CARDIOVASCULAR DISEASE (CVD)
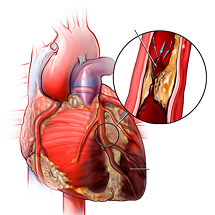
Cardiovascular disease refers to a group of conditions occurring as a result of blockage of blood vessels (more specifically arteries), due to atherosclerosis and clots, impacting the heart and other organs. CVD is also known as atherosclerotic cardiovascular disease (ASCVD).
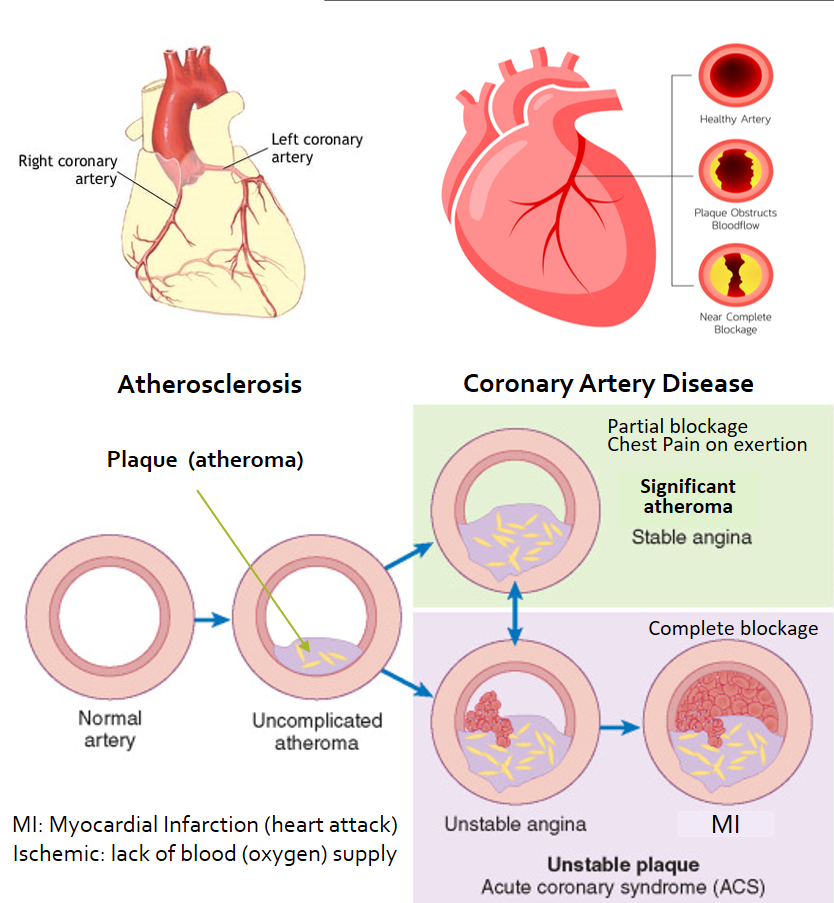
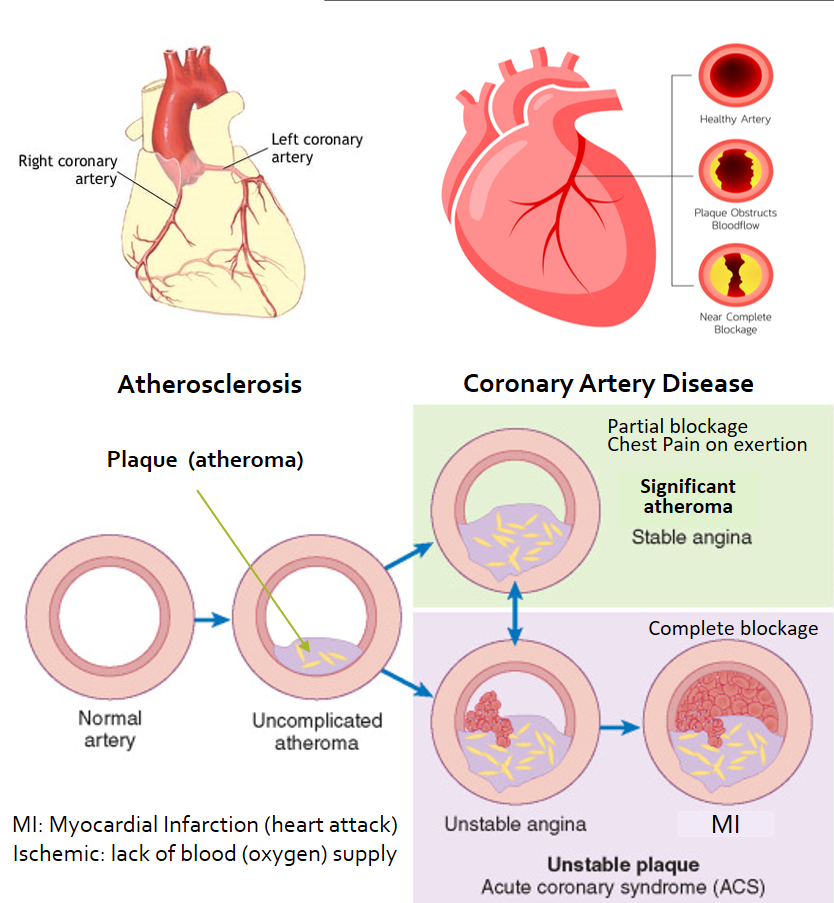
Atherosclerosis (or arteriosclerosis) refers to the buildup or formation of ‘plaques’ in the arteries that carry oxygen-rich blood to all the body organs. These plaques (also called atheroma) are made up of fats, cholesterol, calcium, and some blood cells mainly platelets. These occur due to damage to the artery wall (endothelium) due to high blood pressure, high sugar (diabetes), smoking, and high LDL-cholesterol/triglycerides. These plaques can cause a partial blockage of the arteries, and stiffening of its walls. Atherosclerosis can also lead to further endothelial damage, and the plaque itself can rupture resulting in clot formation (thrombosis) which can cause a sudden complete blockage of that artery.
Ventricular hypertrophy is the thickening of the walls of a ventricle of the heart due to increased work-load, often seen in the elderly, and in those with high BP, coronary artery disease, or after a heart attack. Left ventricular hypertrophy is more common than right but concurrent hypertrophy of both ventricles can also occur.
CVD risk factors include –
- Diabetes
- Hypertension (High Blood Pressure)
- Kidney disease
- Dyslipidemia (increased cholesterol +/- triglycerides in the blood)
- Lack of physical activity (sedentary lifestyle)
- Obesity or being overweight (high BMI)
- Inappropriate diet (high carbohydrate/sugar, salt and/or saturated/trans-fat intake)
- Psychosocial stress
- Smoking/tobacco use
- High alcohol consumption
- Family history of cardiovascular disease, and/or hypertension.
- Recently suffered from COVID
- Asian and African race
- Sleep apnea
