WHAT IS THROMBOSIS
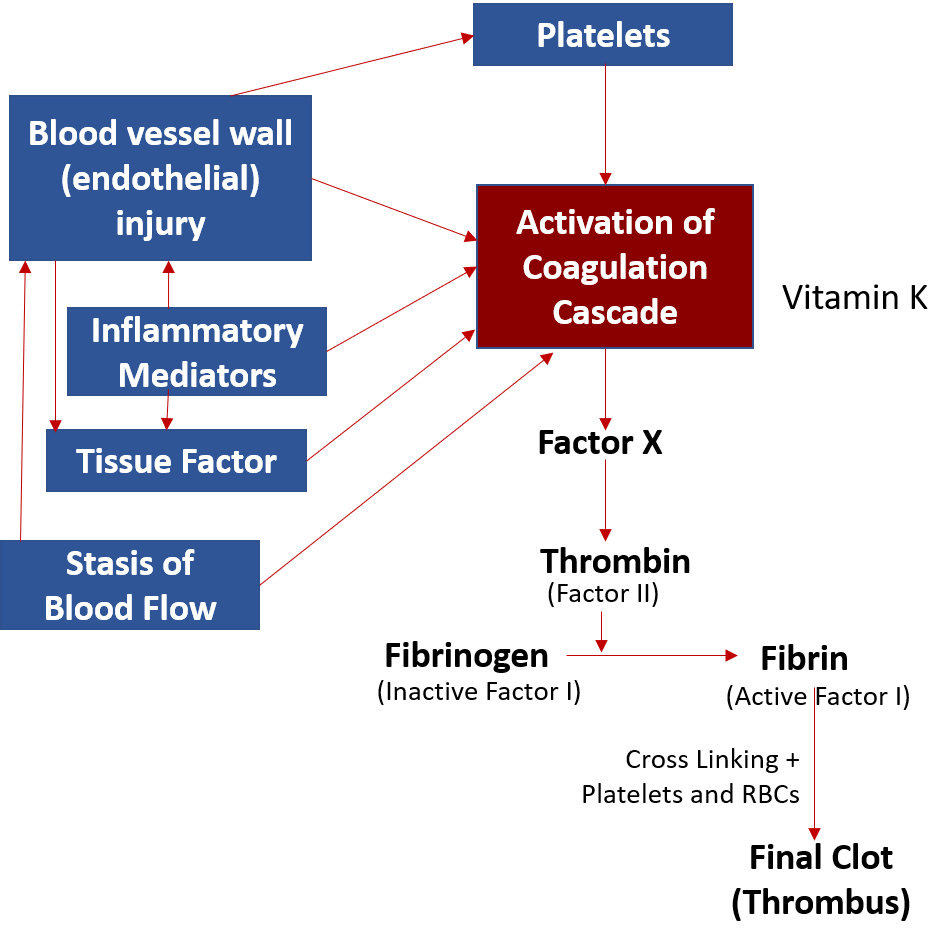
When a clot (thrombus) forms in a blood vessel (artery or vein), it is called thrombosis. Thrombosis or clotting occurs due to an interplay and cascade of activation of coagulation factors (clotting proteins) in the blood. Among these, factor X and factor II (thrombin) form the final common and significant pathways leading to the formation of factor I (fibrin) which cross-links to form the stable clot. Vitamin K plays an important role in the activation of some key coagulation factors, and clot formation.
The body also has anticoagulation factors and plasmin (breaks down fibrin – fibrinolytic) to regulate the clotting process, however, when aggravating risk factors and stimulating mechanisms are dominant, clot formation occurs.
WHAT CAUSES THROMBOSIS
The triad of mechanisms leading to thrombosis, often referred to as Virchow’s triad includes the following –
Blood vessels wall injury – Injury to the vessel wall lining (endothelium) of the blood vessels can be caused by direct trauma but more commonly it occurs over a period of time due to smoking, diabetes, high blood pressure, bad cholesterol (LDL) build-up, and formation of plaques (atherosclerosis) causing cardiovascular disease (CVD). This is seen in arteries where blood flows under high pressure making the endothelium prone to injury. When endothelial injury occurs, there is activation and aggregation of platelets that plug the injury site, and release of a substance called ’tissue factor’, with both of these then activating coagulation factors in the blood to form the clot.
Stasis (stagnation) of blood flow – This is seen to occur more in leg veins due to immobility and impaired muscle action, along with the weakening of the vein valves and wall leading to backflow and pooling of blood (chronic venous insufficiency). Stasis can cause more interaction between clotting factors and also damage the vessel wall over time, leading to more clot formation. Stasis can also occur when the heart is not pumping out blood adequately causing congestion and back-pressure in the veins. This is seen in heart-beat abnormalities like atrial fibrillation and in congestive heart failure.
