BLOOD PRESSURE AND ITS MEASUREMENT
Blood pressure (BP) is the pressure that blood flowing in our arteries exerts on the vessel wall. Arteries are blood vessels that carry blood rich in oxygen from our heart to different parts of the body.
This pressure is maximum (systolic BP) when the heart contracts on the heartbeat and ejects the blood into the artery (aorta). The pressure is lowest (diastolic BP) in between heartbeats. Therefore, blood pressure is expressed in the units of mm of mercury (Hg) as a fraction of systolic upon diastolic BP (example – 120/80 mmHg).
Blood pressure measurement should be performed by a BP machine with appropriate cuff size and calibration.
For any BP measurement, you should be at rest for at least 5 minutes (with no exercise, smoking, or coffee intake 30 minutes prior). Preferably pass urine before a BP measurement.
BP is measured while sitting relaxed and comfortably on a chair preferably having a backrest, with feet flat on the ground. The BP instrument and your arm are rested on the same table at level with your heart. BP if being measured lying down should be done with the BP machine level beside you. Sitting BP is usually 5-10 mm more than lying (supine) BP while standing BP is the lowest. If you have a tendency for dizziness, your difference between sitting and standing BP should be measured.
DEFINING AND STAGING HIGH BP (HYPERTENSION)
Hypertension classification based on BP measurement has been defined by the 2020 International Society of Hypertension, American Heart Association and American College of Cardiology. Hypertension classification and its guidelines are also given by the European College of Cardiology and the European College of Hypertension. There are differences in the classifications in terms of defining hypertension and the terminology used, as shown below.
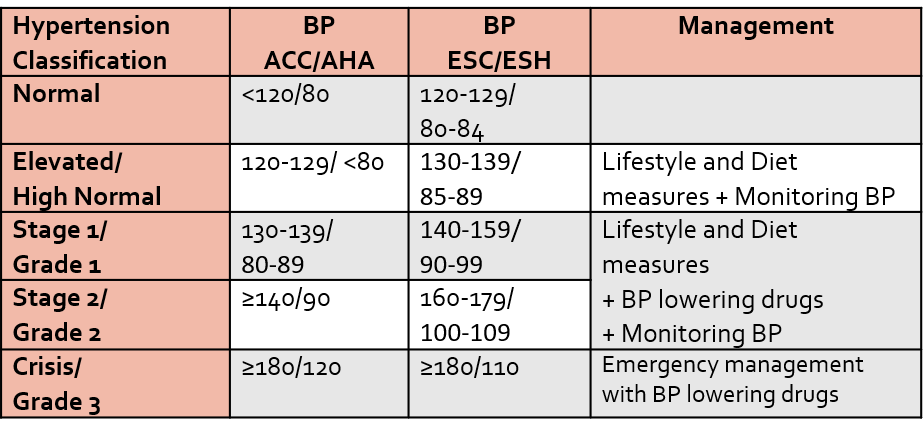
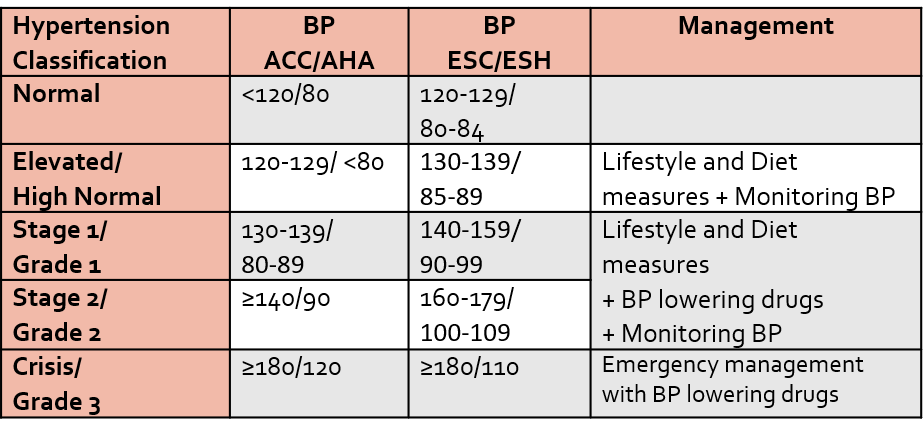
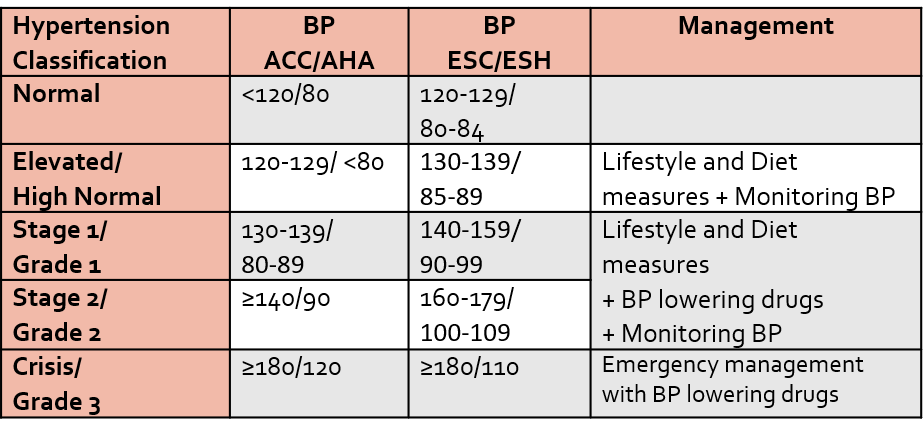
It is to be emphasized that a single BP reading is not diagnostic and is not used for decision-making. If the first visit BP reading is high it should be rechecked again (after 1-2 weeks for BP between 160/100 to 179/109 and 2-4 weeks for BP between 130/80 to 159/99). At least 3 consecutive BP readings over 3 different visits should consistently show raised readings to diagnose anyone as having hypertension. The classification of hypertension followed depends on the country and its accepted national guidelines.
