Asthma and Bronchitis are two of the most common conditions affecting our lower airway (lower respiratory tract).
Human Airway – Upper and Lower
Our respiratory tract (airway) consists of
- Upper airway – nose (nostrils), throat (pharynx) and voice box (larynx)
- Lower airway – windpipe (trachea), bronchi and bronchioles, finally leading into the lungs where oxygen is taken up into the blood and carbon-dioxide gas is given out.
Airway inflammation occurs due to viral or bacterial infections, allergies, or exposure to environmental irritants.
Upper airway inflammation includes common cold, flu, sore throat, and cough. These are usually acute in nature (sudden onset, lasting less than 1-2 weeks). The recovery is spontaneous with symptomatic treatment (for viral infections, and environmental irritants) or with a course of appropriate antibiotics (for bacterial infections).
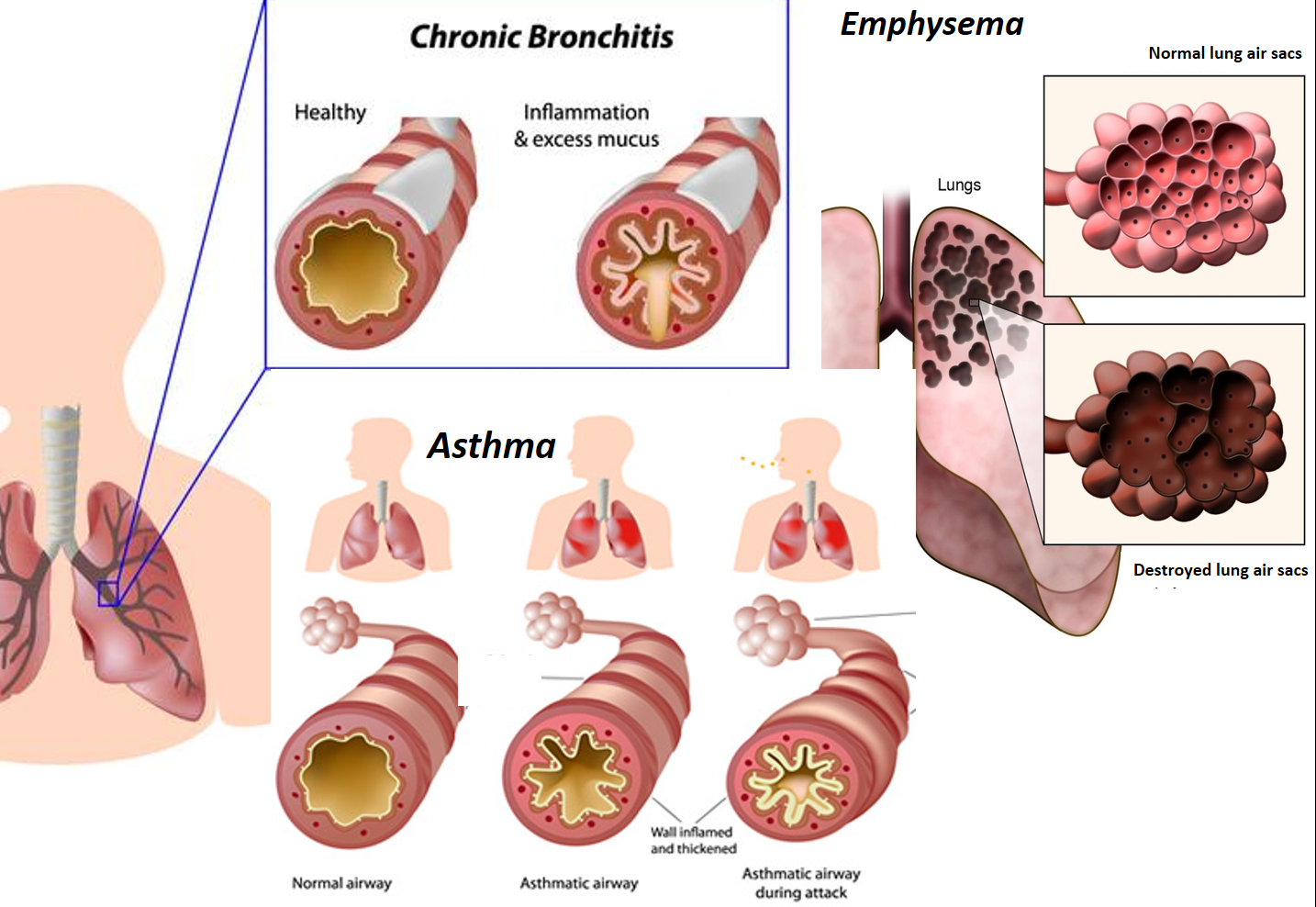
Lower airway inflammation may also be acute as seen in infections of the bronchi (acute bronchitis) and lungs (pneumonia), or chronic (developing over a period of time and lasting for weeks or months to years) as seen in asthma and chronic obstructive pulmonary disease (COPD – includes chronic bronchitis.and emphysema)
ASTHMA AND COPD (CHRONIC BRONCHITIS)
How and why they occur
Asthma and chronic bronchitis represent two important chronic inflammatory conditions of the lower airway (bronchi). They have periods of flare-ups (called exacerbations– when symptoms temporarily and significantly worsen) especially during season change, exposure to dust, air pollution or environmental irritants, and during stress, illness or infections. Though asthma and chronic bronchitis may present similarly in adults with shortness of breath (difficulty in breathing called dyspnea) and cough, they are different medical conditions.
Asthma occurs due to an abnormal inflammatory response of the airway to specific triggering substances or conditions. These may be due to substances called allergens (as seen in 60-70% of cases of asthma that are allergic) which are otherwise harmless and do not affect the general population. Known allergens include dust (house dust mite), pollen, certain food items, fungi, Insects, and animal dander. Other specific triggers include irritant substances, drugs, infection, temperature changes, physical activity, stress, etc. COPD (chronic bronchitis) occurs due to an inflammatory response of the airway to slow and long-term exposure to irritant substances like smoke, tobacco, industrial/factory chemicals, or environmental pollutants over a period of time.
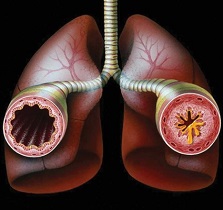
The inflammation in both conditions causes narrowing of the bronchi (bronchoconstriction) which leads to difficulty in breathing and cough. Though the primary response in asthma is to allergens, it can get worsened by environmental irritants. Also, a person with asthma can later develop COPD due to smoking or long-term irritant exposure, and the term ACOS (Asthma COPD Overlap Syndrome) is used in these cases.
Differences between Asthma and COPD
- Asthma that is allergic usually starts in childhood (other types of asthma may start in adulthood) while COPD starts in late adulthood, and is seen more in elderly people.
- Asthma is commonly associated with a family history of asthma itself or other allergies of the nose (allergic rhinitis) or skin (eczema/ atopic dermatitis). COPD may not be linked to family history, but there is commonly a history of smoking or occupational or environmental exposure to irritants.
- The cough in asthma is usually dry and not associated with much phlegm (sputum with mucus), however, an increase in phlegm may be seen during a respiratory infection. In COPD, the hallmark is a productive (wet) cough with the presence of large amounts of phlegm which the patient needs to constantly bring out.
- Asthma is typically worse in the late night or early mornings. In COPD, cough with increased phlegm on waking up in the morning is characteristic, with symptoms persisting throughout the day. Wheezing (a whistling sound due to breathing through a narrow airway) and feeling of chest tightness are more common with asthma.
- At a cellular level, the predominant type of immune cells (white blood cells-WBCs) found in the asthmatic airway are eosinophils (with IgE antibodies), while in COPD they are neutrophils (with IgG antibodies).
- Asthma is intermittent and reversible in nature and is not a progressive condition. It may even get better with age or time. COPD is a progressive condition with the bronchi getting irreversibly narrower, and symptoms worsening over time. Finally, the progressive inflammatory damage in COPD involves the air sacs in the lungs where gaseous exchange happens (a condition called emphysema), reducing the oxygen delivery by the blood to different organs.