- Male gender and increasing age represent an overall higher CVD risk as compared to women and younger age. However, women who smoke, have diabetes, psychosocial stress or depression are a higher risk group as compared to men with the same risk factors.
- Additional risk factors in women include menopause, oral contraceptives use, and hypertension or diabetes in any of their pregnancies.
When blood flow (and therefore oxygen supply) is reduced to the heart, it is called Ischemic Heart Disease (IHD) as ischemia means lack of oxygen. It is also called Coronary Artery Disease (CAD) caused by blockages in the coronary arteries which supply the heart. If more than 50% of any coronary artery is blocked, it is called ‘obstructive’ CAD.
Angina
The lack of adequate oxygen supply to any part of the heart leads to a lack of functioning of that part, and heart pain called ‘angina’.
Stable Angina
In people with obstructive CAD, the heart may continue to get enough blood and oxygen at rest or during normal activities. But during exertion, stress, exercise, or illness, there is a need for more oxygen and therefore more powerful pumping of the heart. At this time there may be inadequacy in blood and oxygen supply to parts of the heart muscles (which do the pumping action), due to the artery blockages. This results in heart pain (angina). Stable angina is relieved with rest and giving medicines (nitrate drugs) that further dilate these partially blocked arteries to increase blood flow and cope with the increased oxygen demand of the heart.
Unstable Angina
Sometimes a plaque causing partial obstruction of the artery ruptures periodically and the resulting blood clot may majorly obstruct the blood supply to a portion of the heart. Such plaques are called unstable plaques. Since this can happen at rest or even on mild exertion, it is unpredictable and called unstable angina. This kind of angina is not relieved by rest, and even the nitrate dilators may relieve the pain incompletely or inadequately.