If the BP reading is 180/110 or higher at any visit, it is treated as an emergency and will need to be immediately managed medically.
Also, the cut-offs mentioned so far are for in-clinic BP measurement. Sometimes self-BP measurement at your home (to prevent rise in BP and heart rate due to anxiousness/nervousness) or a continuous BP measurement over 24 hours (ambulatory BP monitoring) may be advised. In such cases, the BP cutoffs for hypertension may be even lower.
RISK FACTORS
The risk factors described increase the risk of developing hypertension and cardiovascular disease, and its complications. Increasing age and male gender are natural risk factors (an elderly male is more likely to have hypertension as compared to a young female adult). People of South Asian and African races also have a higher risk of developing high BP compared to white races.
Other risk factors include:
- Being overweight or obese (high BMI)
- Dyslipidemia (increased cholesterol +/- triglycerides in the blood)
- Psychosocial stress
- Taking too much salt (sodium) or too little potassium in your diet
- Sedentary lifestyle or inadequate physical activity
- Smoking
- Drinking too much alcohol
- Psychosocial stress or suppressed anger
- Diabetes
- Kidney disease
- Sleep apnea
- Long-term usage of medicines: painkillers (of the Ibuprofen group), some decongestant medicines for cold, some antidepressants or antipsychotics, oral contraceptives, corticosteroids, and certain anti-cancer drugs.
- Family history of high BP
- Women post-menopause, or who had hypertension or diabetes in any of their pregnancies.
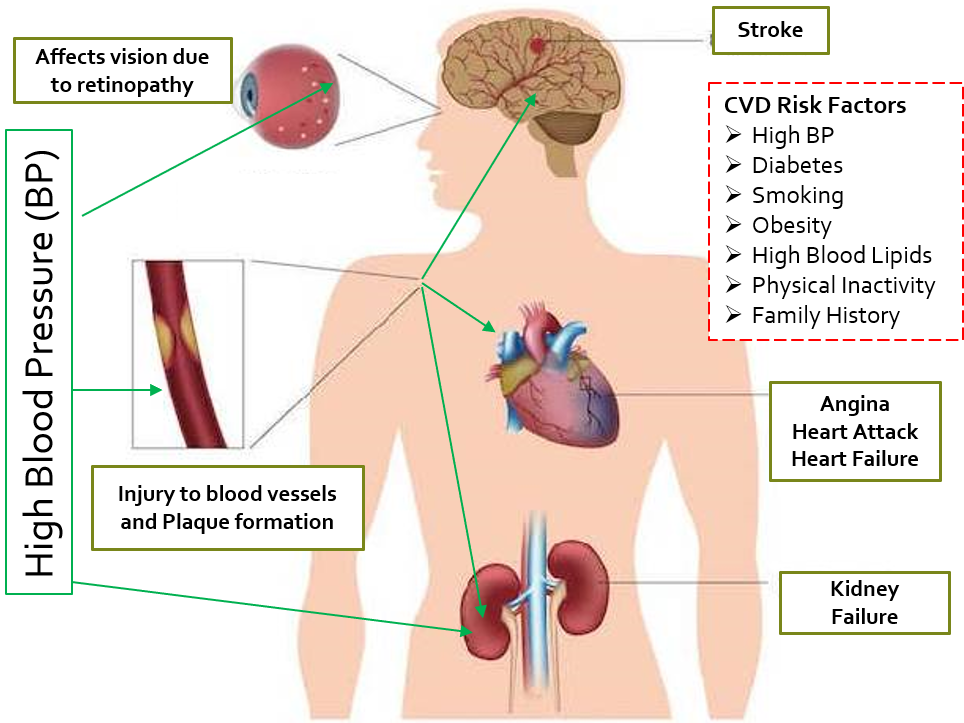
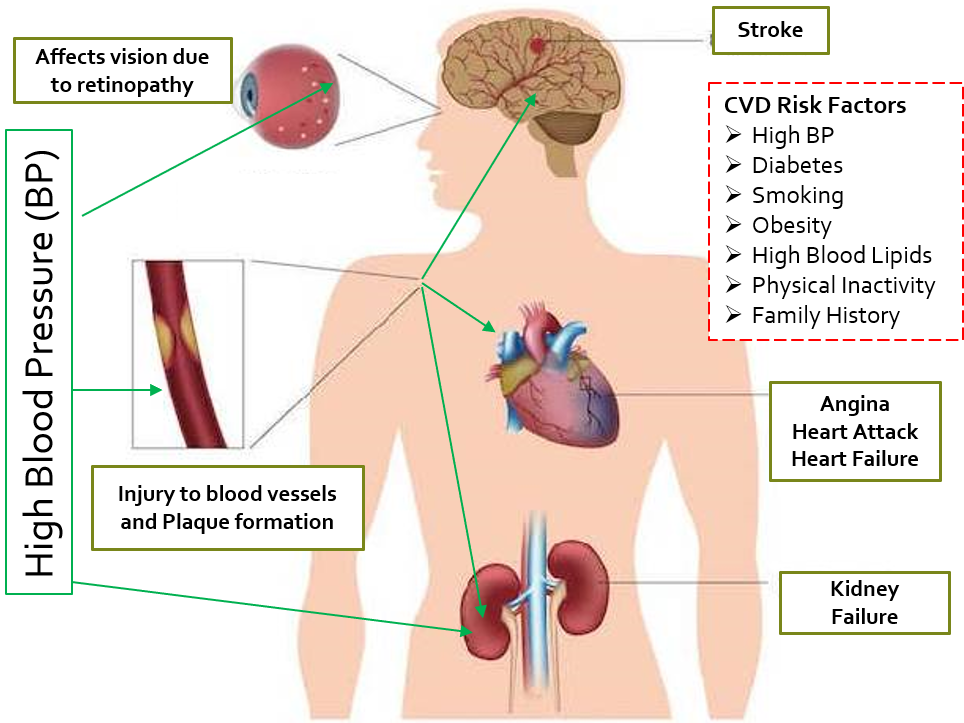
CONSEQUENCES AND COMPLICATIONS OF HYPERTENSION
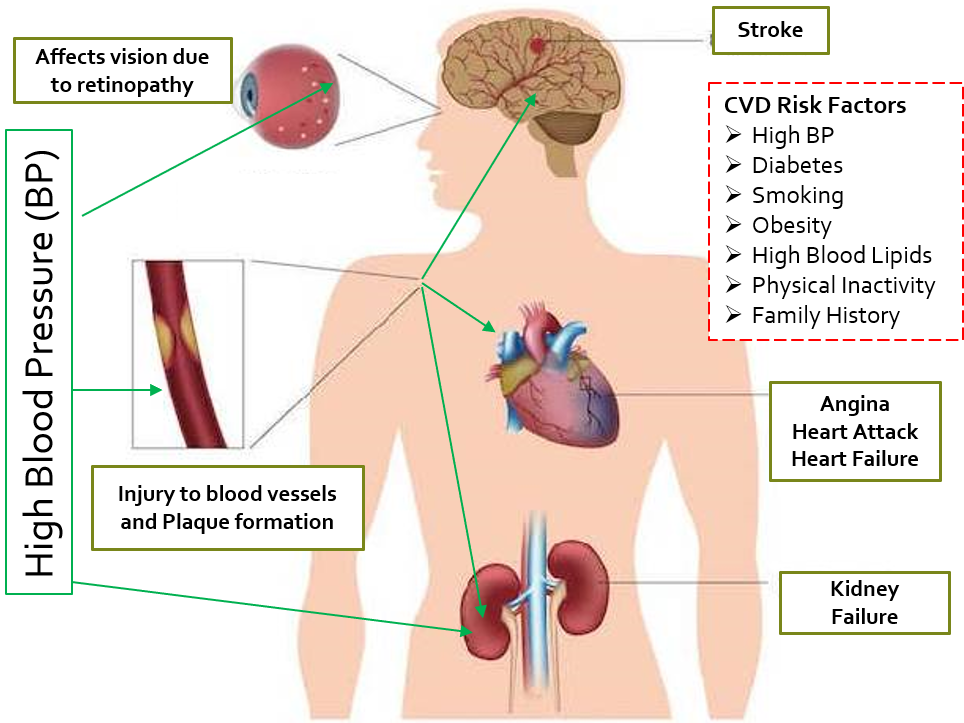
High blood pressure especially when not adequately or well controlled can lead to consequent complications.