- Asthma by itself is not life-threatening or dangerous, and most patients lead a fulfilling life controlled well on medications (mainly inhalers). COPD can greatly reduce the quality of life and exertional/working capacity. As COPD progresses, it can lead to serious complications like lung damage (emphysema) and increased stress on the heart resulting in gradual right-sided heart failure. The risk of developing respiratory infections like pneumonia and resulting complications or mortality is far higher in COPD patients.
DIAGNOSIS
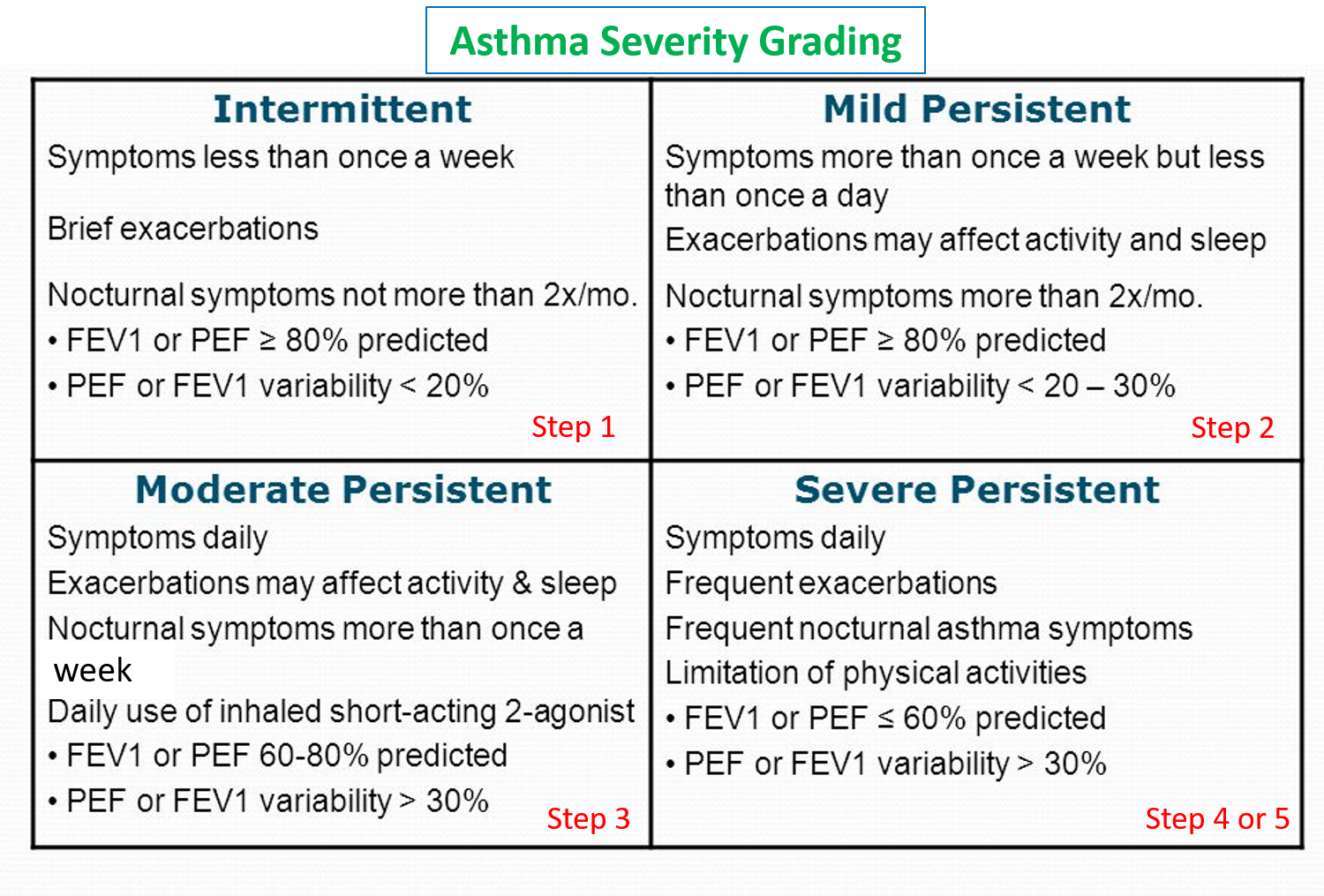
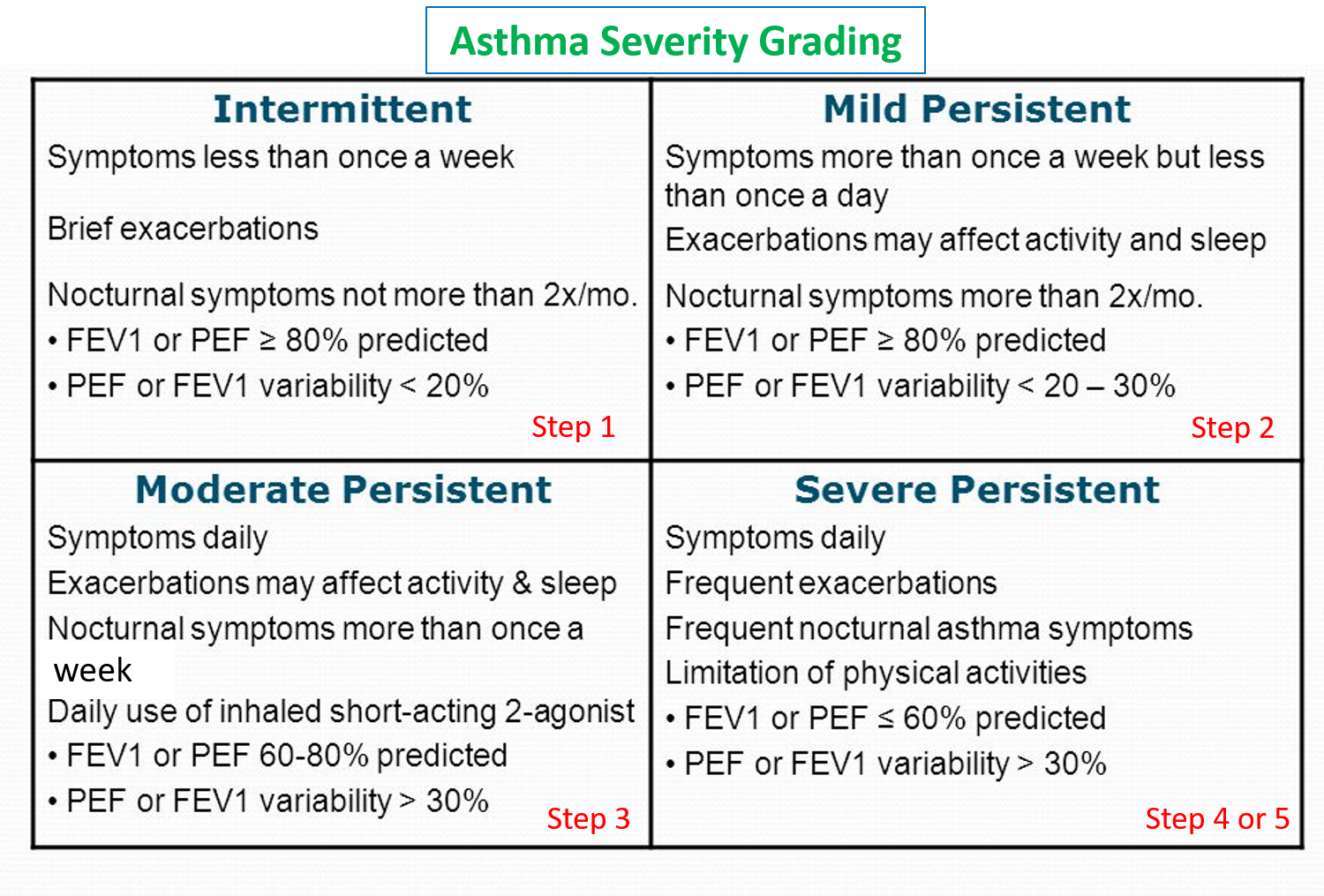
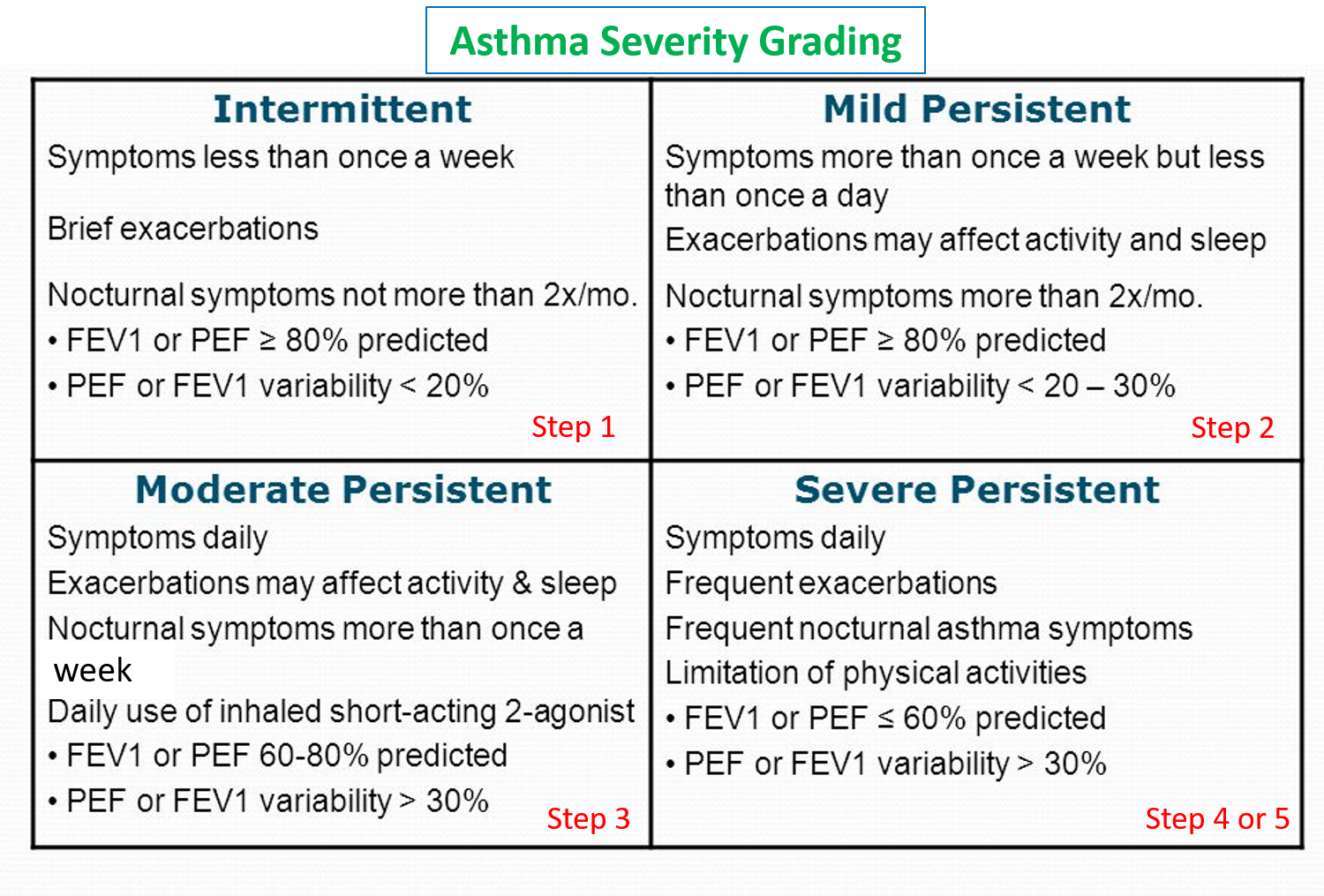
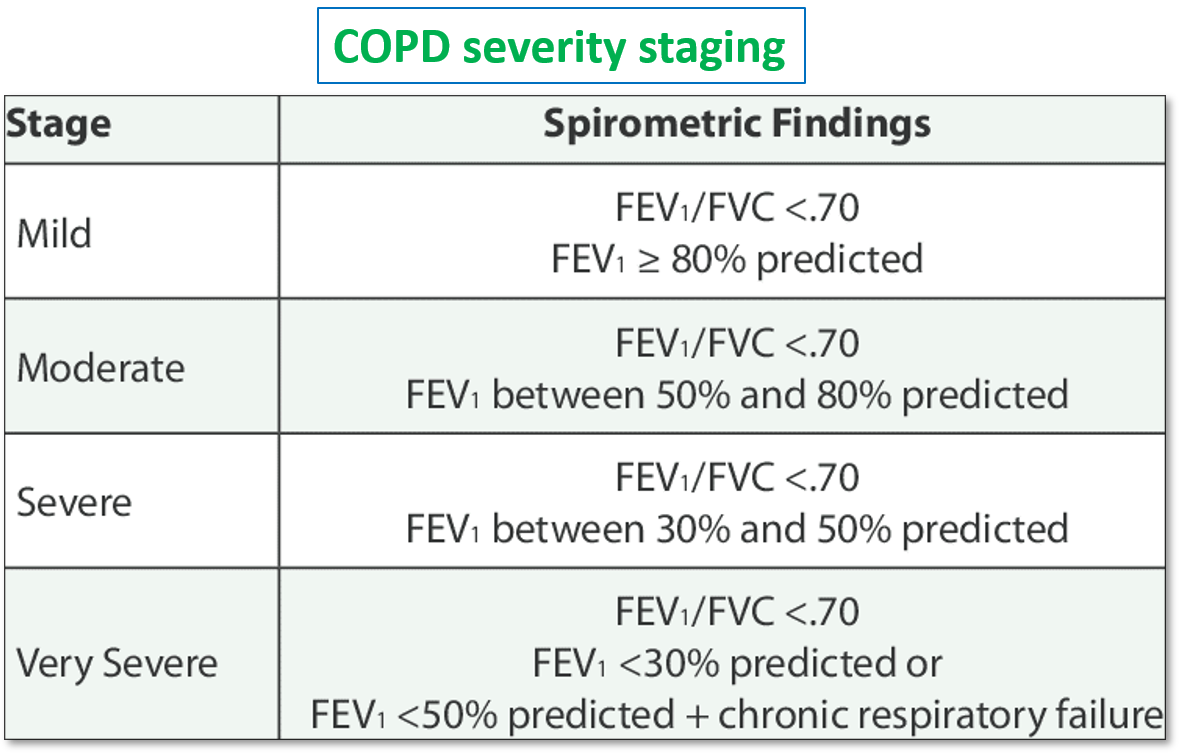
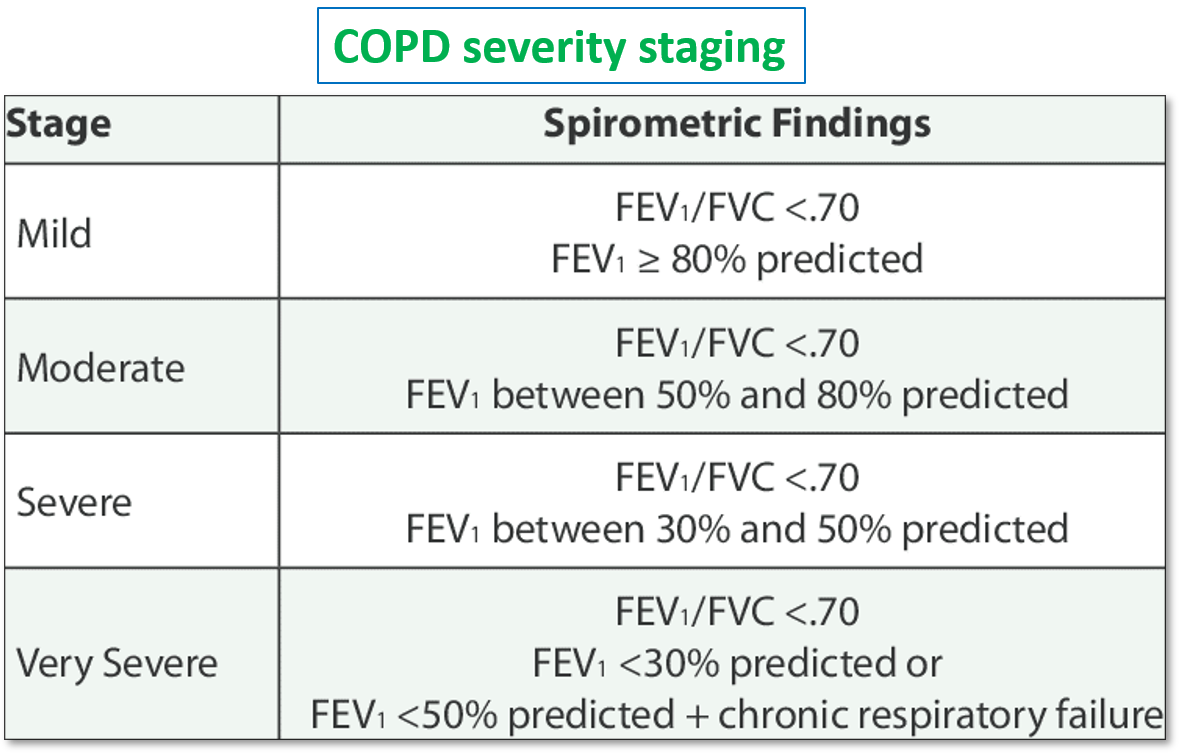
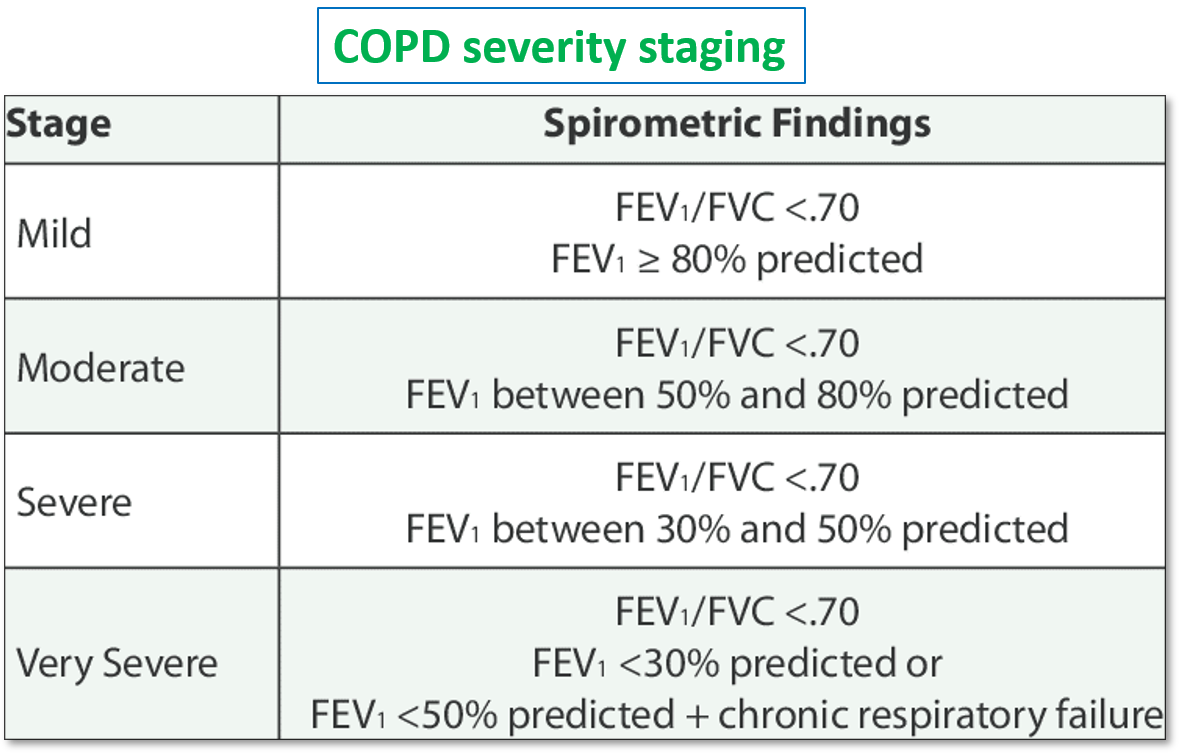
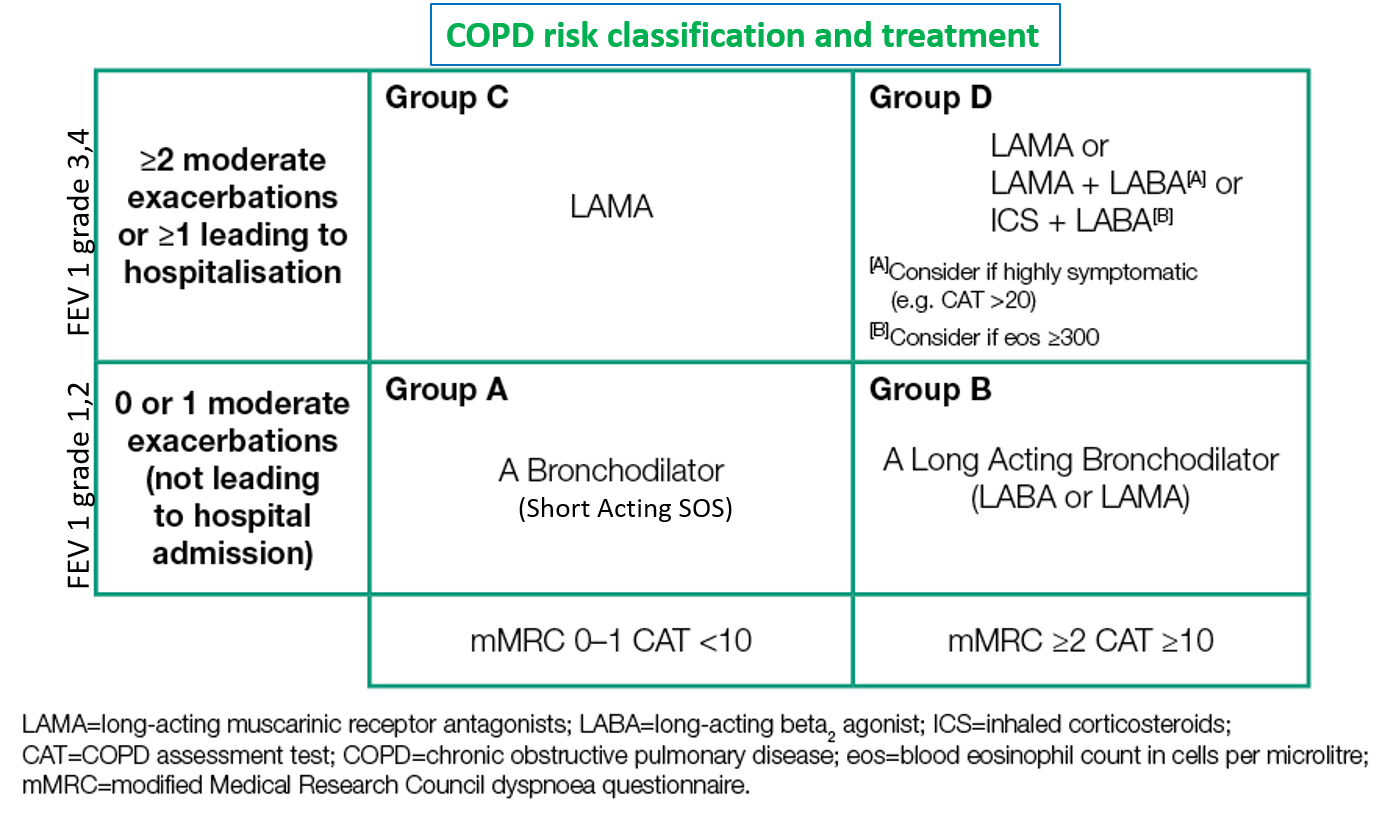
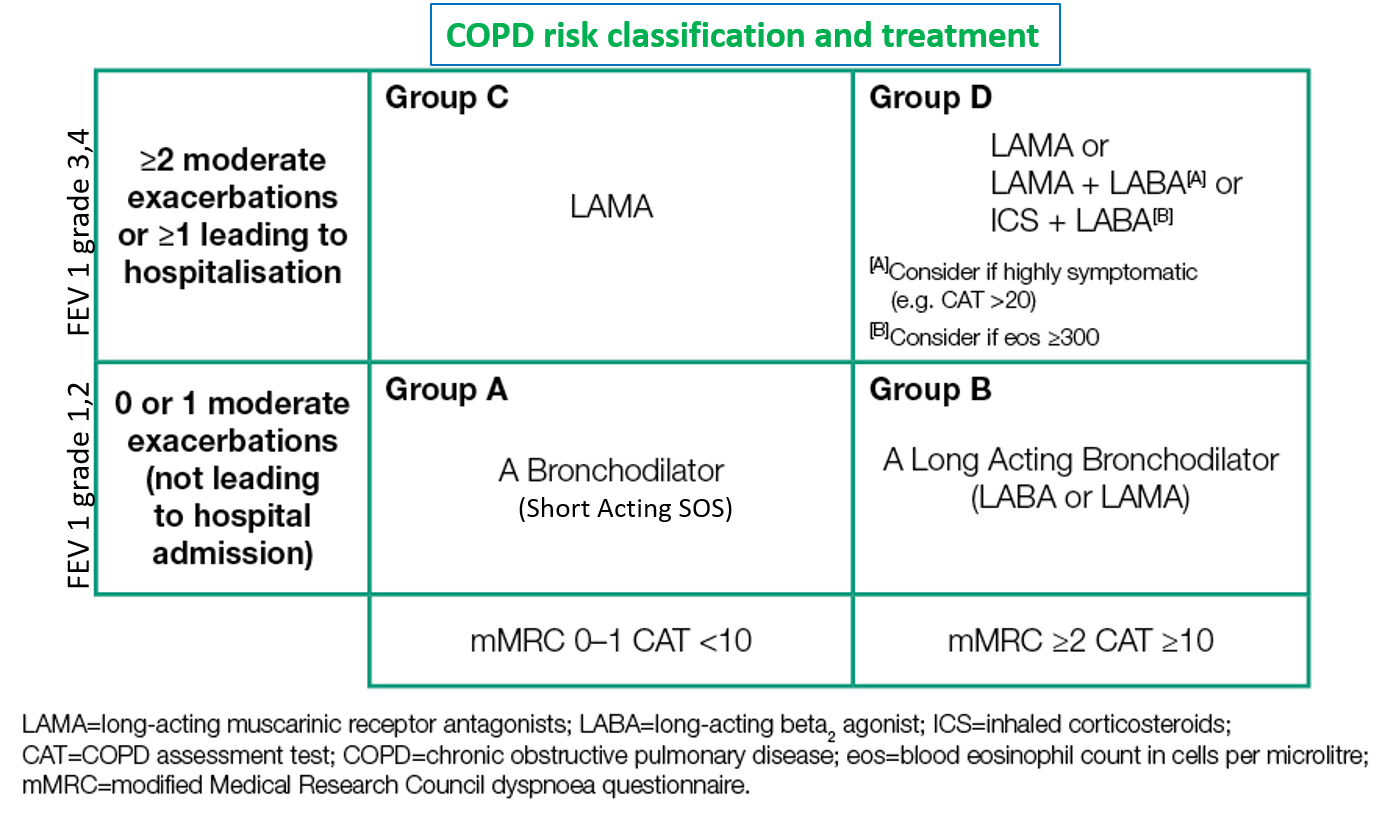
The treating physician may perform certain tests including blood and sputum tests, and evaluation of lung function (pulmonary function tests – PFT) by spirometry to assess the flow and pressures in