Abnormal uterine bleeding (AUB) implies abnormal menstrual bleeding (menses or periods) in terms of frequency, regularity, duration, or amount of bleeding.
Dysfunctional Uterine Bleeding (DUB) is the term used to describe AUB related to changes and possible imbalances in hormones that directly affect the menstrual cycle. It is diagnosed after other conditions causing AUB are ruled out.
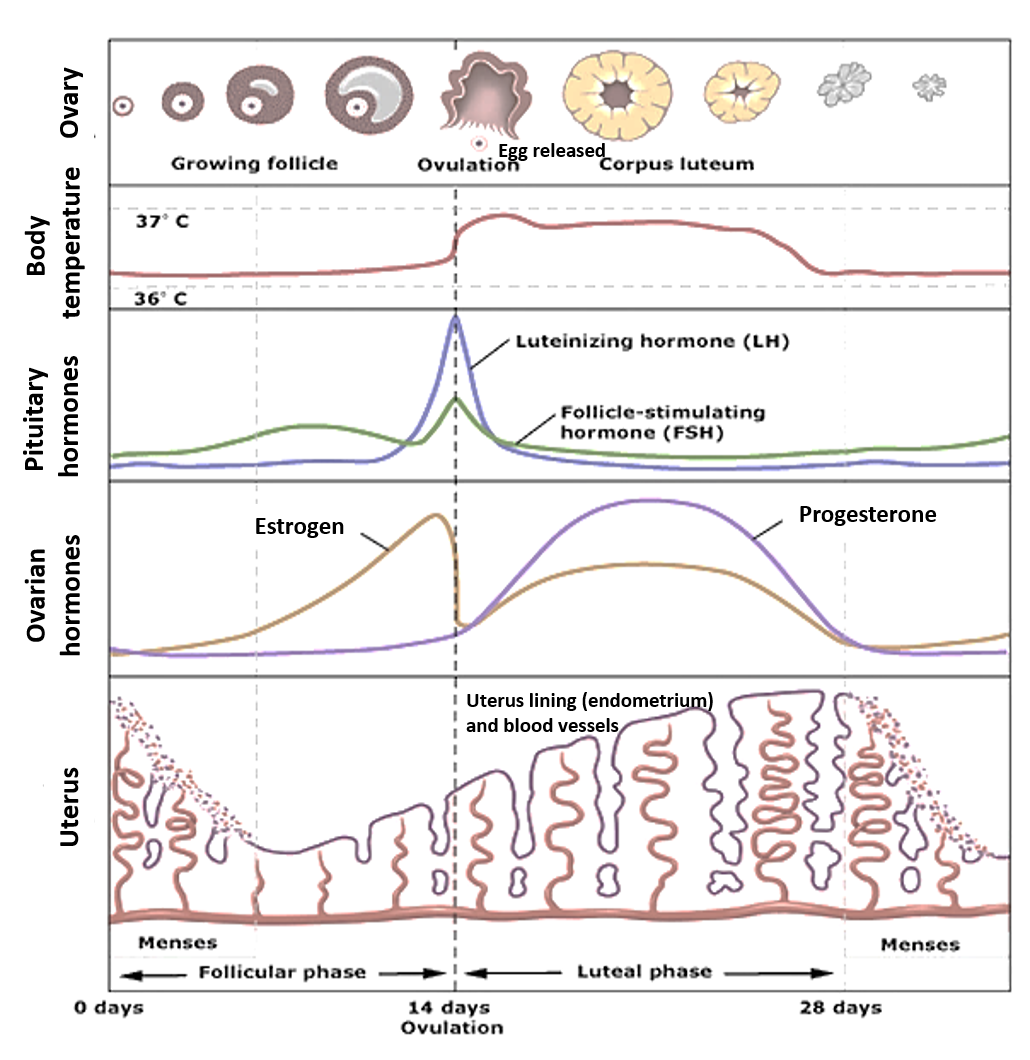
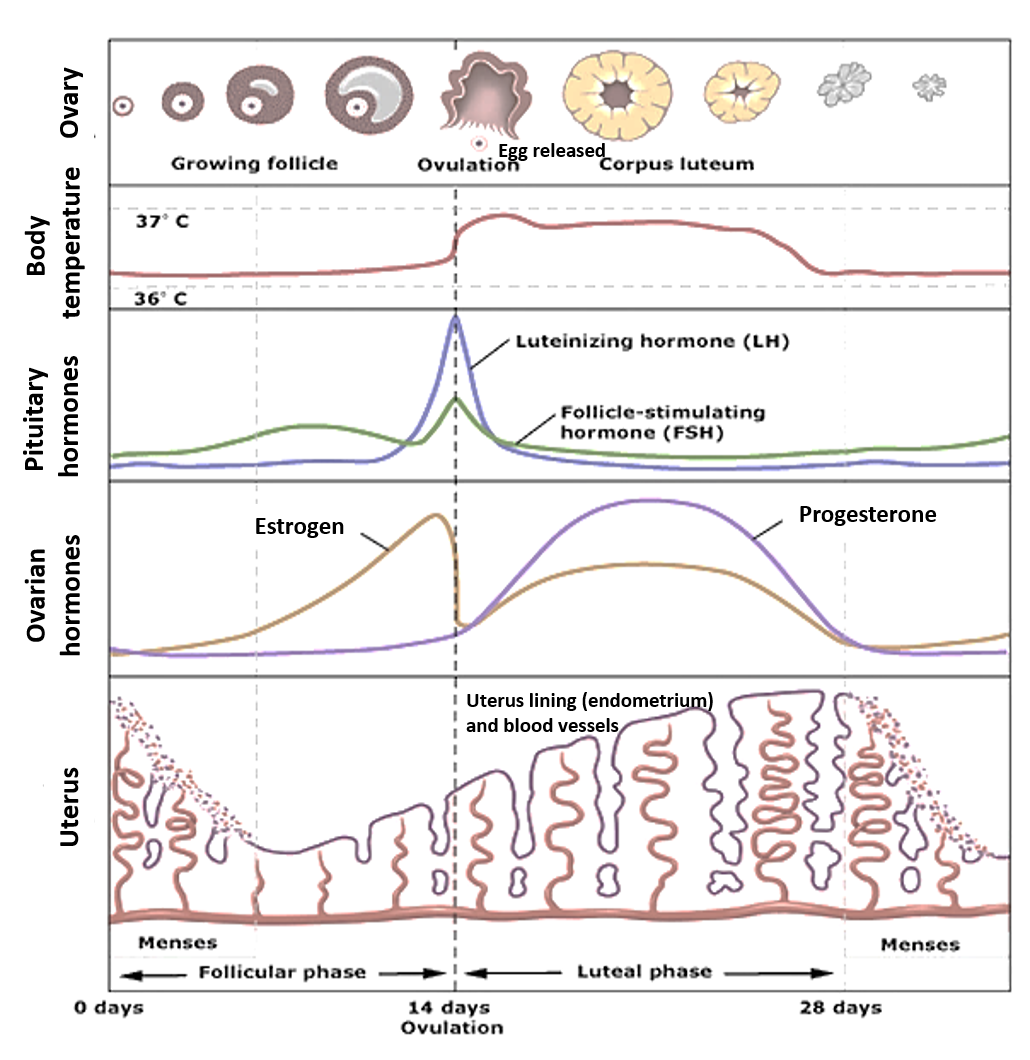
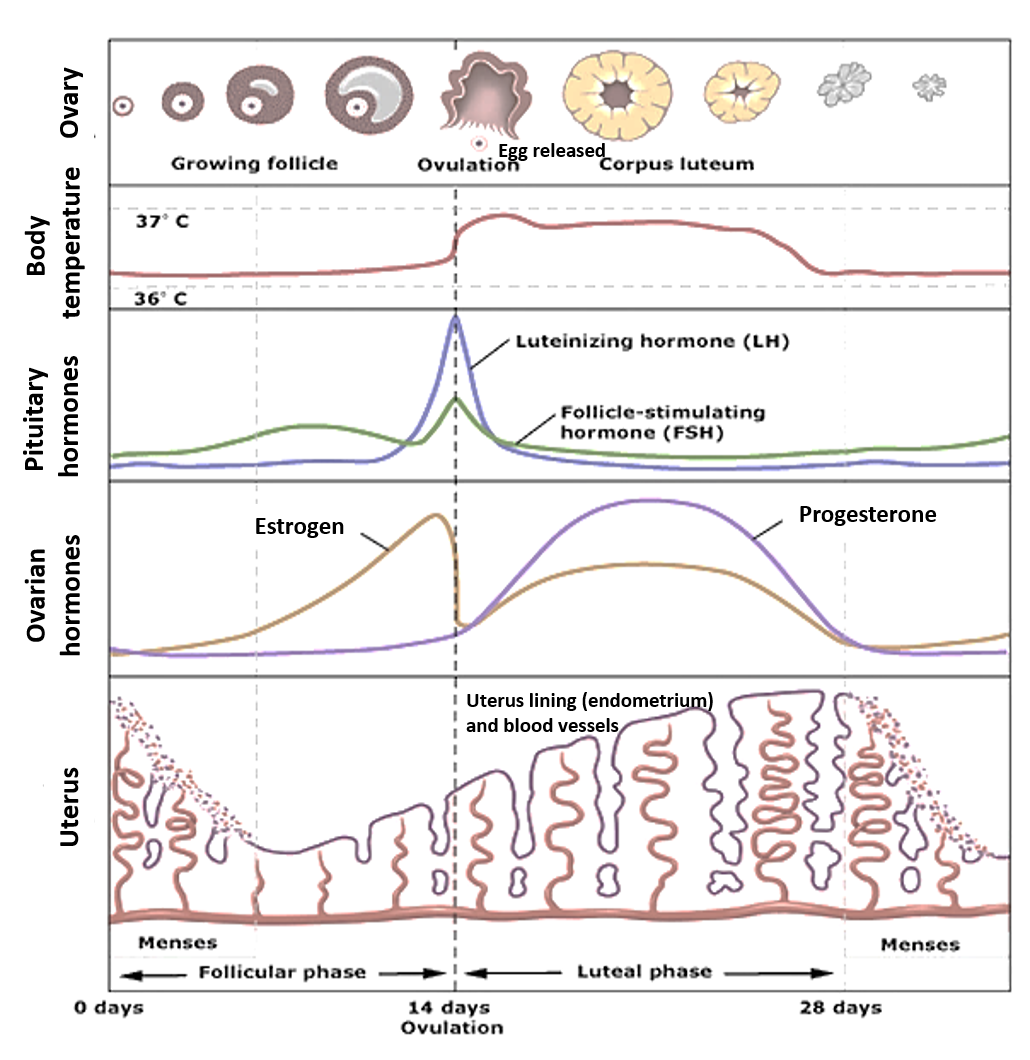
Understanding the Menstrual Cycle
The female reproductive parts include the 2 ovaries and tubes (fallopian tubes) on either side, entering the uterus (womb) which leads down to the cervix and the vagina. Each of the ovaries contains a round aggregation of cells forming sacs called follicles, each of which contains an egg, and one of these follicles releases an egg (ovulation) every month. After the egg is shed, the left-over collapsed follicle is called corpus luteum.
A woman’s menstrual cycle is an interplay and balance of hormones and changes in the ovaries and the uterus. The ovarian hormones estrogen (produced by the developing follicle) and progesterone (produced by the corpus luteum) are dominant respectively in the stages of menstruation before (follicular phase) and after (luteal