Cardiovascular disease (CVD) refers to a group of conditions occurring due to blockage of blood vessels more specifically arteries and its resulting impact on the heart and other organs.
Blood flowing at higher pressure has more chances of causing micro-injuries to the artery wall. This gives rise to increased formation of ‘plaques’ and clots which cause narrowing or obstruction of arteries, leading to CVD. This can result in reduction (partial obstruction) or loss (complete obstruction) of blood supply to vital organs. The above risk factors mentioned for hypertension are also risk factors for developing CVD. High blood pressure increases the risk of CVD, and vice versa, while both CVD and hypertension may present simultaneously.
CVD can result in angina, heart attack (myocardial infarction), stroke, and peripheral arterial disease (PAD). Angina and myocardial infarction (MI) are caused due to partial, and complete blood flow obstruction to the heart respectively which causes heart pain due to oxygen deprivation to heart muscles. Since the heart has to pump blood against higher pressure and resistance, its contracting effort increases which can slowly lead to its reduced efficiency and inability to cope, causing heart failure.
Obstruction/reduction in blood flow to the brain leads to stroke, (also called cerebrovascular accident CVA). High BP can also affect blood flow to our limbs (peripheral arterial disease) which can cause intense pain on walking.
Hypertension can cause ongoing damage to the kidneys and eventual kidney failure.
Other complications like rupture or blockage of the fragile narrow vessels of the retina of the eye (hypertensive retinopathy) can affect vision. Hypertension can cause a reduction in blood flow and damage to many other organs like bones, reproductive organs, and others, hampering their functioning.
High/uncontrolled BP and CVD are risk factors for complications of COVID and other infections in those who get infected and have these comorbidities.
Complications of high BP are shown below.
HEALTH SOLUTIONS
Overall more the number of coexisting risk factors present in an individual, the greater the risk of developing complications of high BP. Sometimes a 10-year risk of CVD is calculated, and if it is > 10%, BP lowering medicines are started immediately along with lifestyle-diet measures.
Setting Target BP.
Target blood pressure with lifestyle measures, and medicines in patients ≥65 years and <65 years should be below 140/80 and 130/80 respectively. There is enough evidence showing BP levels between 130-139/80-89 mm Hg in the general population to be causing a substantial risk of cardiovascular disease (CVD), and premature death. Lower target blood pressure recommendations aim to create greater health consciousness of lifestyle and diet, help in early intervention to prevent complications, and maintain a higher level of community health.
So, <130/80 can be considered the new BP target globally from a cardiologist’s perspective. However, many general physicians today would still rather go with the <140/90 target BP, sometimes further relaxed to <150/90 in patients >65 years of age.
Planning Treatment
People in the stage of elevated BP are managed with lifestyle and diet modifications. These measures can reduce systolic BP by 4-10mmHg, usually in the range of around 5mmHg over a few months.
People in stage 1 hypertension who have coexisting cardiovascular risk factors (or a 10 year CVD risk >10%), will require a BP-lowering medicine in addition to lifestyle-diet measures, as compared to people without additional/coexisting risk factors who can be initially managed with lifestyle-diet measures alone.
All people in stage 2 hypertension should be managed with a combination of BP-lowering drugs, and lifestyle-diet modifications.
The target BP of all patients in stage 1 and 2 hypertension is <130/80. However, there may be variability among physicians and cardiologists in setting target BP in different patients.
