WHAT IS A SKIN ULCER?
Skin ulcers are common and have many causes and mechanisms. The term ‘ulcer’ means a breakdown in the continuity of any protective lining tissue in the body, in this case, the skin. The term ‘wound’ also means the same, however, the difference between a wound and an ulcer is that a wound is caused by a single event of injury or trauma therefore the cause is immediate and external. An ulcer is caused due to external or internal factors acting over a period of time. The external factors could be pressure, repeated friction or trauma, skin irritation, and infections, while internal factors include poor blood circulation or affected nerve function. Sometimes these two terms are used interchangeably in common parlance.
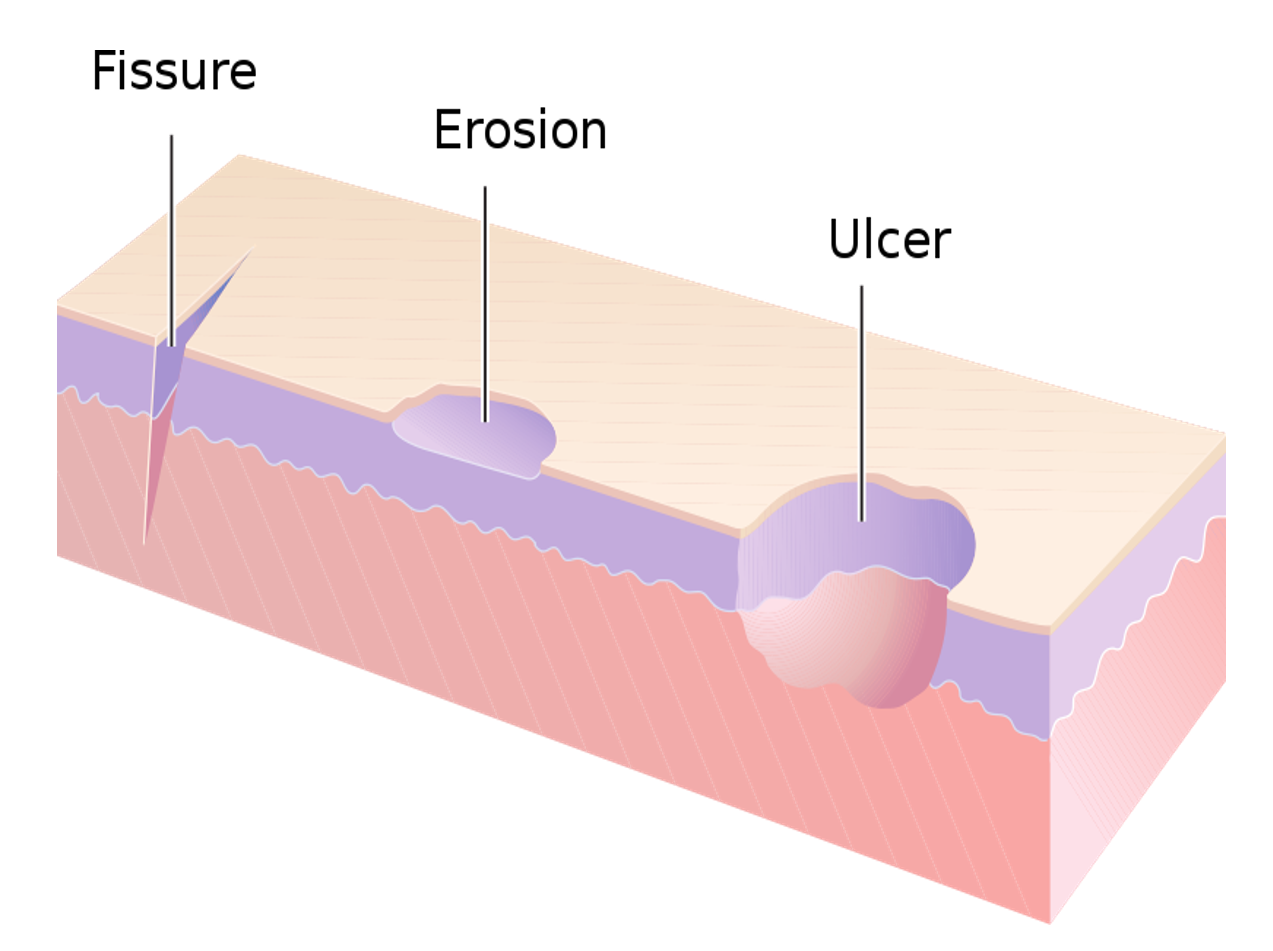
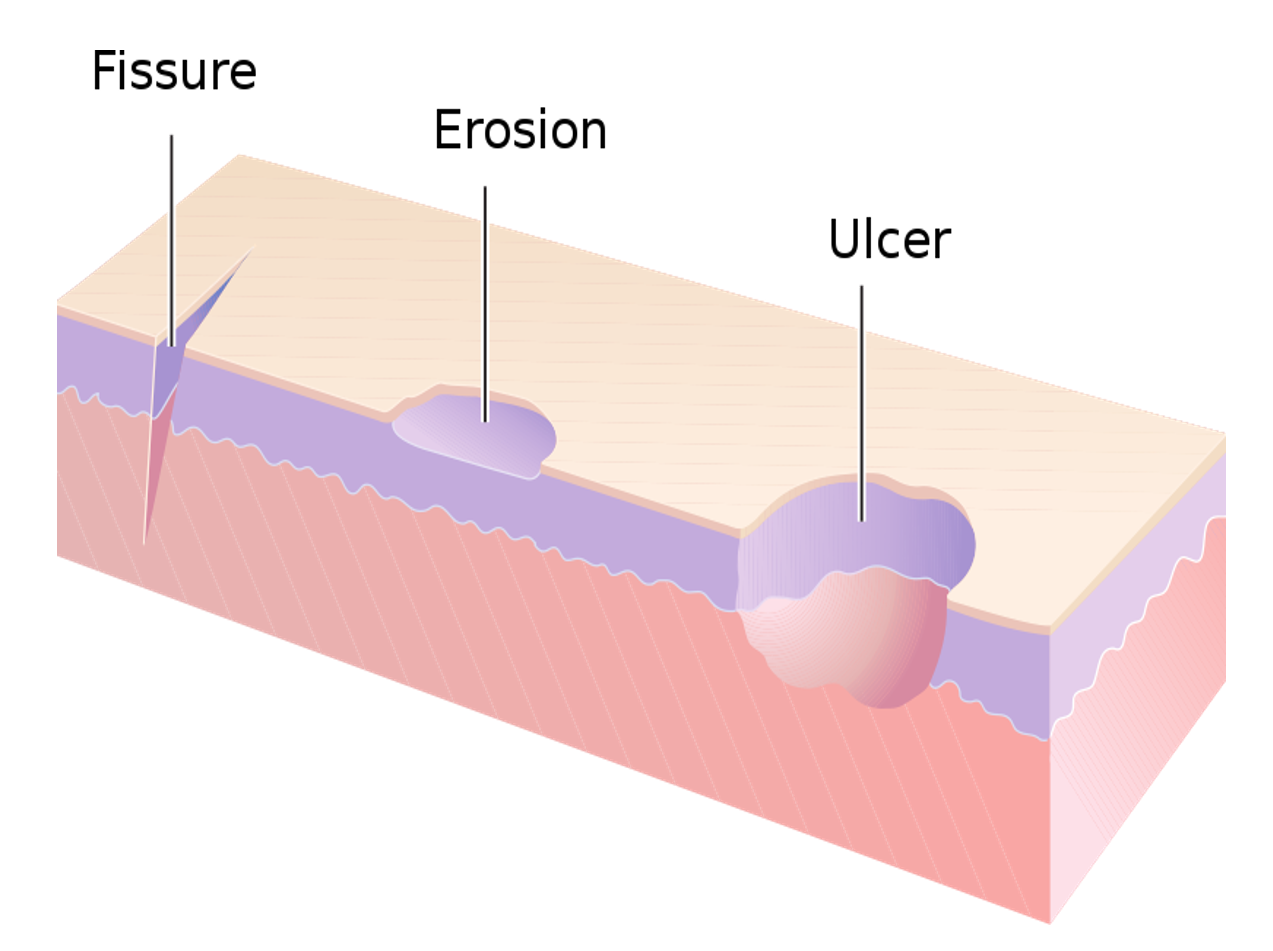
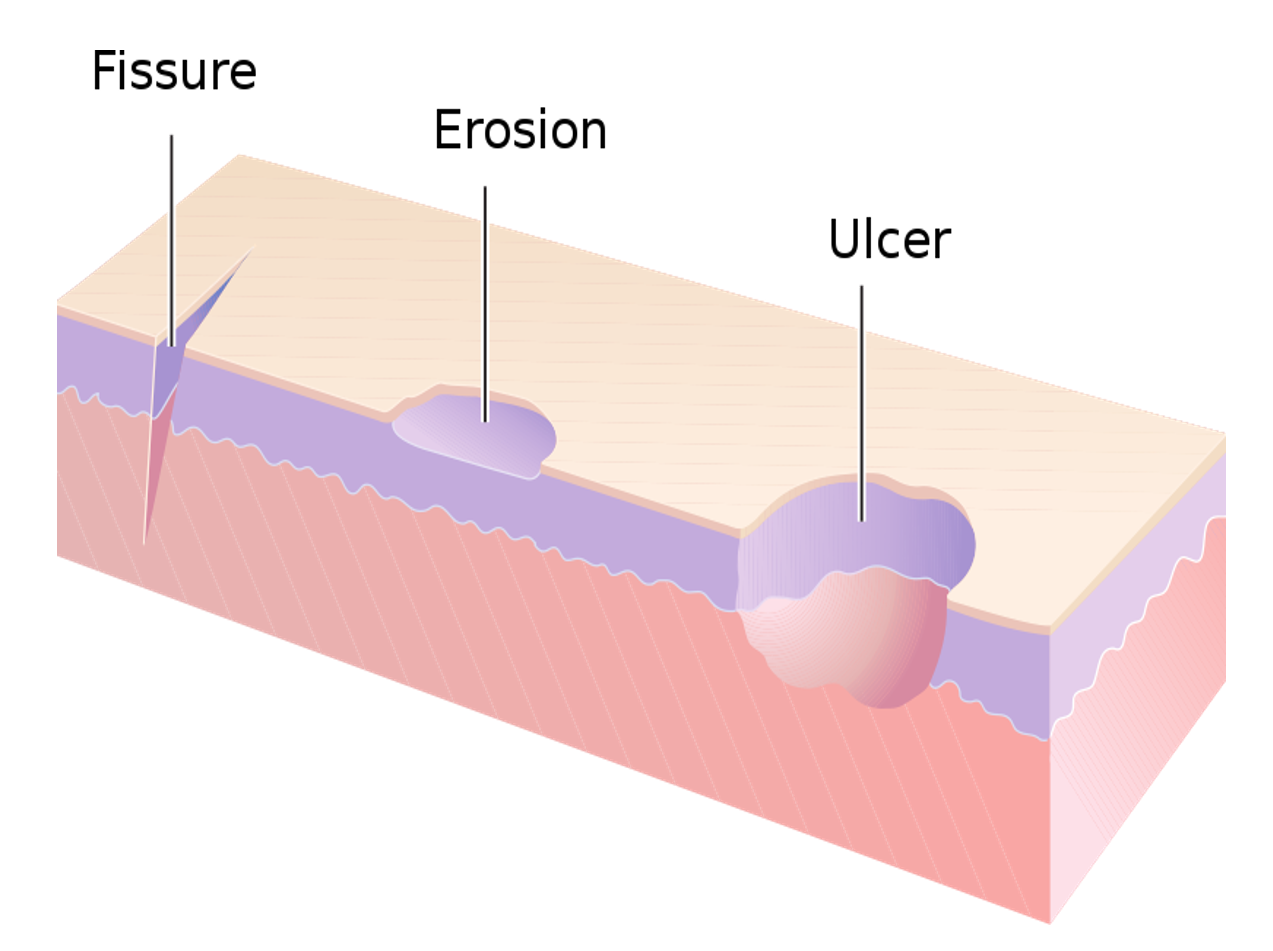
An ‘erosion’ is a term that refers to the loss of only the superficial layers of the skin (epidermis), and healing usually occurs without scarring. An ulcer refers to loss or damage of both superficial and deeper skin layers (epidermis and dermis) and can sometimes extend to underlying fat and muscle. When an ulcer is very deep but narrow, it is called a ‘fissure’ as seen to occur in the anal area due to trauma-induced by hard stools. A ‘sore’ is an umbrella term for any damaged, inflamed, or injured area which causes discomfort or pain.
WHAT ARE THE CAUSES AND TYPES OF SKIN ULCERS?
As mentioned, skin ulcers are caused due to internal or external causes, or a combination of both, over a period of time, which can range from a few days to weeks or even months.
POOR CIRCULATION
This is a common reason for ulcers in the legs and feet, as they are the dependent parts of the body. Such ulcers can either be because of deficient blood supply by the arteries (arterial ulcer) or poor functioning of veins (venous ulcer).
Arterial ulcers are also called ischemic ulcers as they occur due to a deficient supply of blood and oxygen, which leads to poor nutrition, and death of the tissues. Causes of arterial insufficiency can be narrowing, compression, or damage of the artery. Narrowing of the artery is seen due to ‘plaques’ causing atherosclerosis. Risk factors include smoking, diabetes, hypertension (high BP), kidney disease, high cholesterol, obesity, and increasing age. The narrowing can also occur due to inflammation of the artery wall (vasculitis). Sometimes an artery can be compressed by bone or joint deformities, or damaged during an injury or surgery.
Venous ulcers are caused due to deficiency of the blood flow in the veins that leads to stagnation and pooling of blood as seen in chronic venous insufficiency. This causes blood to leak out from the vessels, leading to swelling, inflammation, and break down of the skin. Interruption of the normal venous blood flow can occur due to deficient functioning of vein valves (as in varicose veins), or absence of muscle action (as in prolonged immobilization), both of which are important factors pushing the blood in the veins against gravity. Venous blood flow can also be impaired due to obstruction of the vein by blood clots (venous thrombosis), inflammation of the vein (phlebitis), and in pregnancy (due to pressure from an enlarged uterus).
PRESSURE
Continuous pressure on a particular area of the body, can also decrease the local blood circulation and make the skin break down to form pressure ulcers. Here the cause is not primarily in the blood vessels as seen with arterial and venous ulcers, but due to continuous pressure on the skin.
This is commonly seen in people who are in a lying position (decubitus) for prolonged periods, due to which there is increased pressure of the bodyweight on areas like buttocks, hips, and back. Ulcers which develop as a consequence are called bed sores or decubitus ulcers. Such ulcers can also be found on the back of the head, shoulder, elbow, ankle, or heel.
Tight footwear can cause increased pressure on ankles and heels, leading to pressure ulcers in this area. Sometimes tight bandages especially for fractures can also cause such pressure ulcers.
SKIN IRRITATION AND FRICTION
Repeated and prolonged trauma to the skin can occur due to skin irritation, allergy, or inflammation causing extensive itching like seen in eczema and other skin inflammation. Repeated friction on the skin surface can also cause an ulcer to form over a period of time, as seen with rough clothing items or bandages, certain metallic items worn or used as instruments, and inappropriate footwear (causing shoe bites) all of which cause constant rubbing on the skin.
Infections in the skin like boils can cause an ulcer to form especially after draining the pus. Prolonged exposure to water can also sometimes cause the skin to break down due to waterlogging (maceration).
IMPAIRED NERVE FUNCTION
When nerve function is affected as in diseases of the nerves called neuropathies, there is a reduction in the sensations in that area. Therefore, repeated trauma is ignored and not perceived leading to the formation of skin ulcers (neuropathic ulcers). Such ulcers are seen commonly on the foot which are sites of constant and repeated trauma. Poor nerve function also decreases tissue nutrition and healing, adding to the increased risk of developing ulcers. Therefore, such ulcers are often also called neurotrophic ulcers.
COMBINATION OF FACTORS
Sometimes a combination of factors may be responsible for ulcer formation. In diabetes, there is often damage to the inner lining of blood vessels (endothelium), and atherosclerosis leading to impaired circulation. There is also long-term damage to the nerves (diabetic neuropathy). Therefore, ulcers especially in the foot are seen in many people with diabetes (DFU- Diabetic Foot Ulcers). The increased sugar level also increases the rate of infection in these ulcers. Diabetic foot ulcers, therefore, heal very slowly and can often be recurrent.
In patients wearing rough and tight bandages, both reduction in blood circulation due to pressure, and local skin irritation and friction can cause ulcers to form. In the case of burns (heat/radiation/electric), multiple factors lead to ulcer formation like damage to the skin tissue, blood supply and nerves, and/or presence of infection.
Very rarely skin cancers or auto-immune diseases may be causes of ulcers.



SIGNS AND SYMPTOMS
Ulcers usually look red, with raised inflamed margins. There may be leakage of fluid (exudate or discharge), which can be clear and watery (serous), stained with blood (serosanguineous), or filled with pus when infected (purulent). If there is dead tissue lying in the ulcer (eschar), it may show a blackish-brown color. Pus and dead tissue can also cause a bad smell. The surrounding skin usually shows swelling and discoloration. The symptoms are typically pain, and skin irritation.
Arterial ulcers and neuropathic ulcers are usually deep and well punched out. In arterial ulcers, the skin feels cool, and pulsation of the arteries in the vicinity may be absent. Neuropathic ulcers can be painless due to damage of the nerves and the absence of sensations. Venous and pressure ulcers are shallow with swollen irregular margins.
Diagnosis is usually made visually. Blood or imaging tests may be advised in some cases, to investigate the underlying cause.
TREATMENT
There are two components to treatment – firstly to treat and heal the ulcer itself, and secondly to address the causative factor/s. Some ulcers may take very long to heal especially when circulation or nerve function is impaired, and associated comorbidities like diabetes, malnutrition, and infections are present. Ulcers that take more than 12 weeks to heal are referred to as ‘chronic’ while faster healing ulcers are called ‘acute’.
ULCER CARE
Small non-infected skin ulcers can be treated at home, while large or deep ulcers require a doctor’s care and monitoring. If there is visible dead tissue it should be removed (debrided) by a medical practitioner. An ulcer with copious discharge should be left open till the discharge minimizes.
The ulcer is usually treated and healed by ‘dressing’. The ulcer should be cleaned very gently with a gauze piece wetted with clean water or saline, to remove any loose or dead material. An antiseptic ointment/cream/paste or spray can be applied. Thereafter a gauze piece of adequate size is placed on the ulcer followed by wrapping with a bandage. Dressings should be changed daily or once in 2-3 days depending on the soiling, and stage of healing. Loose cotton should not be used either for cleaning or dressing.
Natural antiseptics made from turmeric/curcumin and herbs like aloe vera can be used if there is no obvious infection. Povidone Iodine is the most common antiseptic prescribed. Now better versions called Cadexomer iodine are available which contain iodine in beads. They help release iodine slowly and over a longer period of time, which reduces the toxic effect of iodine on the tissues, and also absorbs exudates, thereby improving healing rates. Nano-silver preparations available as gels/ointments or as dressing gauze can also be used. Antibiotic ointments like bacitracin-polymyxin-neomycin, mupirocin, framycetin, or fusidic acid should be used sparingly and briefly, as prolonged and indiscriminate use causes resistance as well as damage to skin cells, which can slow down healing.
The bandage applied should not be too tight, and not irritate the skin. A simple way to test that is to see that the affected part is movable without any restriction, and also the person is comfortable and not reporting a feeling of pressure or irritation. Foam and Alginate dressings are also available which have better comfort, absorption, and healing.
Hydrocolloid gels (or hydrogels) contain acrylic polymers/ carbomers and can be applied on the ulcers. These form a protective coating and improve healing, so additional dressing is not needed. Some of these gels are also combined with silver. These can be used after the initial few days of gauze/bandage dressing once the ulcer is healing satisfactorily. Hydrogels are also available as adhesive sheets.
Ulcers that do not heal even after prolonged periods will need skin grafting.
Additionally, sometimes vitamin-mineral supplements are also given orally to improve nutrition and aid healing. Oral antibiotics are given if infection is significant. Anti-inflammatory and pain-killer medicines (NSAID class) are recommended to reduce the pain and swelling.



ADDRESSING THE CAUSE
Comorbidities should be effectively managed like effective control of blood pressure, blood sugar, and lipids (cholesterol and triglycerides). A nutritious healthy diet with adequate physical activity and exercise for maintaining optimum weight/BMI, and avoidance of smoking is recommended.
Avoid tight or uncomfortable footwear (shoes/socks) and sports gears. People who have diabetes should examine their feet regularly. Special orthotic footwear and soles are also available to minimize foot trauma and pressure while maximizing wearing comfort.
Leg elevation and compression stockings help to improve circulation. Changing position every 2 hours if lying or every 15-30 minutes if in a wheelchair, and using alternate pressure/higher density foam mattresses or air/water beds can help to prevent pressure ulcers in immobilized people. Some medicines to improve blood flow like pentoxifylline and cilostazol have shown to be of supportive value in arterial ulcers. Vascular surgery may be needed for repairing venous valves, releasing compression on blood vessels, or for bypass (revascularization) of obstructed vessels.
COMPLICATIONS
Rarely an ulcer may cause complications like the spread of infection to deeper layers of the skin (cellulitis), to underlying bone and joints, or to the blood circulation throughout the body (septicemia). Such infections usually require the use of injectable antibiotics and hospital care. Rarely, infection and death of a large amount of tissue of the affected body part (called gangrene) may even require amputation.
Also read –
Diabetes: Understanding health risks and effective diet-lifestyle measures
For any query, additional information or to discuss any case, write to info@drvarsha.com, and be assured of a response soon.
References


