in synergy. Such absence of synergy and coordination may occur due to trauma and injury to the local muscles and nerves which could happen during childbirth, sexual abuse, accidents, and spinal cord injuries. Such patients may have additional symptoms like urinary complaints (frequency, pain or leakage), pain in lower back or area of genitals, or pain during intercourse. Constipation for such people is typically a feeling of incomplete evacuation even after prolonged strain.
In those with nerve injuries and reduced sensations, the desire/urge to pass stool may not be appreciated consciously leading to enlargement (dilatation) of the large bowel/rectum and accumulation of stools (called megarectum/megacolon).
Mechanical obstruction to the passage of stools
It is important to rule out a local partial (stenosis) or complete obstruction (stricture and stenosis) which prevents stools from passing out. Such cases usually present with almost sudden and complete constipation and a feeling of stools getting stuck. This happens due to inflammation and scarring following injury, ulcers, infections (like STD, TB), instrumentation/surgery/radiation. A tumor or cancerous growth is a cause to be explored in elderly patients presenting with sudden constipation, accompanied by weight loss, and blood loss in stools or presence of paleness/anemia. Sometimes a hard piece of stool (fecal impaction) may cause obstruction. There may sometimes be localized ‘pouches’ which accumulate the stool and cause obstruction (rectoceles).
Secondary to other diseases
Constipation can be one of the manifestations of several body diseases, therefore, it is wise to enquire or look for symptoms of these conditions and treat the primary cause along with managing constipation per se. These include metabolic conditions like diabetes, thyroid disorders, imbalances in calcium, magnesium or potassium levels, increase in blood urea due to liver disorders, neurological conditions like Parkinson’s, multiple sclerosis or post-stroke, and in heavy metal poisoning (like from seafood, occupational/industrial).
Many medicines can cause constipation as included in this list and constipation usually settles down on stopping or eliminating their intake.
Irritable bowel syndrome (IBS)
This is a bowel condition comprising of abdominal pain as hallmark symptom, related to (relieved or brought on by) passing of stool, accompanied by a change in form and frequency of stool. The cause is related to disruptions in the gut-brain connections whereby there may be alterations (increase or decrease) in the sensitivity of the gut to stretch/food, gut motility and transit time, and amount of fluid absorbed from or secreted into the gut. Therefore, IBS can present as abdominal pain with constipation (50% cases IBS-C) or with diarrhea (IBS-D) or a mixed type (IBS-M) with alternate diarrhea and constipation.
Sometimes sensitivity to a substance called gluten found in wheat products can also cause constipation with or without alternating diarrhea and other abdominal symptoms.
HEALTH SOLUTIONS
Constipation is not only a distressing condition affecting quality of life, but can also increase the risk of conditions like hernia and piles (hemorrhoids). Therefore it should be treated in a timely and effective manner.
Diet
The general principles are to include more fiber like whole grains, vegetables and fruits, and less processed and refined food. This is also the key to general good health, weight, sugar and fat management, and keeping many lifestyle and metabolic conditions at bay.
Fibers (Roughage) – These may be insoluble (remain unchanged in the gut but add bulk to the stool to help it move more easily) or soluble (absorb water, swelling into a gel making the stools move slowly but steadily and smoothly). A balanced mix of insoluble fibers (whole grains, wheat bran, brown rice, prunes) and soluble fibers (oat bran, beans, lentils, peas, and flaxseeds) should be incorporated in the diet. Vegetables and fruits are good sources of both insoluble and soluble fibers with the former being more in the outer skin, peel and leafy parts and the latter more in the inner fleshy parts. Fruit like apples, pears, citrus fruits, and berries have good amounts of soluble fibers while tomatoes, nuts, raisins, grapes have good amounts of insoluble fibers. Figs are a great balanced source of both fibers.
Soluble fibers provide additional health benefits like managing cholesterol, sugar, and weight. Some of these fibers are fermented by gut bacteria to additional useful products, but the byproduct gases liberated may temporarily aggravate the feeling of flatulence, bloating or abdominal discomfort especially in IBS patients. This may also be experienced with too much insoluble fiber intake increasing stool bulk. Therefore, fiber intake should be kept to around 20-25g/day in women and 30-35g/day in men out of which 25-30% should come from soluble fibers. The fiber content of the food should be gradually raised. IBS patients should especially avoid FODMAP foods in their diet.
Water and Fluid intake – At least 1.5 to 2 liters/day is the recommended norm (this does not include beverages/other drinks). Beverages/alcohol/aerated and carbonated drinks should be kept to a minimum). Alcoholic, sugary, aerated and carbonated drinks should be avoided/restricted as they increase the tendency to constipation. A morning warm/hot milk, coffee or tea works well to stimulate bowel movement, but it is advisable to restrict them later in the day or evening as they are likely to constipate the next day. Fruit juices work well for people with a tendency to constipation.
