WHAT IS IBD?
Inflammatory Bowel Disease (IBD) refers to a condition of chronic inflammation of the digestive tract (gut) especially the bowels. Inflammation is the body’s response to some form of injury or insult where the affected part of the body shows redness, swelling, impaired functioning and pain. In the short term, inflammation helps to get rid of the offending agent, but in the long term, chronic inflammation can cause ongoing damage to that part of the body. IBD is considered an autoimmune disease, and should not be confused with IBS (Irritable Bowel Syndrome) which is a different and benign clinical condition, sometimes with common or overlapping symptoms with IBD.
WHAT ARE THE TYPES OF IBD?
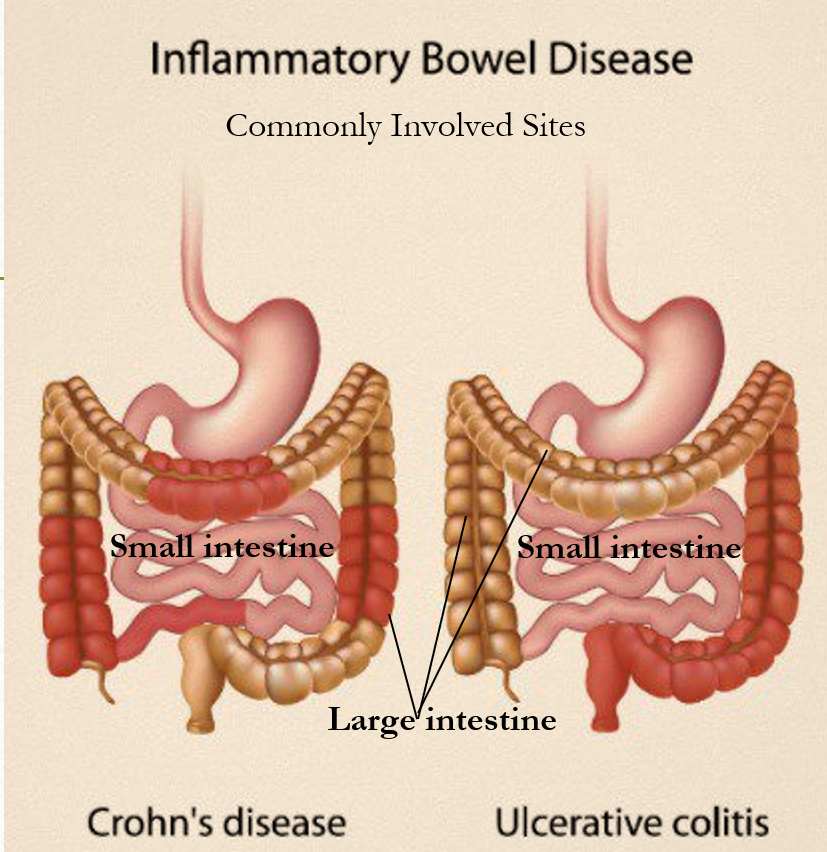