Hypercoagulability – This refers to conditions in the body that increase the tendency and predisposition of clotting due to high amounts of tissue factor and inflammatory mediators (released during infections, cancers, etc.), or abnormalities in the coagulation or anticoagulation factors.
RISK FACTORS
Stagnation of blood flow (stasis) caused due to prolonged immobilization and inactivity causing decreased muscle action
- Hospitalization (especially if >72 hours)
- Post-surgery (especially hip/knee replacement and major abdominal surgery)
- Post-fractures (especially lower limb)
- Post-trauma (especially with backbone injury)
- Paralysis
- Illness requiring bed-rest
- Long flights or car road trips
- Obesity
- Sedentary desk jobs or lifestyle
- Atrial fibrillation
- Heart failure
- Chronic Venous Insufficiency – varicose veins
Damage to the wall of the blood vessel (endothelial injury)
- Smoking
- Diabetes
- High blood pressure (hypertension)
- Lipid abnormalities – High LDL or triglycerides
- Plaque formation (atherosclerosis) and cardiovascular disease (CVD)
- Infections (like COVID)
- Trauma
- Insertion of an intravenous line (especially central line)
Conditions that increase the tendency to clotting (hypercoagulable state)
- Cancer and chemotherapy
- Major surgeries
- Inflammatory bowel disease (IBD)
- Hormone replacement therapy (HRT) and oral contraceptives
- Clotting disorders (thrombophilia)
- Infections like COVID, and others like measles, chickenpox, flu, dengue, hepatitis, and HIV.
- Cardiovascular disease (CVD)
- Diabetes
- Kidney failure and dialysis
- Chronic Obstructive Pulmonary Disease (COPD)
- Smoking
- Family history of thrombosis
- Pregnancy
- Age>60 years
ARTERIAL THROMBOSIS
When a clot forms in an artery it can obstruct blood flow to the organ being supplied. This becomes dangerous when an artery supplying a vital organ like the heart or brain gets blocked. Thrombosis in arteries is usually due to pre-existing atherosclerosis and cardiovascular disease (CVD), and risk factors like high BP, diabetes, lipid abnormalities, and smoking. These factors cause endothelial injury that leads to the activation of platelets and the clotting proteins in the blood. When such comorbidities are present, factors that increase hypercoagulability like infections (COVID), cancer, surgeries, and other diseases, etc. further add to the clotting risk.
Blockage of the coronary artery and its branches can lead to angina and heart attack (myocardial infarction-MI), while blockage of an artery supplying part of the brain can lead to stroke.
In patients with a high risk of thrombosis or previous cardiovascular events like MI/stroke or those who have undergone angioplasty/bypass surgery, medicines to block platelet action (aspirin, clopidogrel, ticlopidine) are given. In very high-risk cases, an anticoagulant (drug inhibiting coagulation factors) is also added. In case a clot needs to be dissolved urgently as in MI or stroke, agents called thrombolytics are used. Procedures and surgeries like angioplasty and bypass grafting are done in CVD to open the blocked artery or bypass it, respectively.
See below – Medicines for prevention and treatment of thrombosis.
VENOUS THROMBOSIS AND THROMBOPHLEBITIS
The formation of a clot in any vein is called venous thrombosis. Conditions causing venous stasis and hypercoagulability are the main cause of venous thrombosis. Inflammation of the vein is called phlebitis which can occur due to direct trauma to the vein during surgery or placing a catheter, or more commonly as a result of a blood clot when it is called thrombophlebitis. The most common sites of thrombosis and thrombophlebitis are the leg veins followed by the arm.
Thrombosis can occur in both superficial and deep veins, but it is deep vein thrombosis (DVT) that is more dangerous due to the risk of ‘embolism’. A clot formed in a vein is attached to the inner wall of the vein, but sometimes a part of it can break loose (embolus), reaching the heart and then the lung (pulmonary embolism –PE) which can even be fatal. DVT and PE are together called venous thromboembolism (VTE).
SIGNS AND SYMPTOMS
Thrombosis especially DVT is itself often quiet and diagnosed when tests are performed due to the presence of associated risk factors, or unfortunately when symptoms of pulmonary embolism occur.