the airway. Asthma and COPD are classified and their severity is graded in accordance to the parameters on spirometry (forced expiratory volume in first second FEV1, forced vital capacity FVC, and peak expiration flow PEF), symptoms or exacerbation frequency, and impact on activities of daily living (quality of life).
Refer: Pulmonary Function Tests.
HOLISTIC HEALTH SOLUTIONS
Management has to be a combination of lifestyle measures and regular medication.
Allergen and Irritant Avoidance:
Though this may be practically difficult sometimes, it is one of the cornerstones of managing airway diseases. For asthma, one can understand the causative allergen with experience or maintaining a symptom diary, for example, exposure to dust or seasonal pollen triggering an attack.
Smoking should be given up. If industrial or occupational exposure is inevitable, change of job profile or wearing appropriate protective masks along with regular washing of nose and mouth should be followed. Residences on the roadside or near highways or factories can also increase exacerbation episodes in asthma and COPD.
Physical Activity
Physical activity (PA) and exercise are integral to health and maintenance in asthma and COPD patients and can improve treatment outcomes, while a sedentary lifestyle is a risk factor for frequent exacerbation episodes as well as worse symptom control. However, it should be kept in mind, that exercise is one of the known triggers of an asthma attack, and also COPD patients may have a low capacity to exercise due to reduced oxygen availability Therefore it is important to keep some points of care in mind while adapting an exercise or PA regime into one’s daily routine.
Know the Points of Care during Physical Exercise to be taken.
Aerobic exercises that use large muscle groups (like walking and yoga) are recommended instead of running or cycling. Strengthening exercises for the upper body, including using light weights and resistive bands, may be particularly helpful in patients with COPD because they help to increase the strength of respiratory muscles. Yoga poses like the standing mountain pose (standing tall with arm raised as much backward, to open up your chest), and standing backbends (performed very gradually) can help expand the chest to increase lung capacity.
Breathing Techniques
Practicing some breathing techniques regularly can help enhance lung capacity, decrease breathlessness and exacerbations. Here are 3 effective breathing techniques to practice.
Diet
A balanced and nutritious diet is important. Obesity or being overweight is associated with a risk of frequent exacerbations and inadequate symptom control, therefore such people can benefit by dropping 3-5 kg weight through a structured diet program. Diet should be rich in fruits and vegetables, with good amounts of proteins and whole grains.
Patients with asthma or COPD should reduce intake of refined sugars, dairy items, excess salt in food, spicy-fried-oily items, and foods that cause gas/bloating. Food items should be warm or at room temperature (not cold) and should preferably be freshly cooked. Overeating or very heavy meals can worsen both bloating and breathlessness.