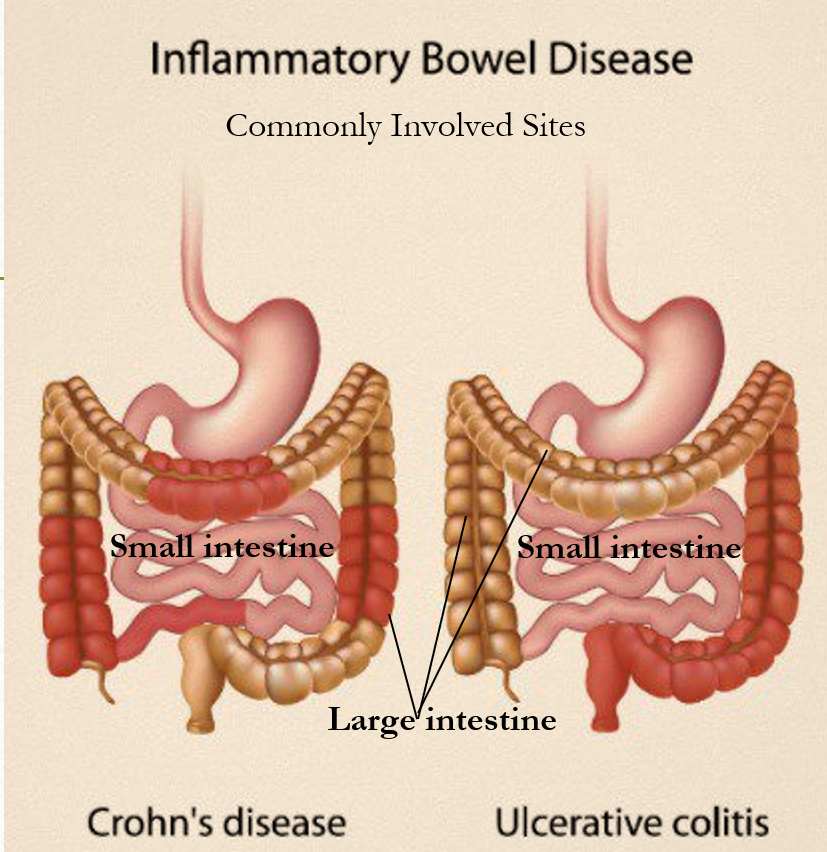
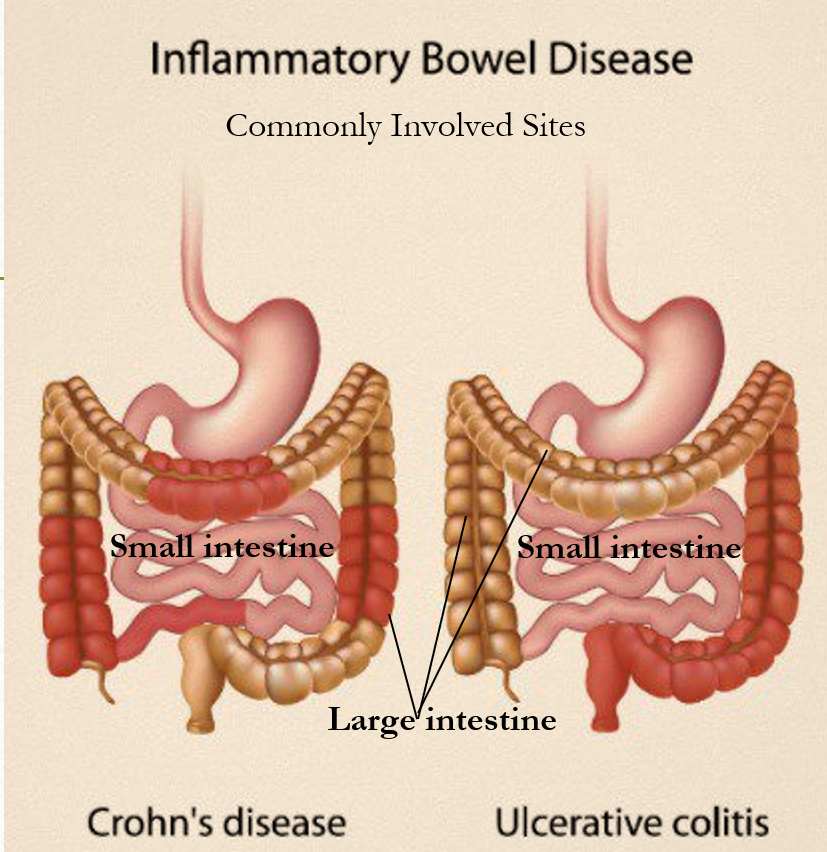
There are two types of IBD
- Crohn’s Disease (CD)
- Ulcerative Colitis (UC)
Crohn’s Disease can involve any part of the gut, but most commonly affects the junction of the small and large intestine, parts of the small intestine or large intestine or both simultaneously. It consists of discontinuous patches of inflammation usually affecting the entire thickness of the gut wall.
Ulcerative Colitis as the name suggests affects the Large Intestine (Colon) and Rectum, most commonly the latter part of the colon (descending colon) and rectum, and sometimes the entire colon (pan-colitis). The inflammation in UC is usually superficial and continuous.