The presenting signs and symptoms are usually due to thrombophlebitis. In the case of superficial veins, there may be redness, itchiness, burning pain, and tenderness along the affected vein with leg/arm swelling. Deep vein thrombophlebitis may also present with redness and pain, but often there are no symptoms, or sometimes only swelling in the affected limb is present. A low-grade fever may be present, which can become high grade if an infection sets in. The overlying skin may sometimes break down forming a venous ulcer.
Pulmonary embolism can present quite suddenly with shortness of breath, cough (sometimes with blood – hemoptysis), chest pain, wheezing, sweating, palpitation, and loss of consciousness. Around 5% of patients with DVT can develop pulmonary embolism which is one of the greatest emergencies in medicine. The fatality rate of acute PE when untreated is about 30% out of which 10% die suddenly. However, with high suspicion, timely diagnosis, and intervention, the death rate can be reduced by three-fourths.
MANAGEMENT
Prevention is the cornerstone of managing DVT. This is done by evaluating risk factors and assessing the actual risk of developing DVT. The risk factors are accorded points, and based on the number of points, the person may be assessed as having a mild, moderate, or high risk of DVT.
D-dimer (marker for thrombosis) levels in the blood can also help assess risk. It is important that while interpreting D-dimer levels in patients >50 years, the age-corrected cut-off (patient’s age in years × 10 ug/l) should be used.
In case of strong suspicion or presence of symptoms of thrombophlebitis like swelling, pain, and skin changes, imaging by a vascular duplex ultrasound is performed.
High-risk cases like those immobilized or hospitalized after major surgeries, fractures, trauma, or medical illnesses, are usually started on preventive doses of medicines called anticoagulants (blood thinners). Sometimes compression stockings also may be given to prevent stasis of blood flow in the veins.
The most important thing is to prevent the occurrence of pulmonary embolism and keep an astute alert for the same.
MEDICINES FOR THROMBOSIS
Anticoagulants (blood thinners or clot preventers)
These include injectable medicines used in the hospital setting like heparin and low molecular weight heparin (LMWH – enoxaparin and dalteparin) and fondaparinux.
Oral anticoagulants which can be used in the home setting or after discharge from the hospital include the conventional drug warfarin and the newer agents called directly-acting oral anticoagulants (DOACs – apixaban, dabigatran, rivaroxaban) also called novel oral anticoagulants (NOACs).
The most important side effect of anticoagulants is the risk of bleeding manifesting as blood in stools, urine, and small hemorrhages under the skin, or sometimes serious intracranial bleed. DOACs do not require constant monitoring of prothrombin time (PT-INR) like warfarin does, as their risk of causing bleeding is low. In addition, warfarin can interact with many food items and other drugs, which has to be discussed with the treating doctor. Anticoagulants are used for the prevention and treatment of DVT for up to 3 months or sometimes longer depending on thrombosis versus clotting risk and history of DVT or PE.
While the LMWH and DOACs act by inhibiting the action of factor X/II, warfarin acts by blocking vitamin K required for clotting. Anticoagulants prevent the formation of new clots and also prevent existing clots from getting bigger so that the body can more easily break them down. However, anticoagulants cannot break down a clot.
Anti-platelet drugs
These include drugs like aspirin, clopidogrel, and ticlopidine. These drugs are useful in cardiovascular disease (CVD) to prevent events like angina, heart attack, and stroke, as clots forming in arteries due to atherosclerosis are due to endothelial injury and are high in platelets.
However, these drugs have limited value in venous thrombosis. They may be used in low-risk cases and in patients with co-existing CVD.
Thrombolytics (clot busters or breakers)
These drugs are required in some cases of DVT with large clots and also for treating PE. These are given intravenously, and sometimes directly into the clot itself through a catheter inserted under imaging (duplex ultrasound) guidance. Such drugs act by breaking down fibrin and so are also called fibrinolytics. These include tissue plasminogen activators (t-PA – alteplase, reteplase, tenecteplase), anistreplase, streptokinase, and urokinase.
In addition to VTE, these drugs are also used to treat heart attack (myocardial infarction) or stroke caused by a clot blocking a coronary artery or cerebral artery respectively.
PROCEDURES AND SURGERY
By using the thin tube called the catheter inserted into the vein through a small incision, large clots can be removed (thrombectomy) or dissolved (thrombolysis). This is usually performed by a vascular surgeon in the operation theater under local anesthesia.
In some cases, vena cava filters are inserted into the abdomen to prevent pulmonary embolism.
Also read:
Post-COVID Cardiovascular Effects – Know the Symptoms and Causes
For any query, additional information or to discuss any case, leave a comment or write to info@drvarsha.com and be assured of a response soon.
Reference: CDC-VTE