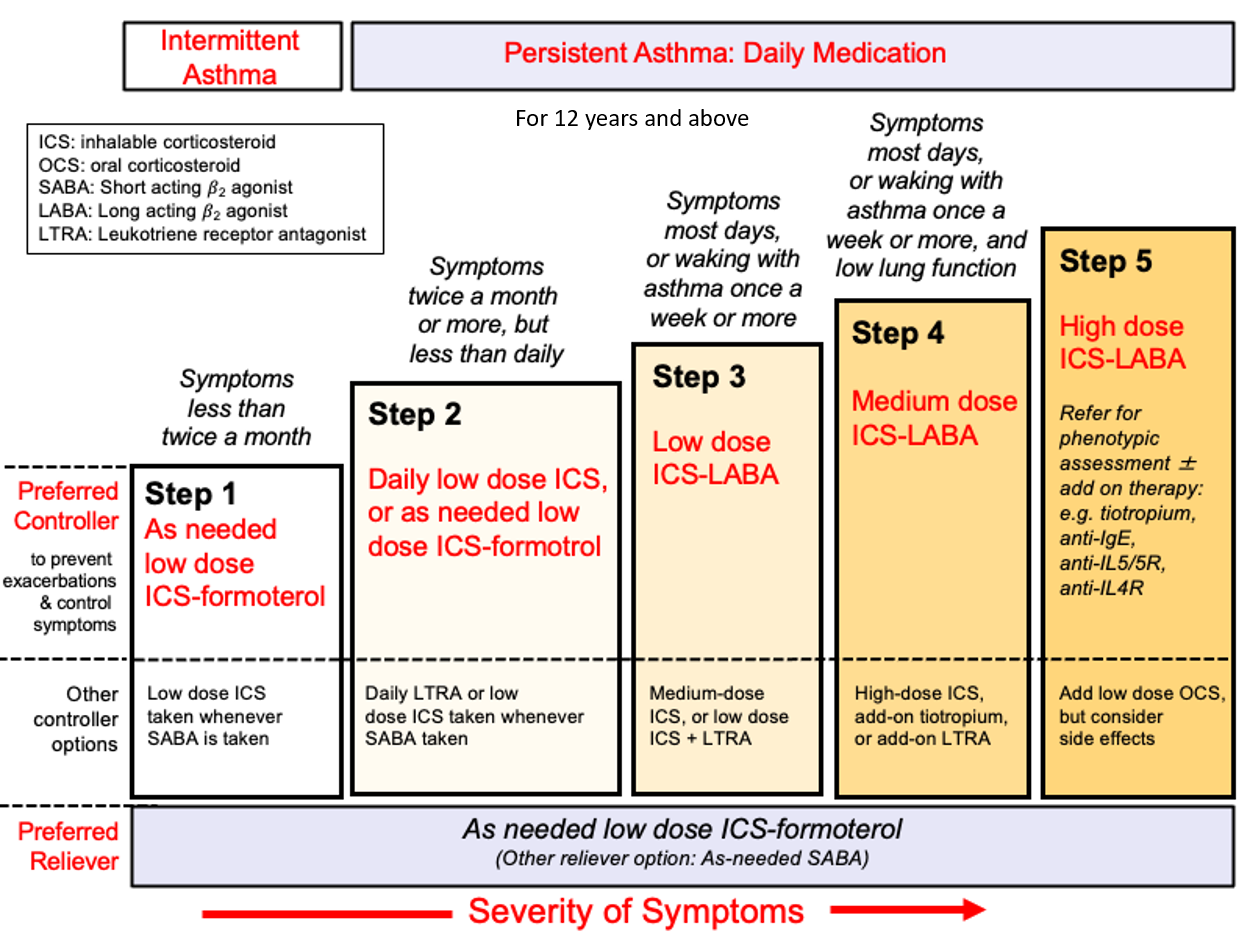
Medications
It is important to take medications regularly according to the prescribed timing and dose. Follow-up should be regular with the treating physician for evaluation of symptom control and lung function.
Inhalers
The mainstay for asthma and COPD treatment is inhalers. They are most effective, and easy to use with excellent acceptance and tolerance. Inhalers can be either DPIs (Dry Powder Inhalers) or MDIs (Metered Dose Inhalers). In DPIs, a capsule containing the drug dose in powder form is inserted into the inhaler and the powder is inhaled through a deep breath. While in MDIs, the drug is in the inhaler and is inhaled as an aerosol. Sometimes a spacer may be added to the inhaler to take in the drug more