Myocardial Infarction
When a complete or almost complete blockage is present in any coronary artery, it can stop the blood flow and oxygen supply to a part of the heart. This causes damage to the cardiac muscles, (myocardium) and the condition is called Myocardial Infarction (MI) or Heart Attack. MI causes severe heart pain, and this pain is not relieved either by rest (can even occur at rest) or by dilating medicines. (MI is further classified into ST-segment elevation- STEMI and Non-ST-segment elevation- NSTEMI, based on changes seen in ECG).
Unstable angina and MI are together called Acute Coronary Syndrome (ACS). The pain usually lasts more than 10 minutes, compared to the usual 2-5-minute duration seen with stable angina. The pain is like a squeezing or tightening sensation in the chest which may radiate to the jaw, neck, arm, shoulder, and back. Often symptoms of anxiety, like breathlessness, lightheadedness, sweating, and nausea may be associated. Sometimes the pain may not be so typical and get dismissed as indigestion or gas, so it is best to do an ECG in case of the slightest suspicion.
It may be hard to clinically differentiate unstable angina and MI. ECG changes and rising cardiac enzymes in the blood (markers of MI) can help establish the diagnosis. ACS especially MI is one of the most common causes of cardiac arrest or sudden cardiac death.
MANAGEMENT OF CVD
Risk assessment and Medical evaluation
Angina or MI can be the first manifestation of CAD, therefore it is important to have your BP, blood lipids (triglycerides and cholesterol), and sugar checked regularly if you have any of the risk factors mentioned above, or are more than 45 years (male) or 55 years (female) years of age. You may be advised further tests like ECG, 2D-echocardiography to assess cardiac function, and cardiac CT-angiography to diagnose the extent of blockage of arteries.
It is important to note here that seemingly very fit individuals without known or obvious risk factors, who are into high-intensity weight training and workout regimes may also have underlying CVD or CAD. They are at an even higher risk of angina and MI due to the sudden and high demands placed on the pumping action of their heart and oxygen supply. Therefore anyone engaging in such activity should have these mentioned tests done initially and periodically.
Healthy diet
Reduce packaged foods, and foods high on salt, trans/saturated fats, and sugar. Switch to a healthy diet that has more fresh foods, fruits and vegetables, and whole grains, which can also help maintain appropriate weight and BMI.
Healthy lifestyle:
This should include stress management, stopping smoking, and reducing alcohol intake (to not more than a glass daily). There should be adequate physical activity that should include 30-45 minutes of exercise like brisk walking, swimming, yoga, aerobics, cycling, etc. at least 5 times/week. An uninterrupted sleep of 8 hours on most nights is very important. Take out half to 1-hour of relaxation time daily to spend with family, pursue a hobby, including a few minutes of breathing exercises like pranayama and meditation.
Medicines
Treatment of high BP and diabetes with regular medicines, monitoring and follow-up are most important. In addition, to reduce plaque formation, medicines to lower cholesterol/triglycerides, and prevent clots (thrombosis) in the arteries (antiplatelet drugs like aspirin, clopidogrel, ticlopidine) are prescribed. In very high-risk cases especially those with past history of MI or stroke, or associated heart failure, anticoagulant medicines (rivaroxaban, apixaban) may be given along with antiplatelet agents.
Emergency treatment
Treatment of an acute coronary episode requires immediate hospitalization (preferably in a 1-hour window) and timely treatment with thrombolytic medicines that break down a clot (alteplase, streptokinase, etc.) as well as long-term blood thinning/anti-platelet medicines. Interventions on the blocked vessels include angioplasty with stenting or bypass grafting depending on the type and extent of blockages. Risk factor management and dietary modifications would always be needed lifelong.
CVD EFFECTS ON OTHER ORGANS
Apart from coronary artery disease (CAD) and ischemic heart disease (IHD), CVD also affects vessels of the brain (cerebrovascular disease) that can lead to transient ischemic attacks (TIA) and stroke.
CVD can also affect arteries of the limbs (peripheral arterial disease – PAD, or peripheral vascular disease – PVD), and the kidney (atherosclerotic reno-vascular disease ARVD), leading to chronic kidney disease.
Also read:
High Blood Pressure (BP) – Risks and Solutions for Hypertension
Diabetes: Understanding health risks and effective diet-lifestyle measures
For any query, additional information or to discuss any case, write to info@drvarsha.com and be assured of a response soon
References
2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease