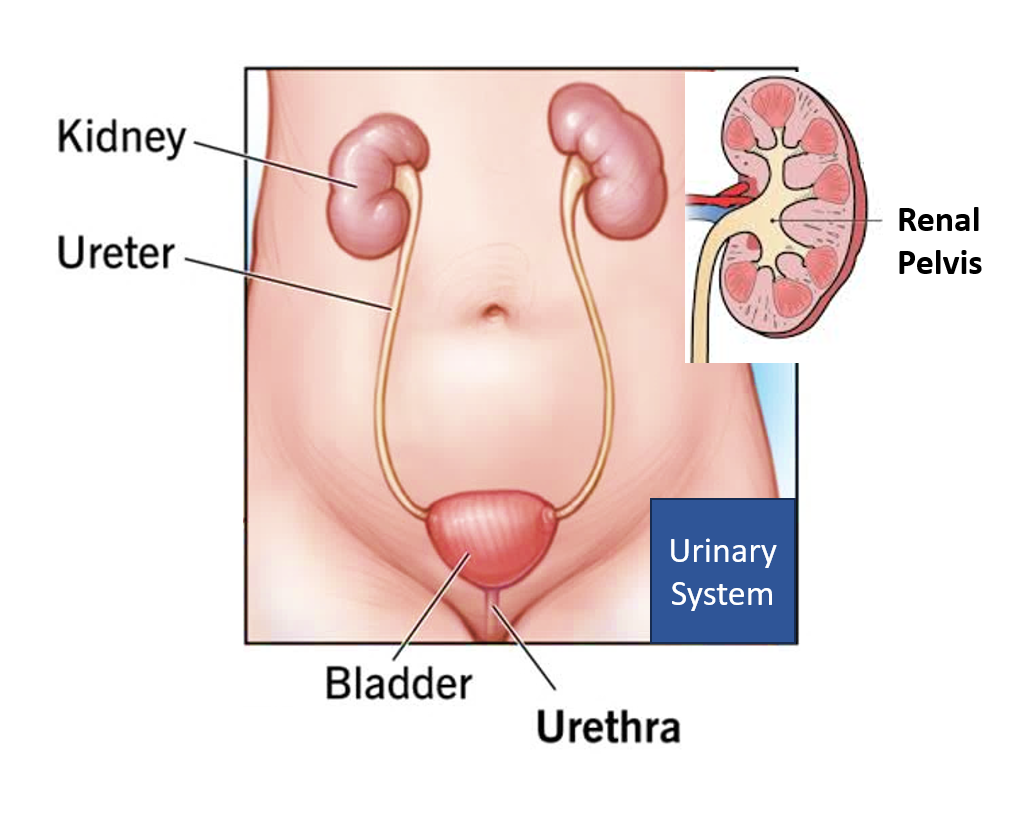
URINARY SYSTEM
The kidney is a bean-shaped organ on either side of the abdomen. They help in filtering and excreting wastes from our body out in the form of urine. There are tubes called ureters that arise from each kidney and enter a storage bag called the urinary bladder. From here the urine flows out through a tube called the urethra. The kidneys, ureters, bladder, and urethra constitute our urinary system.
URINE PRODUCTION
The kidney is made of millions of units called nephrons that are individually equipped to absorb and secrete substances into filtered blood, to form urine. Normally given an intake of 2L/day of water, 1-2L of urine should be produced in 24 hours. Human urine is composed primarily of water (95%), the rest being urea (2%), creatinine (0.1%), uric acid (0.03%), and electrolytes like sodium, potassium, chloride, sulfate, ammonium, phosphate, and other ions and sometimes trace amounts of proteins.