easily, especially in children. Using a nebulizer is another method of effectively giving inhalational medicines where the medicine is inhaled as a mist through a mask.



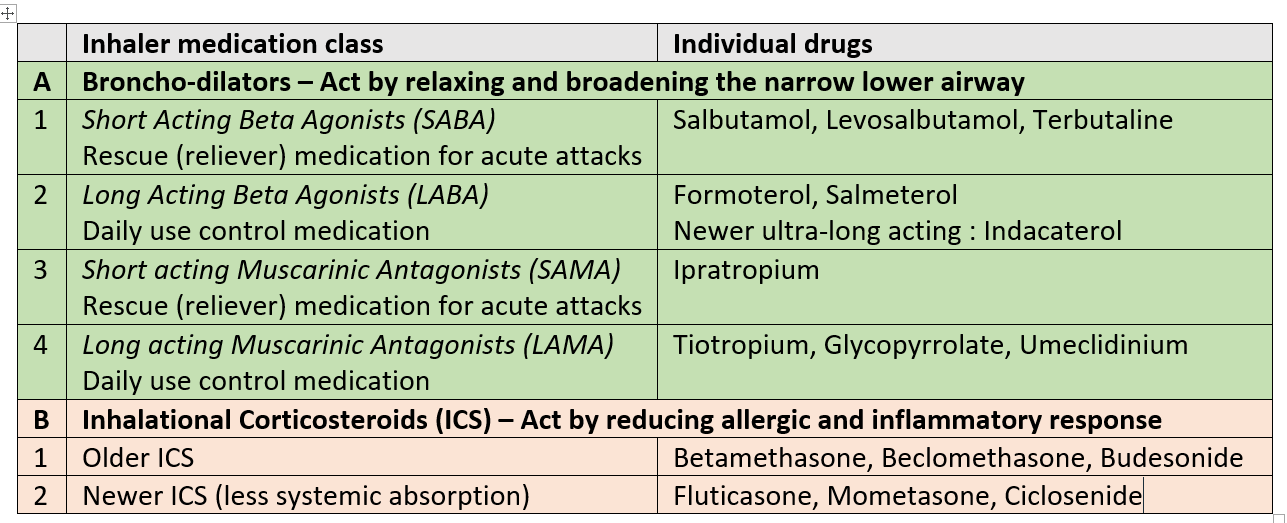
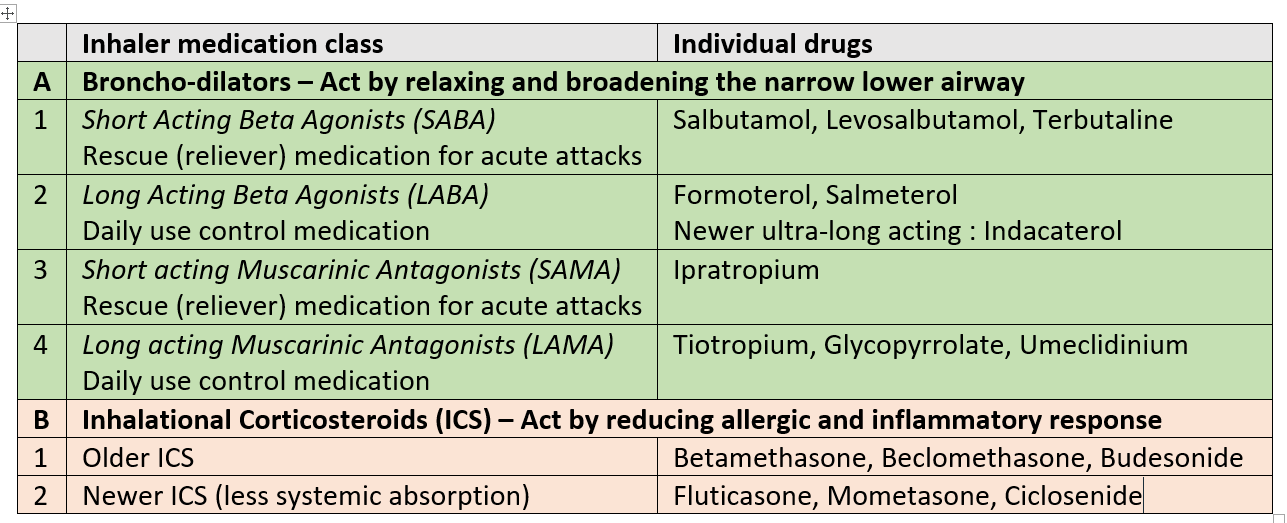
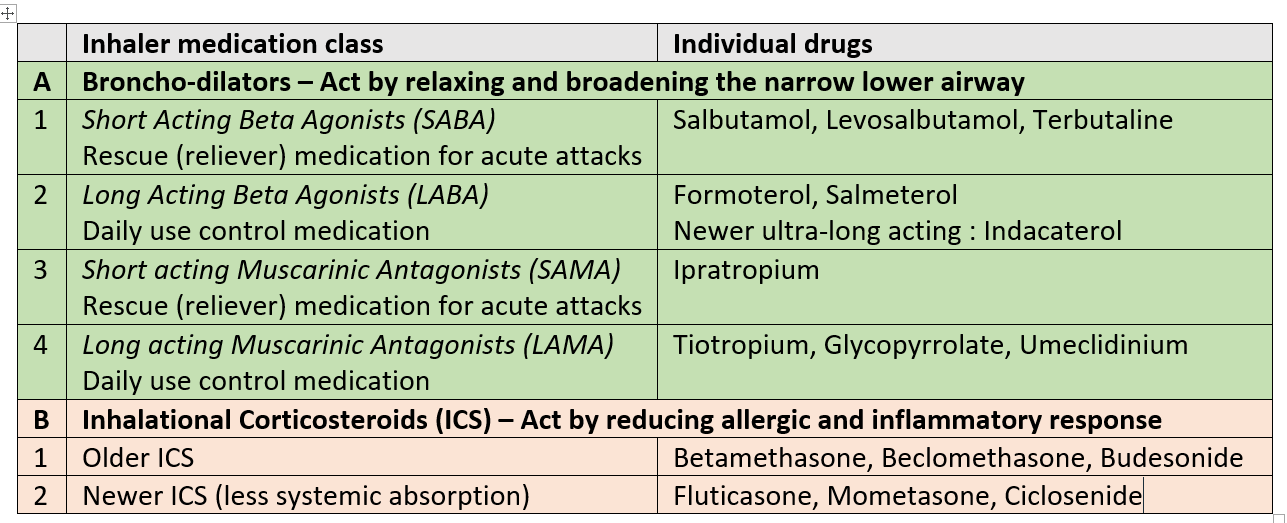
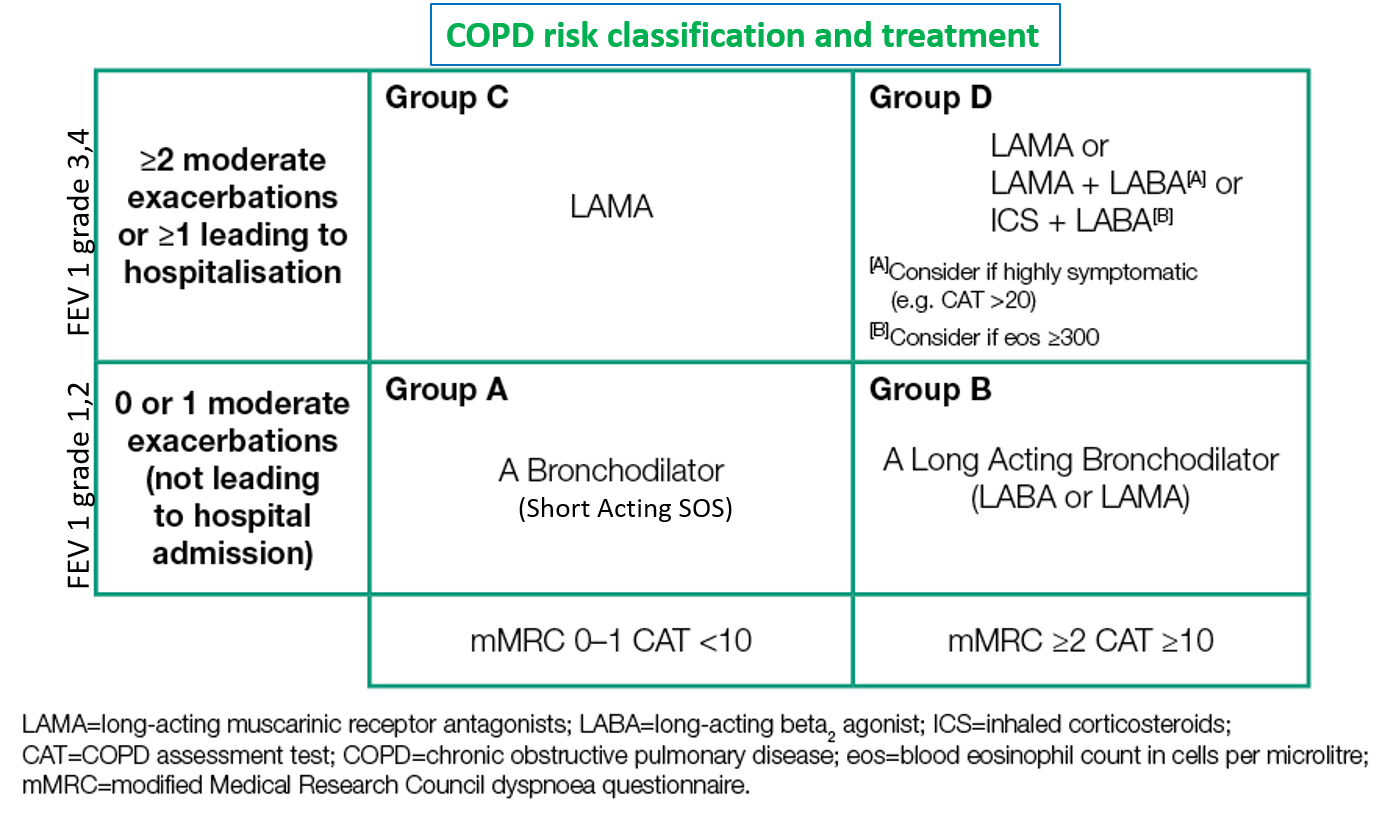
SABA and SAMA are used as reliever inhalers during breathlessness or worsening of symptoms. LABA, LAMA, and ICS are given as regular long term controller inhalers.
Note – Combination inhalers are commonly prescribed (SABA-SAMA, LABA-LAMA, LABA-ICS, LABA-LAMA-ICS). Other ultra long acting once a day LABAs like Olodaterol, and Vilanterol (in combination with ICS -Fluticasone) are also approved and available in some countries.