Lifestyle and Diet measures for reducing BP and CVD risk
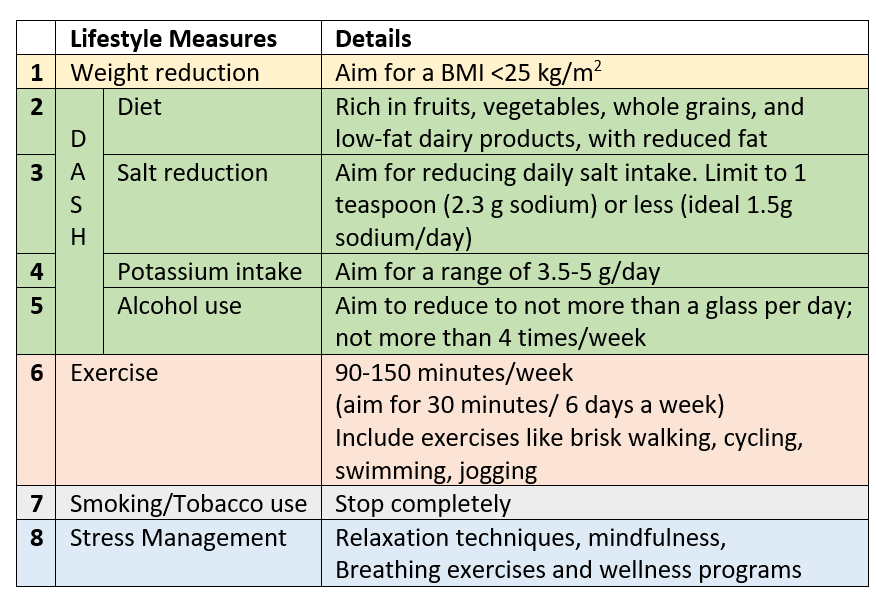
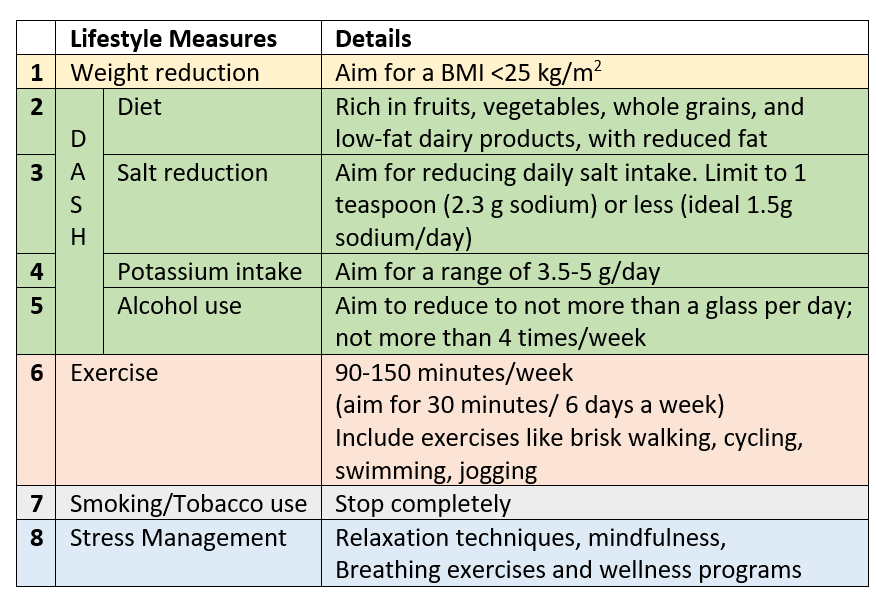
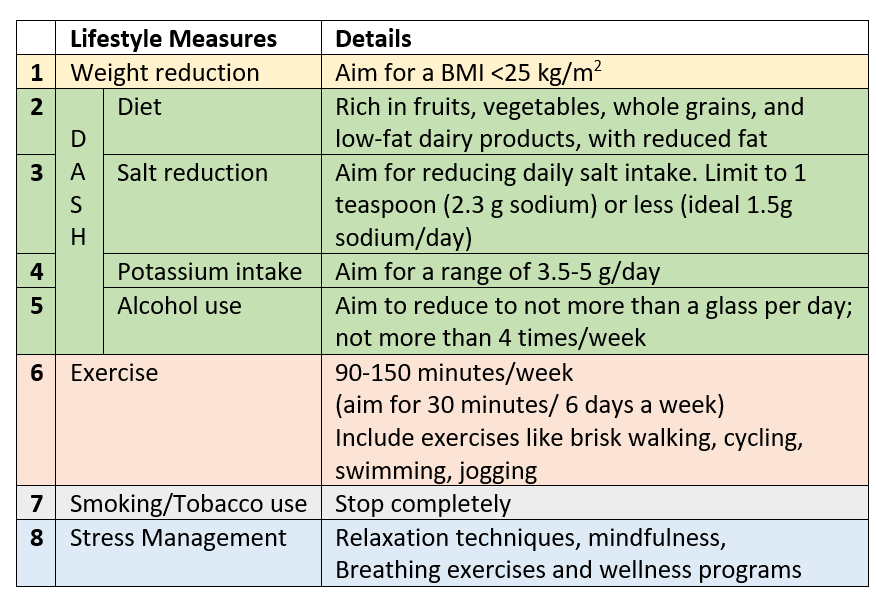
DASH– Dietary Approaches to Stop Hypertension is aimed at lowering BP, reducing the risk of cardiovascular sequelae and also helping in BMI and weight reduction.