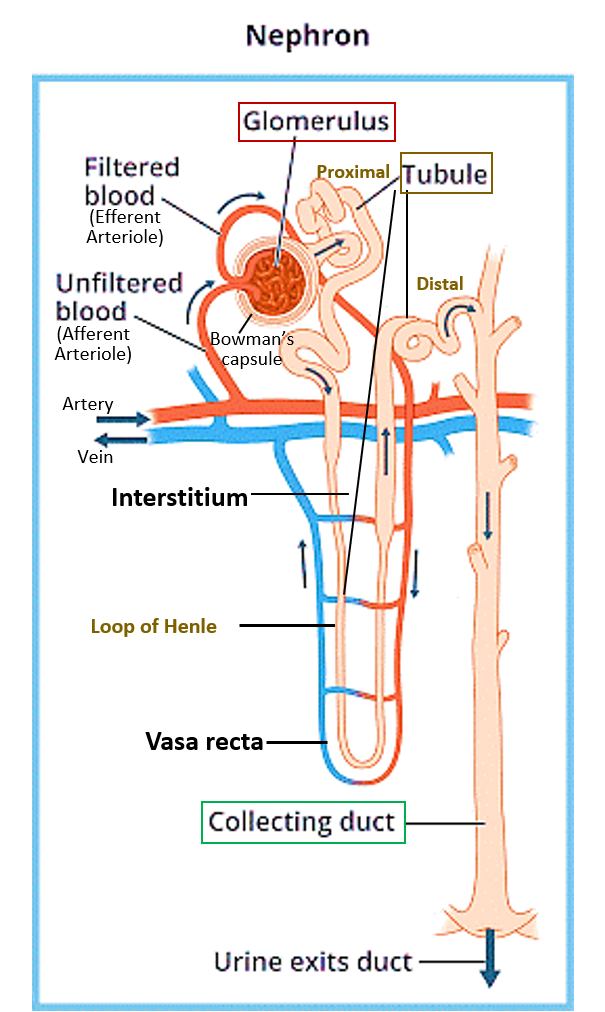
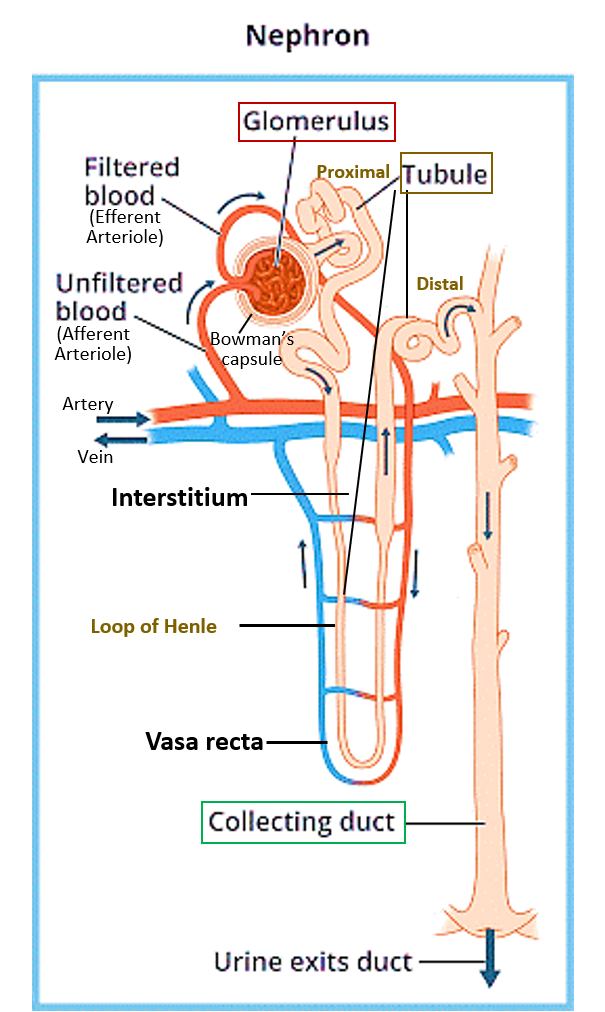
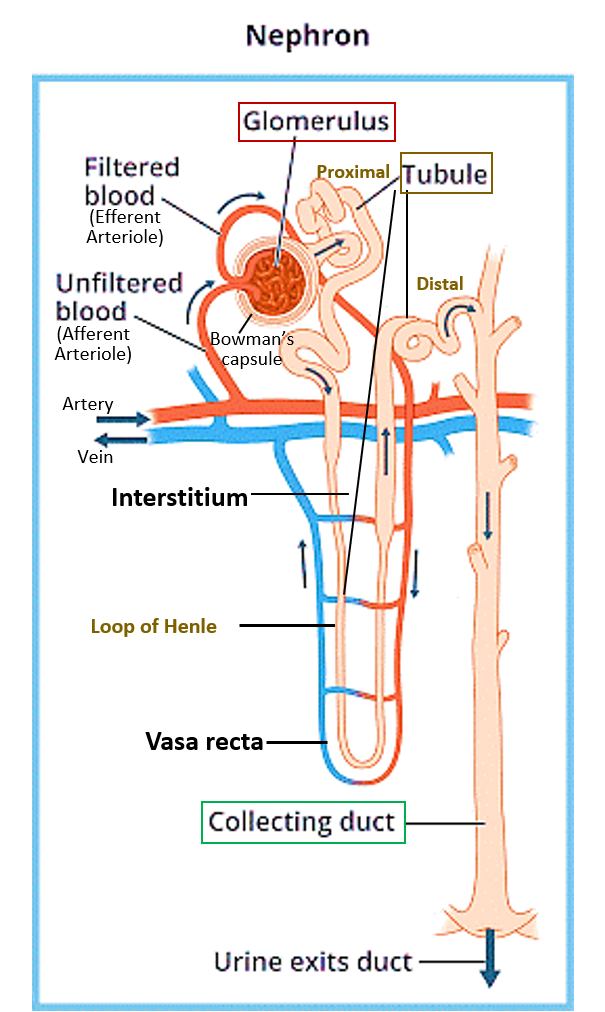
The blood to be filtered comes from a branch of the renal artery called the afferent arteriole from where it enters a network of capillaries called the glomerulus inside the cup of the nephron called the Bowman’s capsule. Blood with wastes filters out of the glomerulus into the renal tubule through the Bowman’s capsule of the nephron, and the filtered blood leaves through the efferent arteriole.
The filtered contents travel through the various parts of the renal tubule (proximal, loop of Henle, and distal) and substances are absorbed or secreted.
- The proximal tubule absorbs glucose, proteins/amino acids, vitamins, and lactic acid, and secretes creatinine, ammonium and hydrogen ions. The regulation of urea and uric acid in the urine also occurs here.
- The loop of Henle has a descending part that mainly absorbs water and secretes urea, while the ascending loop absorbs sodium, potassium and chloride ions.
- The distal tubule absorbs sodium, chloride, and bicarbonate ions along with water, and secretes potassium, hydrogen, and ammonium ions. So, this is the place where a sodium-potassium exchange takes place and is an important zone for water and electrolyte balance.
- The collecting duct mainly absorbs water and regulates urea according to the hydration status of the individual, producing the final concentration and volume of urine. Numerous collecting ducts merge into the renal pelvis, which then becomes the ureter.
- The tubules and collecting duct are supported structurally by a connective tissue in between called the interstitium.
HORMONAL REGULATION