Advanced cases of COPD may require oxygen therapy
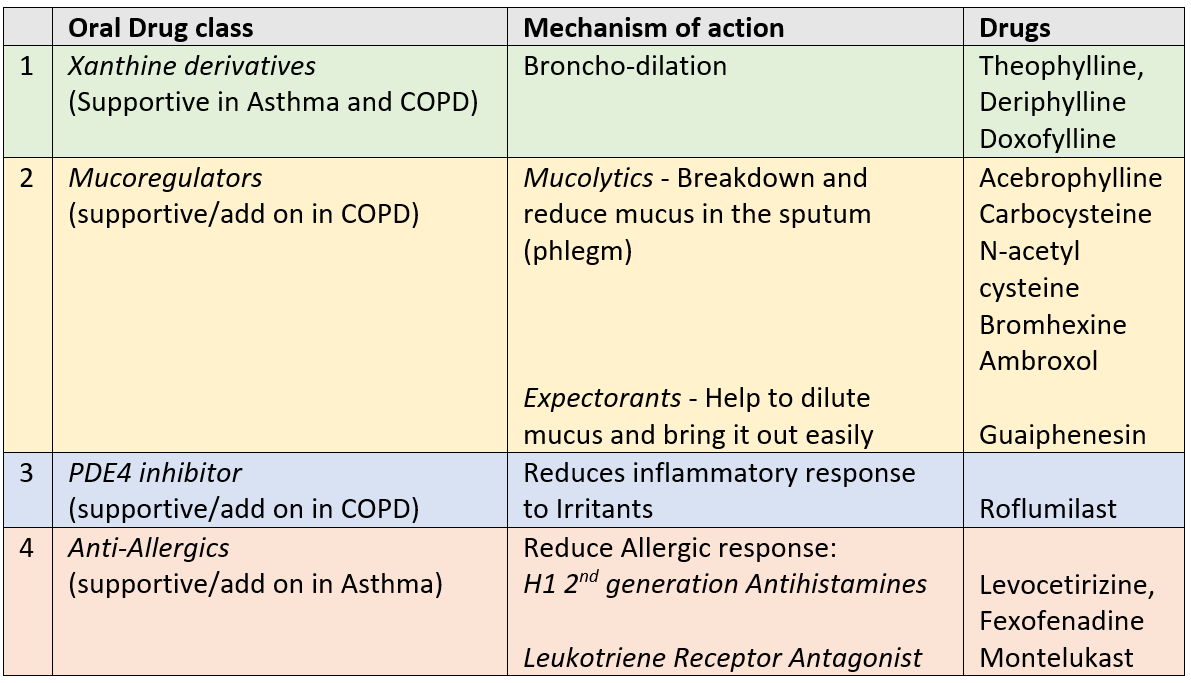
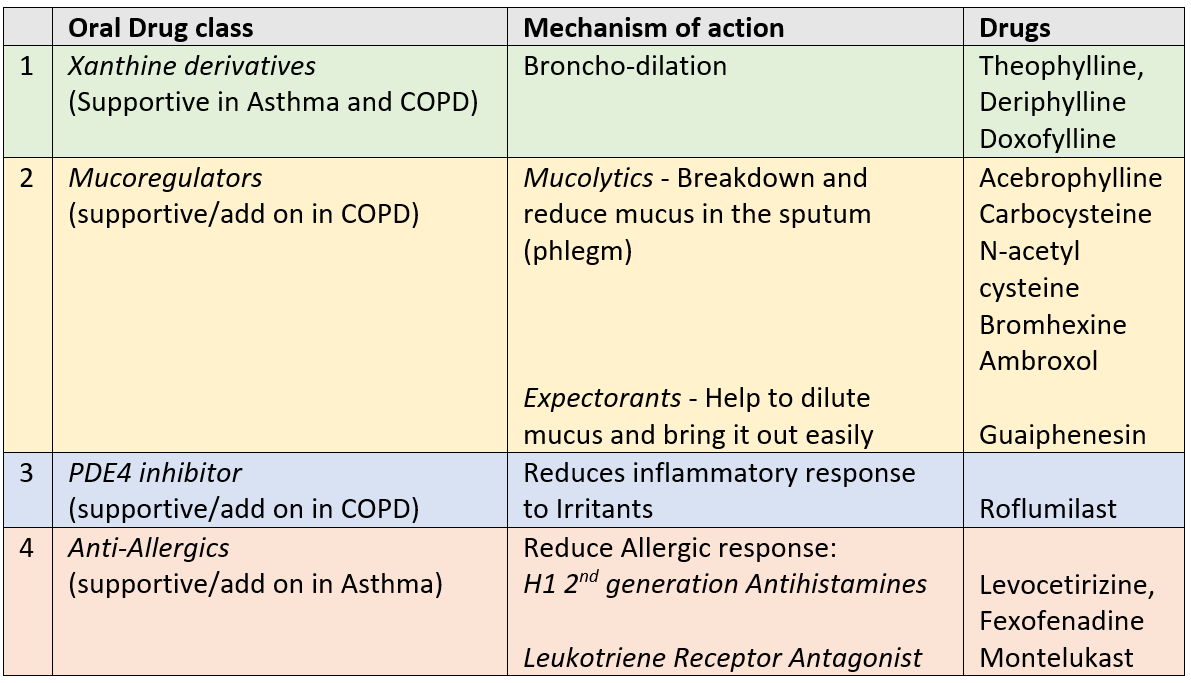
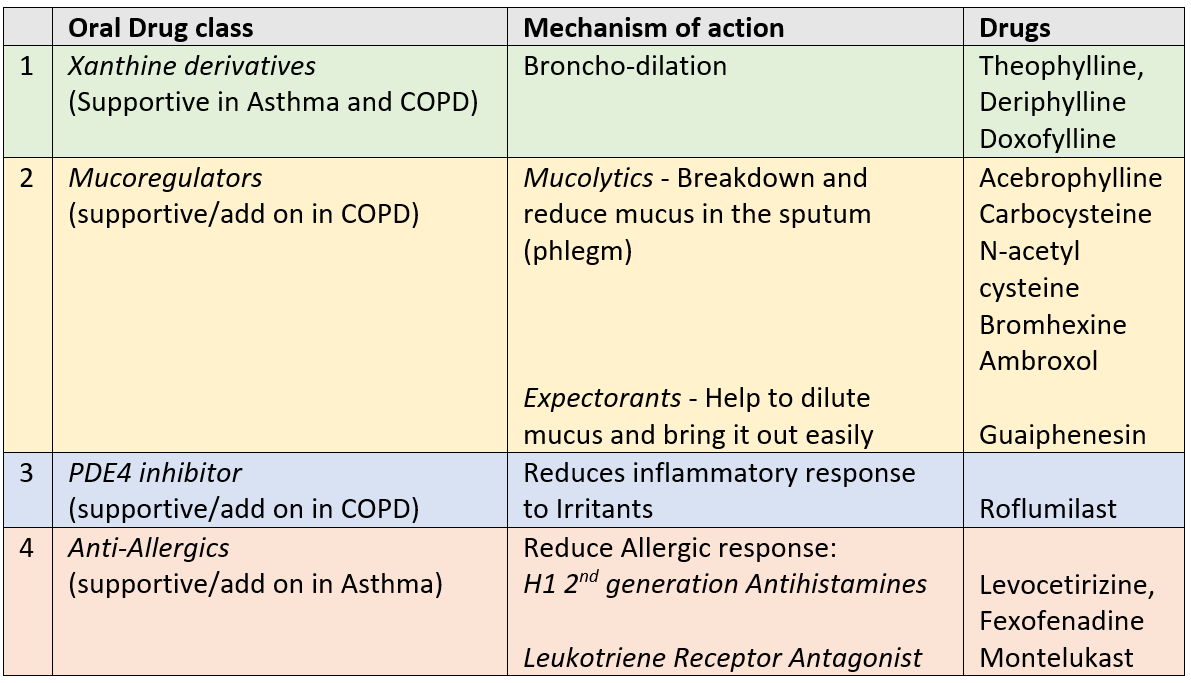
Oral medicines
Oral medications may be prescribed as an add-on during times of exacerbations, infection or physical stress for better symptom control.
Biologicals
Biological injections (MAbs) act by targeting specific cytokines (called interleukins- IL), which are inflammatory messenger proteins implicated in airway inflammation in asthma. These include omalizumab (anti IgE) and newer ones approved in some countries like mepolizumab, reslizumab, and benralizumab (anti IL5), and dupilumab (anti IL4 and IL13). These are indicated in severe and uncontrolled asthma cases.
The US FDA recently approved tezepelumab, the first biologic that targets the airway epithelial cytokine thymic stromal lymphopoietin (TSLP), for severe asthma as an add-on maintenance treatment of adult and pediatric patients aged 12 years and older.
ASTHMA SEVERITY GRADING, CLASSIFICATION, AND TREATMENT
COPD SEVERITY GRADING, CLASSIFICATION, AND TREATMENT
Also read:
3 Effective Techniques to improve Breathing capacity and control
For any query, additional information or to discuss any case, write to info@drvarsha.com, and be assured of a response soon.
REFERENCES
American Academy of Allergy, Asthma and Immunology: Asthma and COPD- Differences and Similarities