Further lifestyle-diet measures for blood sugar and lipids (cholesterol and triglycerides) will also be advised if these 2 risk factors are coexisting with hypertension.
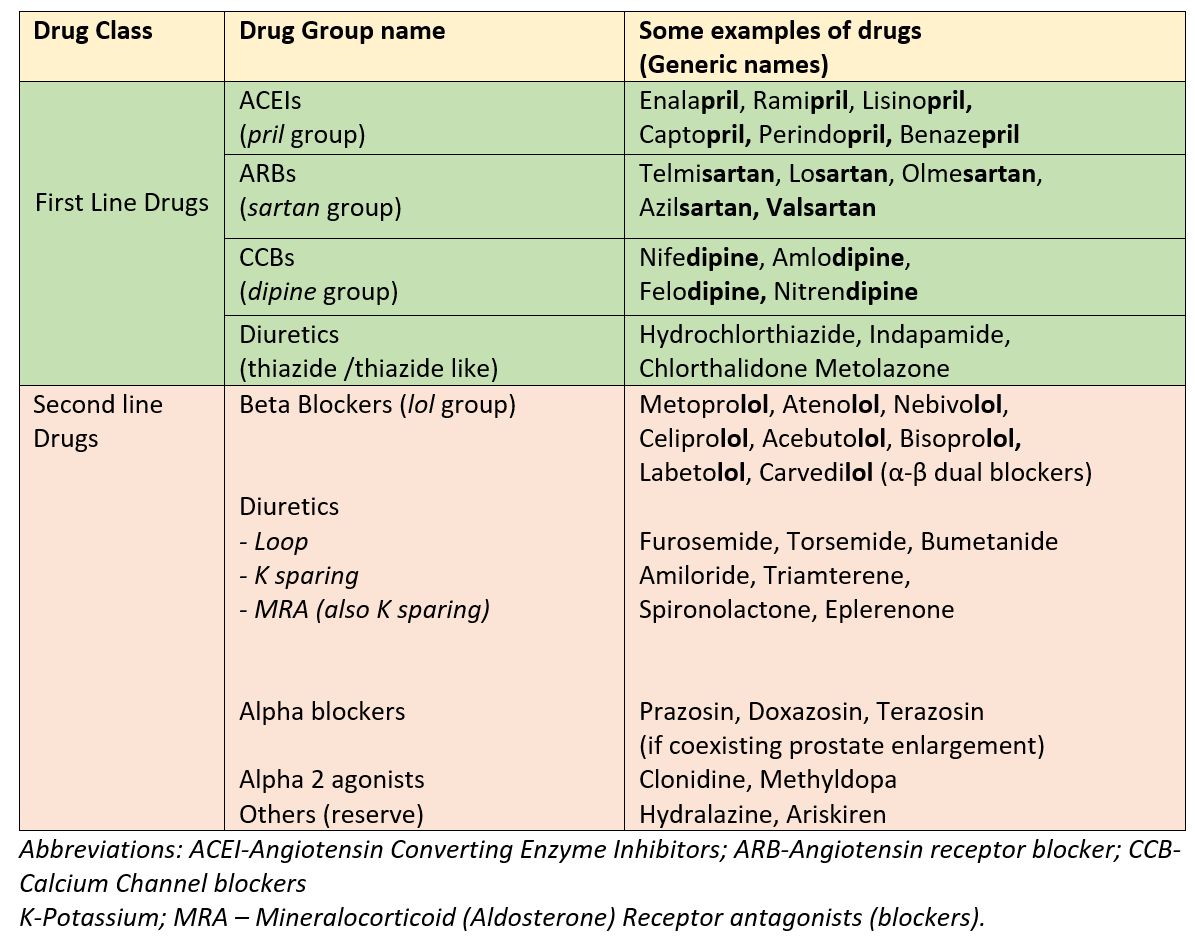
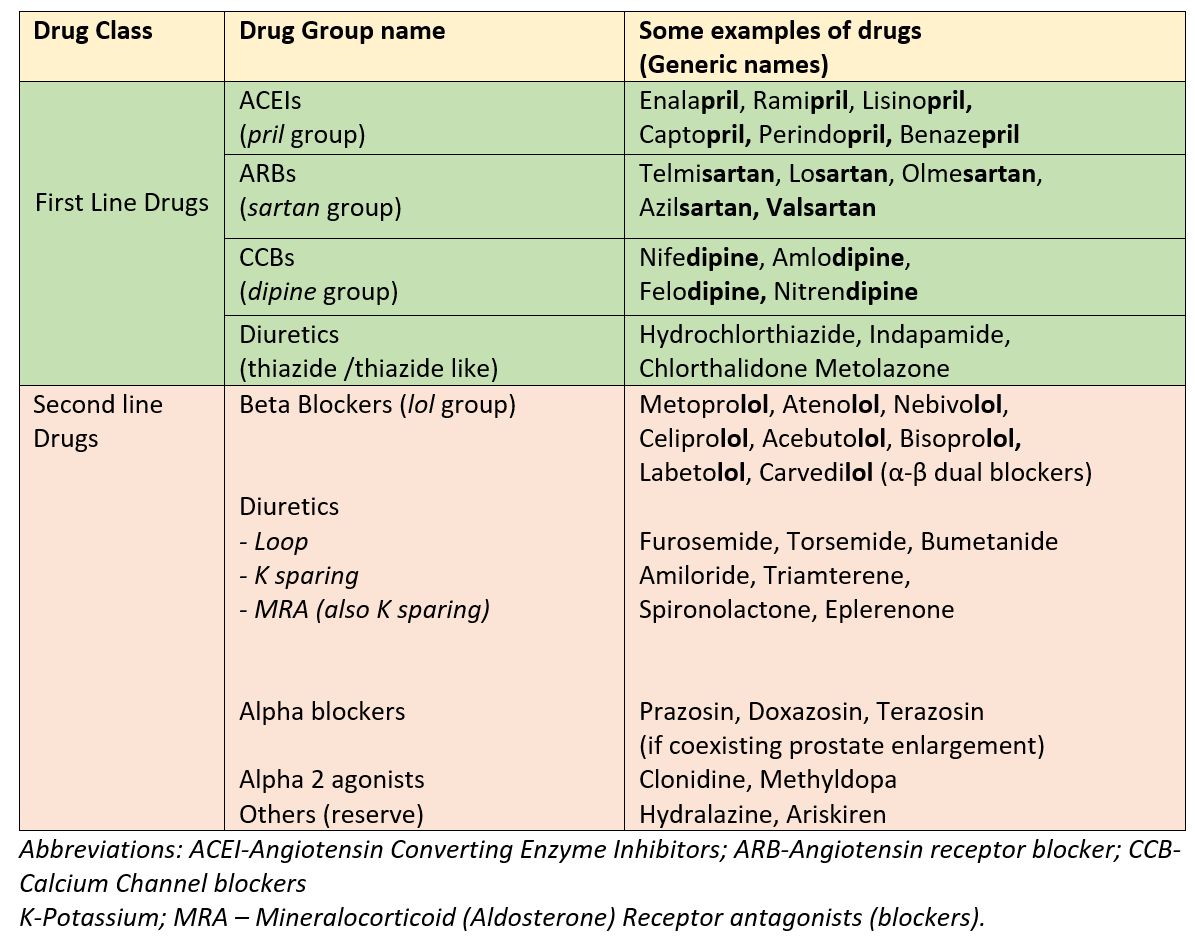
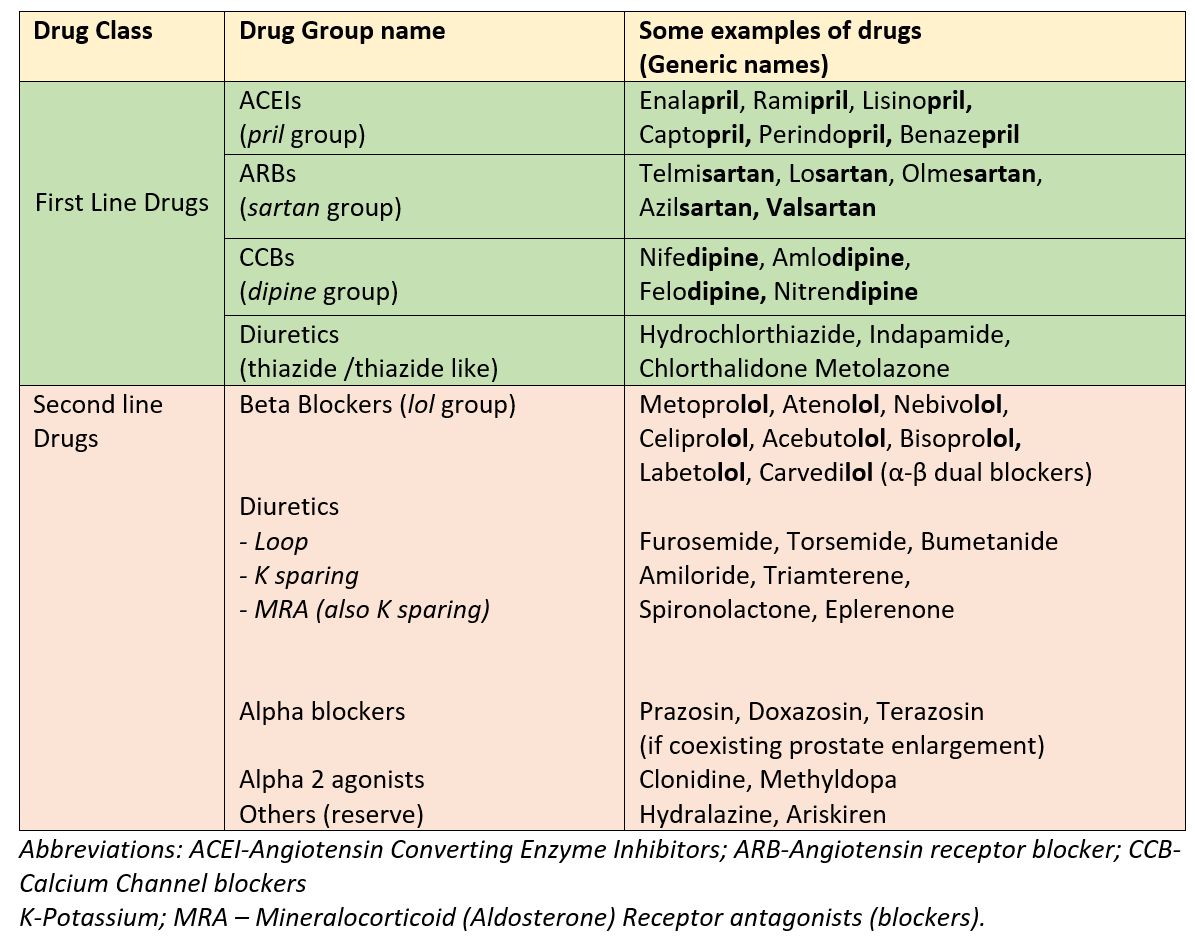
Overview of BP lowering Medicines
BP lowering medicines are given singly or in combinations (separately or combined in a single pill). Usually, one medicine is added for every 10mm systolic BP above target. Sometimes two medicines at lower doses may be preferred to one medicine at a higher dose, to improve response and reduce side effects.
There are 4 classes of BP-lowering medicines which are considered as first-line. One of these or a combination of these is used to bring and maintain the BP at target values. The second-line drugs are used when the combination of 3 first-line agents of different classes do not manage to control high BP or in certain special situations or patients with associated cardiac, kidney or other conditions.
Important points to remember
- All medicines should be taken only by prescription and recommendation of a qualified medical practitioner in the dose, schedule and time of day prescribed along with incorporating all the lifestyle and diet measures suggested.