The RAAS system (Renin-Angiotensin-Aldosterone System) regulates blood pressure, blood flow to the kidneys, the resistance of blood vessels, as well as fluid-electrolyte balance, all of which also affect kidney function and urine production. While the renin-angiotensin system causes vasoconstriction and increased blood pressure, with decreased blood flow to the kidneys, aldosterone increases the absorption of sodium and water at the distal tubule. There is another hormone called anti-diuretic hormone (ADH) that increases the absorption of water in the collecting ducts.
Cells lining the glomerulus convert prorenin in the blood into renin.
Renin converts angiotensinogen released by the liver to angiotensin I, which is converted by angiotensin-converting enzyme (ACE) in the cells lining the blood vessels to angiotensin II which is a potent vasoconstrictor that causes blood vessels to narrow, resulting in increased blood pressure. Aldosterone is produced by the adrenal gland just on top of the kidney, and ADH comes from the pituitary gland in the brain.
The kidney also produces two important substances, which are the hormone called erythropoietin which stimulates the bone marrow to produce red blood cells, and the enzyme that converts vitamin D to its active form calcitriol. Therefore, in kidney failure or chronic kidney disease, one has to give erythropoietin injections to prevent or manage anemia, and also supplement vitamin D directly in its active form calcitriol.
ABNORMAL KIDNEY FUNCTION
Kidneys may function abnormally due to problems or diseases of the kidney itself, or also due to other conditions like cardiovascular disease, heart failure, high blood pressure, diabetes and liver cirrhosis, as well as due to general infections or autoimmune diseases.
Inflammation or disease of the kidney cells (nephrons) is called nephritis. If this involves mainly the glomerulus, it is called Glomerulonephritis, while the involvement of the tubule and the interstitium is called Tubulointerstitial nephritis. The renal pelvis can be infected (Pyelonephritis) from urinary tract infection spreading upwards from the urethra, and urinary bladder through the ureters. There can also be stones formed in different parts of the urinary system.