phase) ovulation. These hormones are regulated by other hormones called gonadotropins (follicle-stimulating hormone- FSH, and luteinizing hormones-LH) released from the pituitary gland at the base of the brain. The gonadotropin hormones are in turn regulated by gonadotropin-releasing hormone (GnRH) from the hypothalamus in the brain.
Estrogen helps in the development of the follicles and the egg contained in them till one of the follicles ‘ripens’ and is ready to release the egg. Estrogen level thereafter drops and a surge in the LH hormone causes the egg to be released (ovulation). The remaining follicle now called the corpus luteum produces progesterone the levels of which rise to further thicken the lining of the uterus (endometrium) and increase its blood supply. If conception does not occur, progesterone levels fall, and menses (bleeding) start to shed the thickened lining and extra blood supply.
As progesterone supports the lining of the uterus, its relative deficiency can cause earlier, heavy and prolonged periods (AUB).
A normal menstrual cycle has a usual frequency of about 25-35 days and lasts around 5-7 days.
INCREASED MENSTRUAL BLEEDING
This refers to menses that are heavier, longer than usual, or that occur at a frequent or irregular time.
Most of the terminologies below have been used for several years and so continue to be used even today, however, have been abolished for the preference of simpler more descriptive terms by recent medical association guidelines.
Menorrhagia refers to heavy or prolonged periods. Heavy bleeding usually implies the need to change the tampon/pad in less than 1-2 hours (or the requirement for double padding or changing pads through the night). It could be associated with the passage of large clots (more than one-quarter pad size). A prolonged period refers to the bleeding lasting more than 1 week. Menorrhagia can in some cases be associated with dysmenorrhea (cramping pains).
Polymenorrhea is a term used to describe a menstrual cycle that is shorter than 21 days. When present with menorrhagia, it is called polymenorrhagia.
Hypermenorrhea is often used interchangeably with menorrhagia and refers to increased blood volume (>90ml) lost in one menstrual cycle.
Metrorrhagia is abnormal bleeding that occurs between periods or bleeding not associated with menstruation. If it occurs with menorrhagia, it is called menometrorrhagia.
Around 5-10% of women suffer from increased bleeding and heavy periods, which can have a significant impact on their quality of life, activities, and productivity during the period, and cause fatigue, weakness, and anemia.