WHAT ARE THE SYMPTOMS OF IBD?
Symptoms of IBD typically are crampy abdominal pain, persistent diarrhea, blood and mucus in the stools, change in appetite, weight loss, fatigue and sometimes fever. Nausea and vomiting may be seen in Crohn’s while urgency to pass stool and a feeling of incomplete evacuation are common in Ulcerative Colitis. The characteristic feature of IBD is that there are periods when the symptoms are prominent followed by symptom-free intervals (remission) which could be as long as even months or years.
Complications can arise as a consequence of progressive inflammation and damage like ulcers, tears (fissures), abnormal tunnels (fistulas), perforation of the bowel wall, bowel infections, scarring leading to bowel obstruction (strictures), massive bleeding (hemorrhage) and malnutrition. There is also an increased risk of developing cancers of the Colon in people with IBD (UC type).
WHAT IS THE CAUSE OF IBD?
The exact cause of IBD is often difficult to identify. It has been linked to an abnormal response of the immune system to environmental or dietary triggers, or to bacteria in the Gut, thereby producing chronic inflammation. Possible risk factors include genetic predisposition, family history of IBD, cigarette smoking, high stress, a diet high in fats or refined foods, and long-term use of pain medications of the NSAID group (like ibuprofen, naproxen, diclofenac etc.).
IBD is usually diagnosed in the third decade of life (30s). Sometimes IBD may be associated with other diseases due to an abnormal immune system response like inflammation of the joints (arthritis), bones, muscles, skin, eye, liver and bile duct system.
HOW IS IBD DIAGNOSED?
Blood tests are commonly ordered to check for anemia, infection, inflammation, nutritional deficiency and general health. These may include CBC, ESR, CRP, Blood sugar, Vitamin B12, Calcium, Iron studies, Liver and Kidney function, Proteins (albumin), and Electrolytes.
Stool test to check the presence of blood (both presence of Red Blood Cells and White Blood Cells) or pathogenic bacteria/parasites is also usually ordered. Sometimes specific markers may be tested for in the stool sample.
X-ray is performed for initial imaging and view of the digestive tract. In some cases, CT/MRI of the abdomen is required to look for complications like strictures, dilatations, perforations, fistulae, etc.
The most important and gold standard test is a Colonoscopy (Endoscopy of the lower digestive tract) performed by a Gastroenterologist whereby a slender tube with a light and camera is inserted through the anus to study the rectum, large intestine up to the last part of the small intestine. Colonoscopy helps not only to visualize and diagnose, but also perform small procedures and take a biopsy (a small piece from the gut wall to study under a microscope).
If the involvement of the upper part of the digestive tract is suspected in Crohn’s type of IBD, a test called EGD (Esophago-Gastro-Duodenoscopy) is performed where the lighted tube with a camera is inserted through the mouth to visualize food pipe (esophagus), stomach and the initial part of the small intestine. Enteroscopy is an endoscopic procedure done to visualize the small intestine. Now a technique called Capsule Endoscopy is available whereby the patient swallows a capsule with a multidirectional wireless camera, which records images of the digestive tract that are transmitted to a recorder worn on a belt around the waist. The capsule is eliminated in the stools naturally. This procedure is useful in Crohn’s disease to image the entire small intestine which is difficult by both Colonoscopy and Enteroscopy.
WHAT IS THE TREATMENT OF IBD?
The treatment approach to IBD includes Diet and Lifestyle modification, and appropriate drugs.
Diet and Lifestyle modification
People with IBD can often suffer from vitamin and mineral deficiencies and malnutrition resulting from a change in appetite, vomiting, diarrhea and decreased absorption of nutrients due to bowel inflammation. Therefore, eating a nutritious diet rich in vegetables, fruits, proteins, grains and yogurt with a good amount of daily water intake is advised. Eating frequent small meals instead of large meals at a time is recommended.
A personal record of daily diet to ascertain foods that trigger symptoms helps in avoiding such items in the diet. Sources of Omega 3 fats like fish, fish oils, canola oil, walnuts, flaxseeds) as well as substances that reduce inflammation like turmeric, ginger and garlic can be included in the diet. General avoidance of deep-fried, processed, fast, packaged and refined foods routinely is advised. Reducing the intake of caffeine and alcohol is also advised.