Kidney failure can occur due to acute nephritis, which usually recovers once the inflammation is controlled or it can occur due to chronic kidney disease (CKD) that usually progresses to end-stage renal disease requiring dialysis or kidney transplant.
KIDNEY FUNCTION TESTS
These include urine, blood, and imaging tests that assess the functioning of the kidney.
URINE TESTS
Urine Volume
a. Polyuria: Volume more than 3000 ml / 24 hours as observed in Diabetes, some kidney diseases, excess water intake, intake of diuretics like caffeine, alcohol or drugs
b. Oliguria: Volume less than 400 ml / 24 hours as observed in fluid deprivation, excess fluid loss as in hemorrhage or shock, dehydration, progressive kidney diseases, obstruction in the urinary tract, heart and lungs diseases, and sometimes due to strenuous muscular exercise.
c. Anuria: Less than 150ml / 24hrs or complete absence of urine output, observed in kidney failure or shock (a critical condition brought on by sudden blood loss or drop in blood flow through the body).
Abnormal Substances in Urine
Urine tests look for the presence of abnormal substances in urine like sugar (glucose – glycosuria), proteins (proteinuria), fats (lipiduria), blood or red blood cells (hematuria), increased white blood cells or pus cells (pyuria) or casts and lining cells, that can indicate a functional deficit of the kidney.
Normally urine is colorless or light yellow. Gross loss of blood produces red-colored urine. Urine may be dark yellow or yellowish-brown during fever or increased bile pigments (bilirubin and urobilinogen) in urine. Infections like typhoid/cholera can give a greenish hue to urine. Some drugs like rifampicin can cause orange-red urine color. Fats in urine give a milky look. Proteins in urine give a foamy appearance. Ketones in urine may be seen in some people with diabetes that produce a fruity odor.
The amount of albumin and creatinine in urine are considered important indicators of kidney function. The UACR (Urinary albumin to creatinine ratio) should normally be less than 30mg/g.
Urine may also be evaluated for crystals of calcium oxalate, phosphate or uric acid.
Urinary Tract Infections (UTIs) can sometimes produce a foul odor in urine. The urine is usually tested for the presence of bacteria, which can then be cultured and evaluated for sensitivity to various antibiotics.
To test urinary volume, urine has to be collected over 24 hours. The excretion of creatinine and albumin over 24 hours is sometimes performed to assess kidney function.
BLOOD TESTS
These include a complete blood count (CBC) that helps look for low hemoglobin (anemia), or the presence of any infection or allergies. Creatinine and Blood urea nitrogen (BUN) are the two critical blood tests that when raised point towards abnormal kidney function. Blood proteins albumin and globulin with their ratio, and electrolytes including sodium, potassium, and chloride are also done to assess renal function.
For treating underlying conditions, blood sugar, lipid profile (triglycerides and cholesterol), and liver function tests (bilirubin and liver enzymes) would also be needed in some cases. Blood calcitriol (active form of vitamin D, and PTH -parathormone) tests may also be done to diagnose bone disease due to a renal cause.
From the creatinine values based on age, gender, weight and race, an estimated glomerular filtration rate (eGFR) can be calculated, which gives an idea of the filtering function of the glomerulus. The values are given as % of what is normal for that age, gender, weight, and race. Sometimes UACR and eGFR are used to grade the level of kidney dysfunction and risk of chronic kidney disease (CKD).
IMAGING TESTS
These include ultrasonography, which also aids in taking a biopsy sample, and CT/MRI.
The nuclear renal scan, also known as renal scintigraphy, is an imaging method that uses radiopharmaceuticals/ radiotracers to evaluate renal structure as well as function. The various injected radiotracers are extracted from the blood by the kidneys and emit radiation, particularly gamma radiation, that is detected by gamma cameras. In this test, images help visualize how blood flows in and out of the kidneys, and how urine flows through the kidneys, ureters, and bladder. Also, it can estimate the function of each kidney individually, and helps in diagnosing kidney disease, obstruction, swellings (tumors/cysts/abscess), and can also estimate blood pressure in renal arteries. It is especially useful to monitor kidney function after transplant.
Also read:
Tubulointerstitial nephritis – Causes, Diagnosis and Treatment
Chronic Kidney Disease (CKD) – 5 Key Points of Understanding