Constipating food items – These include meats, cheese, butter, fried foods, frozen foods, ice creams, processed grains and foods, high salt foods, and sweetened sugary food items (cookies, cakes, pastries, etc). Unripe bananas tend to constipate so go for ripe bananas that have a good amount of soluble fibers.
Yogurt is very beneficial for constipation as well as to maintain gut bacteria (probiotics). Olive oil has a mild laxative effect so is a good option to use for cooking for constipated people.
Lifestyle
A few habits go a long way to improve functional constipation. It’s prudent to ensure adequate time for passing stool by setting time for waking and not suppressing the urge to go to the toilet.
Include half an hour of exercise (5 days/week) in your lifestyle – swimming, brisk walking, cycling, jogging, yoga, or aerobics. If sitting for prolonged periods of time, take a short walk and do some stretching every 2 hours. Squatting exercises help to build abdominal muscle strength and aid in managing constipation.
The brain and gut have an intricate connection, so stress or depression can lead to the release of chemical mediators which increase the acid release and slow down gut movement. Including de-stressing and relaxation techniques in daily routine like deep breathing exercises, indulging in hobbies like reading, music, dance, crafts, gardening, and sports, can also contribute to smooth bowel functioning.
MEDICINES FOR CONSTIPATION
Laxative medicines are recommended in chronic and resistant constipation and are best used after medical consultation and investigations which may include blood and stool testing. A colonoscopy may also be performed to rule out certain causes, and sometimes specific tests for gluten sensitivity or lactose intolerance may be advised.
The following are the laxatives medicines, and even though many are available over the counter, it is best to start in accordance with medically recommended amount and duration. Irregular, inappropriate or overuse of laxatives can actually worsen the symptoms or condition in many people.
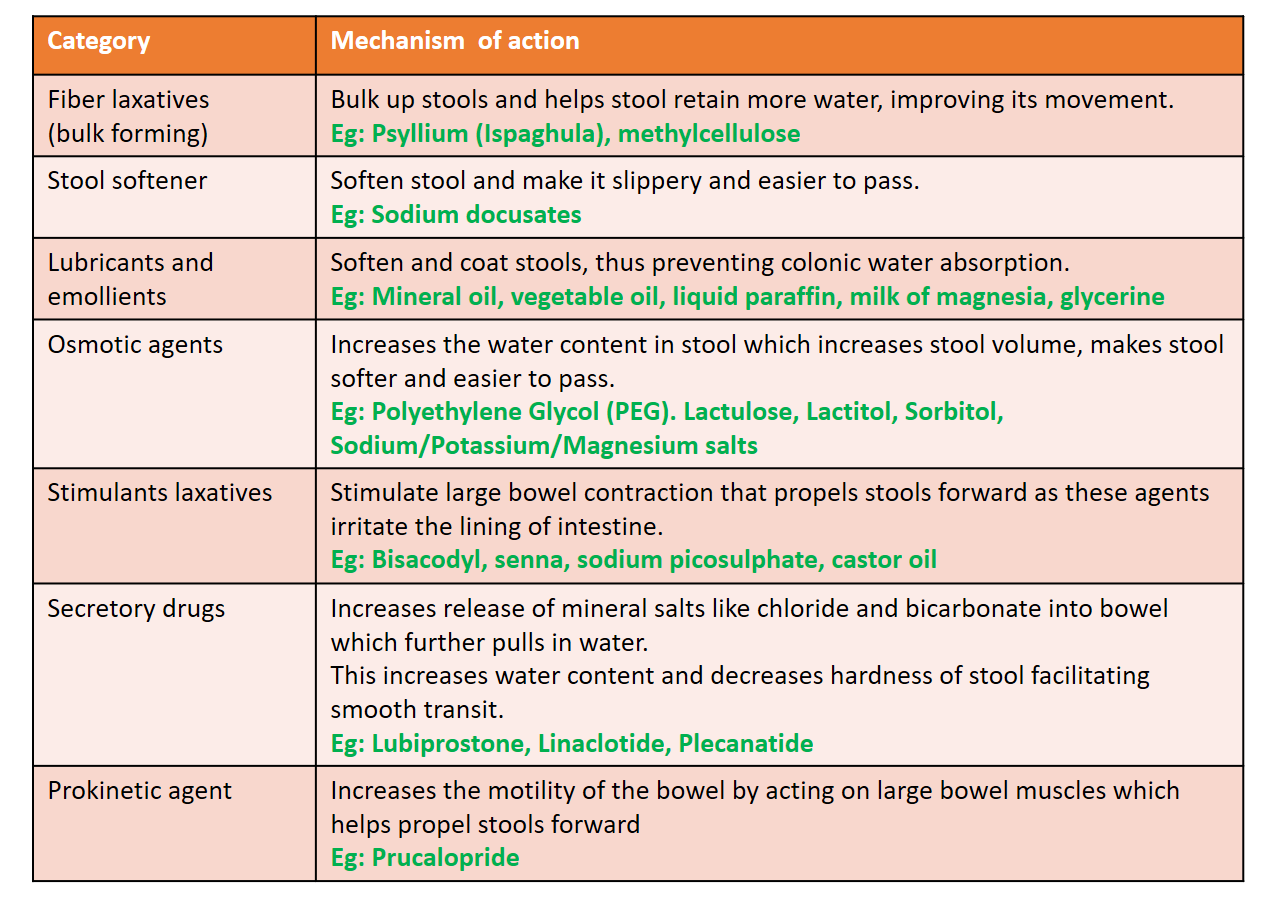
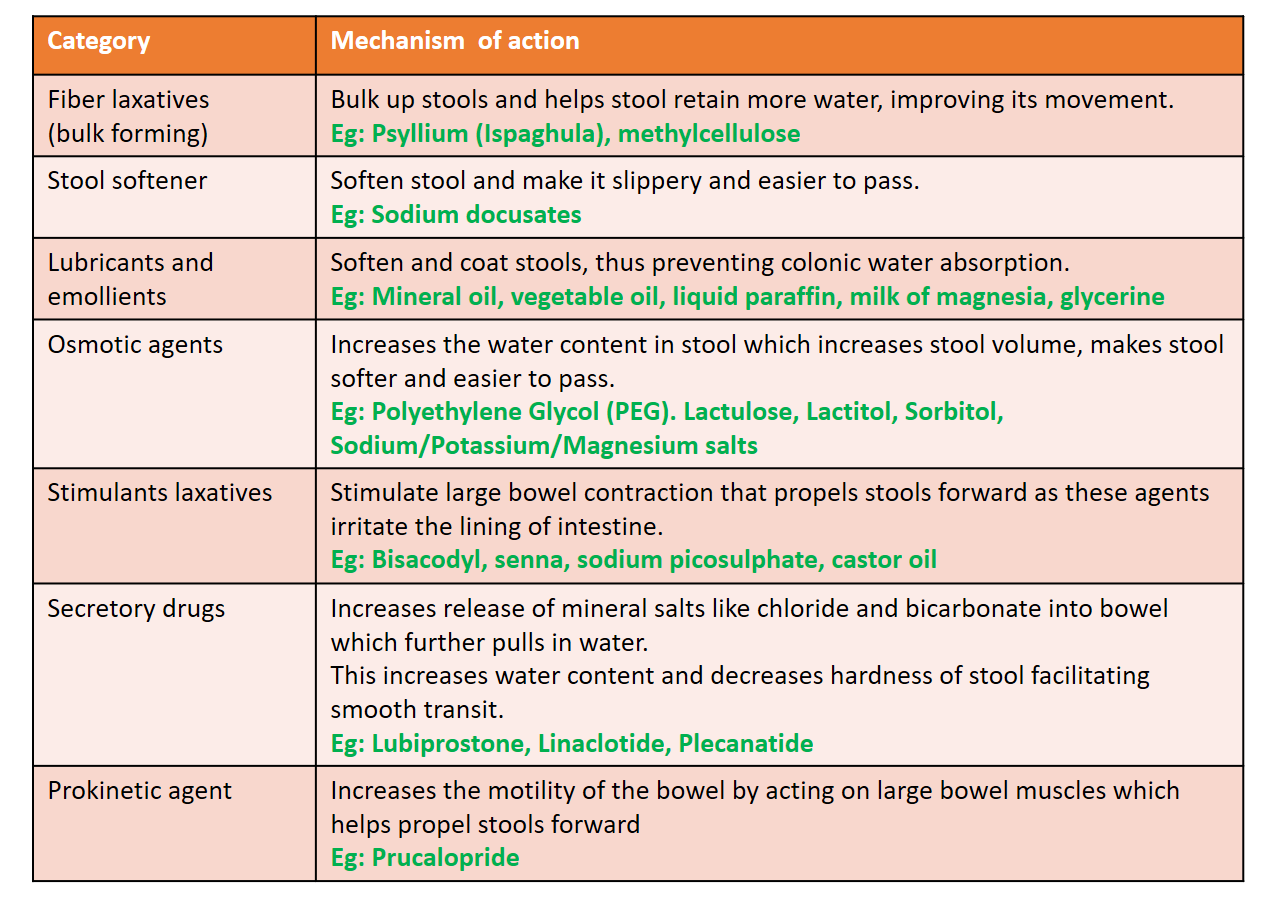
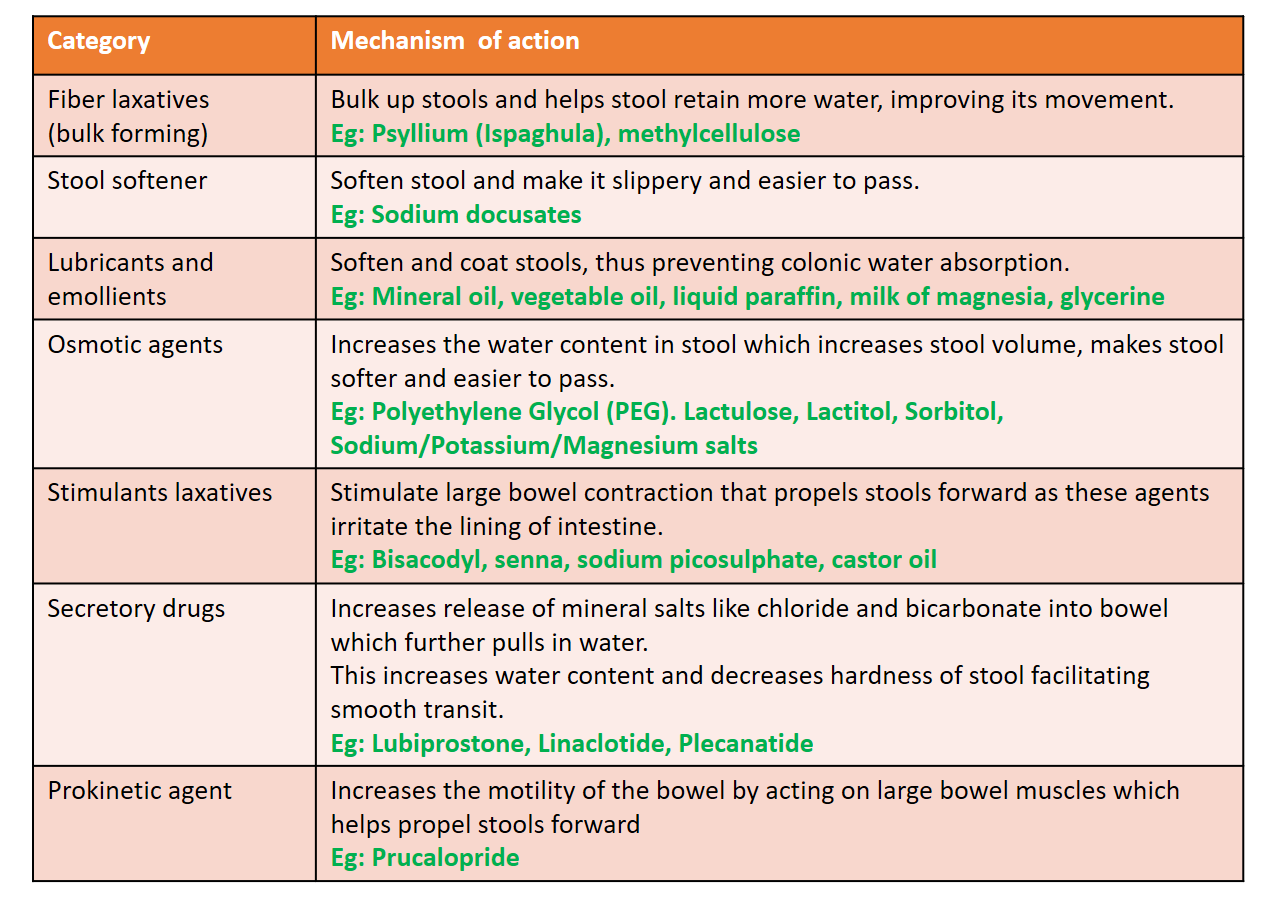
A combination of laxatives is also available (Ispaghula+Lactulose, PEG+Ispaghula, Milk of Magnesia+Liquid paraffin, etc). They are available as powders, liquids, and capsules. They may be used as an enema through the anus in a hospital setting for emptying bowel before surgery/procedure or in acute severe constipation.
Some of the side effects of laxative medicines include nausea, bloating, abdominal cramps, diarrhea and imbalance of mineral salts in the body. Palatability is also an issue that is often solved by flavoring the powder and liquid preparations. In elderly leakage of stools (fecal incontinence) maybe a disturbing side effect. Many of the over the counter preparations start to reduce in effectiveness over a period of time in chronic constipation cases, and need for larger and multiple doses may arise. Newer drugs like linaclotide/plecanatide (yet to be launched in India) and Prucalopride have shown effectiveness in chronic constipation not responding satisfactorily to conventional laxatives, and also has the advantage of once-daily dosing.
Further reading –
For any query, additional information or to discuss any case, write to info@drvarsha.com and be assured of a response soon.
References