- Separate medicines will also be needed for coexisting risk factors (like diabetes and high lipids) if present.
- Irregularity of taking these pills can lead to uncontrolled BP.
- There are certain situations where some classes of drugs may not be appropriate or suitable, while some may cause side effects in certain patients, so one should never start or change any drug without consulting a qualified physician.
- The blood pressure, and parameters for other risk factors when present, should be measured and monitored periodically under the guidance of the treating physician.
- Usually suggested follow up visit is at 3 months after starting on lifestyle-diet measures, and at 1 month after starting a BP-lowering medicine.
Some scientific terms
Essential (or Primary) hypertension is high blood pressure that doesn’t have a known cause.
Secondary Hypertension is high BP caused by another medical condition like diseases of the heart, kidney, arteries or hormones
Resistant Hypertension is the term used when the target blood pressure of below the cut-off cannot be achieved even with lifestyle measures and concurrent use of three BP lowering medicines (of the 1st line classes with one of the medicines being a thiazide group diuretic), after ensuring full compliance and regularity of treatment.
‘Uncontrolled Hypertension’ includes resistant hypertension as well as those patients not fully compliant or regular with medicines and/or incorporation of lifestyle measures.
The reserve or 2nd line medicines are then added in resistant hypertension to achieve target BP. Sometimes certain procedures (called renal denervation- by radiofrequency or ultrasound) may also be used to manage resistant cases.
Preeclampsia is high blood pressure during pregnancy. It can have serious consequences for the mother and fetus, therefore needs to be addressed timely. The first-line drugs below like ACEI, and ARBs cannot be given in pregnancy due to adverse effects on the fetus. Therefore preeclampsia is managed by drugs like labetalol, methyldopa, and nifedipine.
Also read-
Incorporating the DASH diet to reduce BP, BMI and Cardiovascular risk
For any query, additional information or to discuss any case, write to info@drvarsha.com and be assured of a response soon
References