CAUSES
- Hormonal imbalance, especially a relative deficiency of progesterone may occur in cycles not shedding eggs (anovulatory cycles). This is often seen as polymenorrhagia in adolescents who have recently started periods (Anovulatory AUB), those on estrogen hormone treatment, or intense physical/mental stress.
- Polycystic ovary syndrome (PCOS)
- Endometriosis
- Benign growths like fibroids (leiomyoma) and polyps in the uterus
- Adenomyosis (glands from the uterus lining called endometrium get incorporated into the uterine muscle)
- Using an Intrauterine device for contraception
- Miscarriage (especially if a heavy period comes late) or threatened/incomplete abortion
- Ectopic pregnancy (fetus growing in abnormal place outside uterus like in the fallopian tubes)- a medical emergency
- Infection/inflammation of the uterus, vagina, cervix, or pelvic organs (PID-pelvic inflammatory disease)
- Diabetes or disorders of thyroid, kidney or liver
- Cancers – uterine, cervical or ovarian
- Inherited bleeding disorders, clotting factor deficiency
- Blood thinner medications (anticoagulants)
DIAGNOSIS
Usually, increased menstrual bleeding happening once in a while and mainly on the first 2-3 days of the period can be managed with rest, reassurance, relaxation and stress reduction and analgesics (pain-relieving medicines) if there is associated menstrual cramps. However, if this increased bleeding occurs as a regular feature, it is advisable to get a few tests done.
These tests include a physical and gynecological examination, blood tests (complete blood counts, blood sugar, and thyroid, kidney, liver function), a Pap test and an ultrasound. Further tests may be advised if needed (like hysteroscopy/hysterography and endometrial biopsy).
TREATMENT
A healthy diet, regular physical exercise and stress management go a long way in managing heavy periods and increased menstrual bleeding.
Medicines are prescribed to:
1. Balance hormonal levels and regularize periods
- oral contraceptives
- progesterone or progestins (synthetic progesterone) – as oral tablets, injections or intrauterine devices (IUD)
- GnRH agonists – as injections/nasal spray for short-term use in severe/non-responsive cases
2. Reduce bleeding (tranexamic acid, mefenamic acid)
3. Reduce associated pain when present (NSAIDs like mefenamic acid, naproxen, and antispasmodic medicines like dicyclomine, and drotaverine)
4. Treat and prevent anemia (iron-folic acid-B12 supplements)
If a specific condition (as listed in causes) is diagnosed, it should be treated with the recommended therapy or where needed the appropriate procedure/surgery. Sometimes the menorrhagia is non-responsive to common treatments, so in such cases, procedures/surgery (like dilatation and curettage D&C, uterine artery embolization, laser/radiofrequency/balloon ablation, myomectomy, endometrial resection, focused ultrasound surgery or sometimes removal of the uterus- hysterectomy) may be performed by trained and skilled medical experts/gynecologists.
DECREASED MENSTRUAL BLEEDING
This is also called infrequent AUB, (or oligomenorrhea) which implies infrequent menses almost always at an interval of more than 35 days or having less than 9 periods a year in adults (for adolescents it is defined as less than 4 periods in 1st-year post starting menses, less than 6 periods in 2nd-year post starting menses, and less than 8 years in the 3rd-5th-year post start of menses.)
Hypomenorrhea is often used interchangeably with oligomenorrhea and refers to decreased blood volume (<30ml) lost in one menstrual cycle.
The causes are sometimes natural like in the first few years after attaining menarche or while nearing menopause, due to hormonal instability. It may also be seen in women taking birth control pills, those who engage in heavy exercise/intense sports or take anabolic steroids to enhance performance, during high mental/physical stress or drastic dietary and weight changes (as may be seen in eating disorders like anorexia or bulimia), and in PCOS. Diabetes and thyroid disorders can also be a cause. High levels of the milk hormone ‘prolactin’ which can sometimes be a side effect of medicines like antipsychotics and antiepileptics, also can cause decreased menstruation. Rare causes include prolactin hormone-releasing pituitary tumors (prolactinoma), androgen hormone-releasing ovarian/adrenal tumors, or anatomical abnormalities of the uterus or cervix.
Decreased menstrual bleeding itself does not need treatment, except for a nutritious diet, appropriate physical activity, reassurance, and in some cases changing the contraceptive pill. More importantly, any underlying or associated health condition should be diagnosed and treated. Pregnancy should be ruled out in all such cases.
Also read:
Ovarian Cysts: Understanding Causes, Diagnosis and Implications
For any query, additional information or to discuss any case, write to info@drvarsha.com and be assured of a response soon.
References: