What is Cardiomyopathy? How is it different from Myocarditis?
As the word suggests, cardiomyopathy is a disease (pathy) of the muscles (myo) of the heart (cardio). When heart muscles get damaged, the force of contraction decreases, and so does the amount of blood pumped out into the arteries. This eventually leads to heart failure.
Cardiomyopathy is closely related to myocarditis which refers to the inflammation of the heart muscles. Many of the causes, risk factors, and symptoms of cardiomyopathy and myocarditis are common. Myocarditis often resolves spontaneously with supportive treatment, but in severe and persistent cases it can lead to cardiomyopathy which is the damage and reduced function of heart muscles. Therefore, in such cases, myocarditis is synonymous with inflammatory cardiomyopathy.
What are the Causes?
Often the cause maybe unknown or not determined. Cardiomyopathy may also be inherited (hereditary) or run in families. Some known causes and risk factors that are associated with increased risk of muscle damage that can be sudden or over a period of time are:
- Heart attack (myocardial infarction – MI) and coronary artery disease
- Hypertension (high BP)
- Tachyarrhythmias (fast heart rhythm disorders)
- Infection and inflammation of the heart muscles (myocarditis)
- Diabetes
- Obesity
- Thyroid disease
- Cardiac valve defects
- Vitamin B1 deficiency
- Alcohol abuse
- Deposition of abnormal substances in the heart muscles – sarcoidosis (abnormal lumps of inflammatory cells called granulomas), amyloidosis (abnormal proteins), hemochromatosis (iron overload).
- Autoimmune (connective tissue disorders) like lupus and scleroderma
- Drugs – Chemotherapy (anthracyclines) and radiation for cancer, anabolic steroids, anti-HIV drugs, chloroquine, antipsychotic drugs (phenothiazine group, clozapine), cocaine, and amphetamines
- Family history of cardiomyopathy or heart failure
What are the Symptoms of Cardiomyopathy?
The initial period of the disease is usually without symptoms. When heart failure starts to set in then symptoms appear like:
- Fatigue
- Dizziness
- Palpitation
- Breathlessness (initially on physical exertion and later even when at rest)
- Swelling in legs-ankle-feet and abdomen
- Cough and chest discomfort or a feeling of pressure when lying down
Are there different types of Cardiomyopathy?
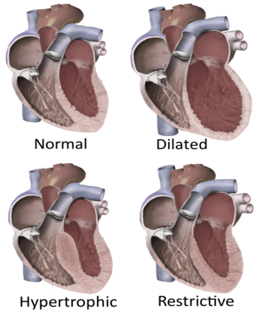
Cardiomyopathy usually affects the left ventricle of the heart most significantly. The main types are:
Dilated cardiomyopathy – The weakened heart muscles are unable to pump blood effectively, which causes the ventricle to enlarge (dilate). This is seen after a heart attack damaging large parts of the heart muscle, or long-standing coronary artery disease, and with alcohol/drug abuse, and myocarditis. It more often affects middle-aged men but it is sometimes seen as a complication of pregnancy. This kind of cardiomyopathy may rarely be inherited also.
Hypertrophic cardiomyopathy – The heart muscles become abnormally thick, making it difficult to contract and pump blood, and also narrows the ventricle preventing adequate filling. It is mostly caused due to genetic mutations and is often inherited. It is seen more commonly and more severely in children. This should be differentiated from simple ventricular hypertrophy which is the thickening of the walls of a ventricle of the heart, often seen in the elderly, and in those with high BP, coronary artery disease, or after a heart attack. Left ventricular hypertrophy is more common than right but concurrent hypertrophy of both ventricles can also occur.
Restrictive cardiomyopathy – The heart muscle becomes stiff and inflexible. Therefore, the muscles are unable to relax and create room for adequate blood to fill the ventricles. This reduces the amount of blood available for pumping. It is seen in conditions where abnormal substances are deposited in the heart muscle like iron, amyloid, inflammatory cells, tumors, etc. It is also seen due to scarring (fibrosis) after chemotherapy and radiotherapy, and in some fibrotic diseases like scleroderma. Restrictive cardiomyopathy is more common in the elderly.
How is Cardiomyopathy managed?
Cardiomyopathy is diagnosed based on symptom history and examination, and tests like chest X-ray, ECG, echocardiography, and cardiac MRI/CT. Blood tests include complete blood counts (CBC), kidney, liver, and thyroid function tests, iron levels, and protein markers of heart muscle damage like B-type natriuretic peptide (BNP). Cardiac catheterization (inserting a tiny tube into the heart through an arm/leg vein) can help assess the pressure in the ventricles and pumping effectiveness. A dye inserted during the procedure (coronary angiogram) can reveal blockages. A heart muscle biopsy can also be performed during this procedure.
Home remedies include salt and fluid restriction, minimizing alcohol intake, stopping smoking, and restricting strenuous physical activity.
Anti-inflammatory medicines like the NSAID group or a course of corticosteroids may be given to treat inflammatory cardiomyopathy or myocarditis. Drugs to manage heart failure are the cornerstone of treatment that include diuretics to reduce swelling may be needed, as well as medicines for blood pressure and decreasing heart load and rate like ACEI/ARBs or beta-blockers, and drugs to manage arrhythmia. Blood thinners (anticoagulants) may be added in case of assessed thrombosis risk.
Interventions (procedures and surgery) include those to remove portions of thickened heart muscle (septal ablation through catheter, or surgical septal myectomy), and to improve pumping action and blood flow (Ventricular assist device – VAD). Extracorporeal membrane oxygenation (ECMO) acts like an external lung through which blood is passed to remove carbon dioxide and add oxygen to the blood. For heart rhythm disturbances due to cardiomyopathy, radiofrequency ablation, pacemaker, or Implantable cardioverter-defibrillator (ICD) are used. Heart transplant is the treatment recommended, while the medicines and interventions are supportive and buy time till the appropriate donor is available.
Also read:
Inflammation of Heart Layers (Carditis) – Pericarditis, Myocarditis, Endocarditis
For any query, additional information or to discuss any case, write to info@drvarsha.com and be assured of a response soon.
Reference