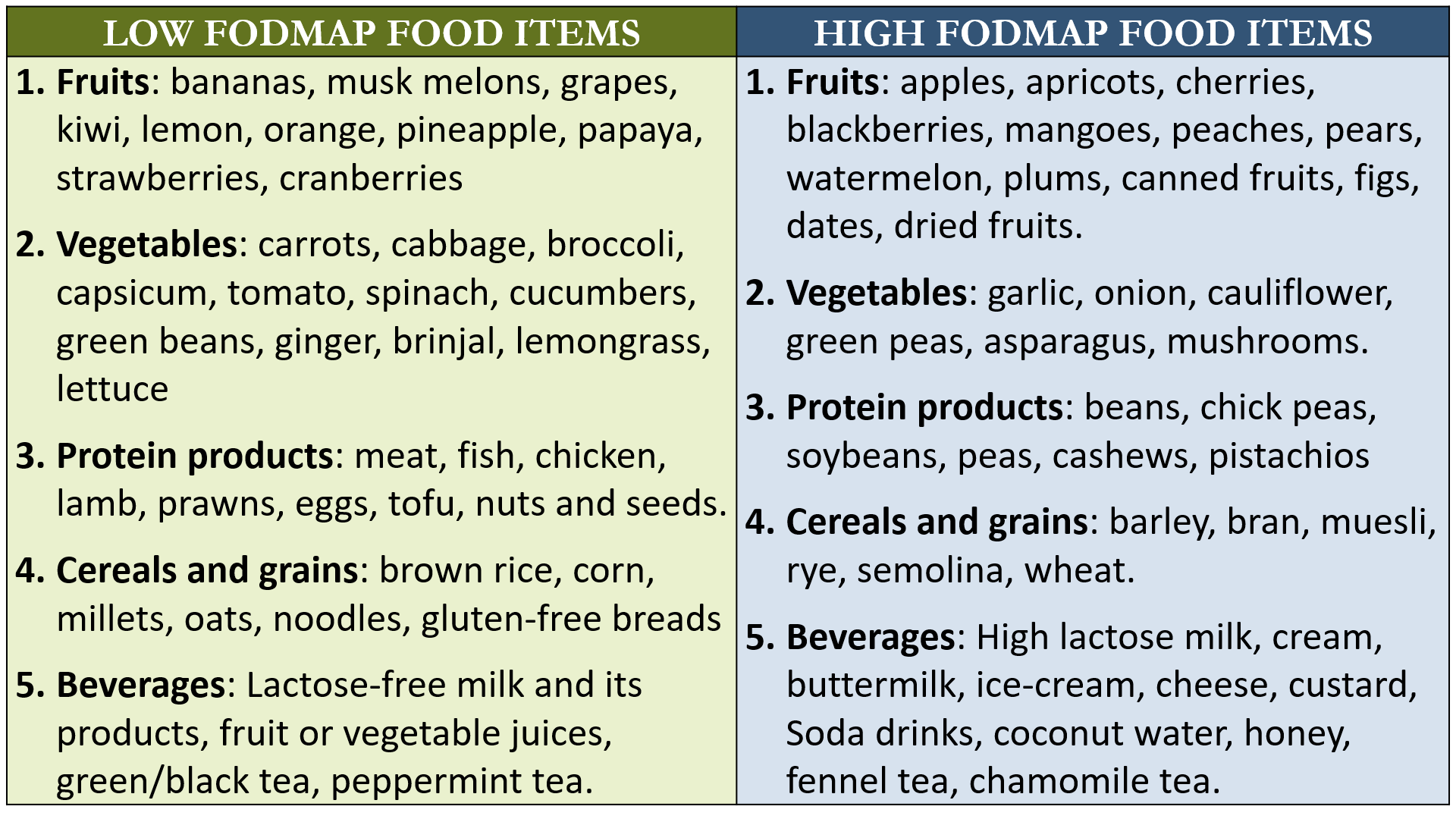
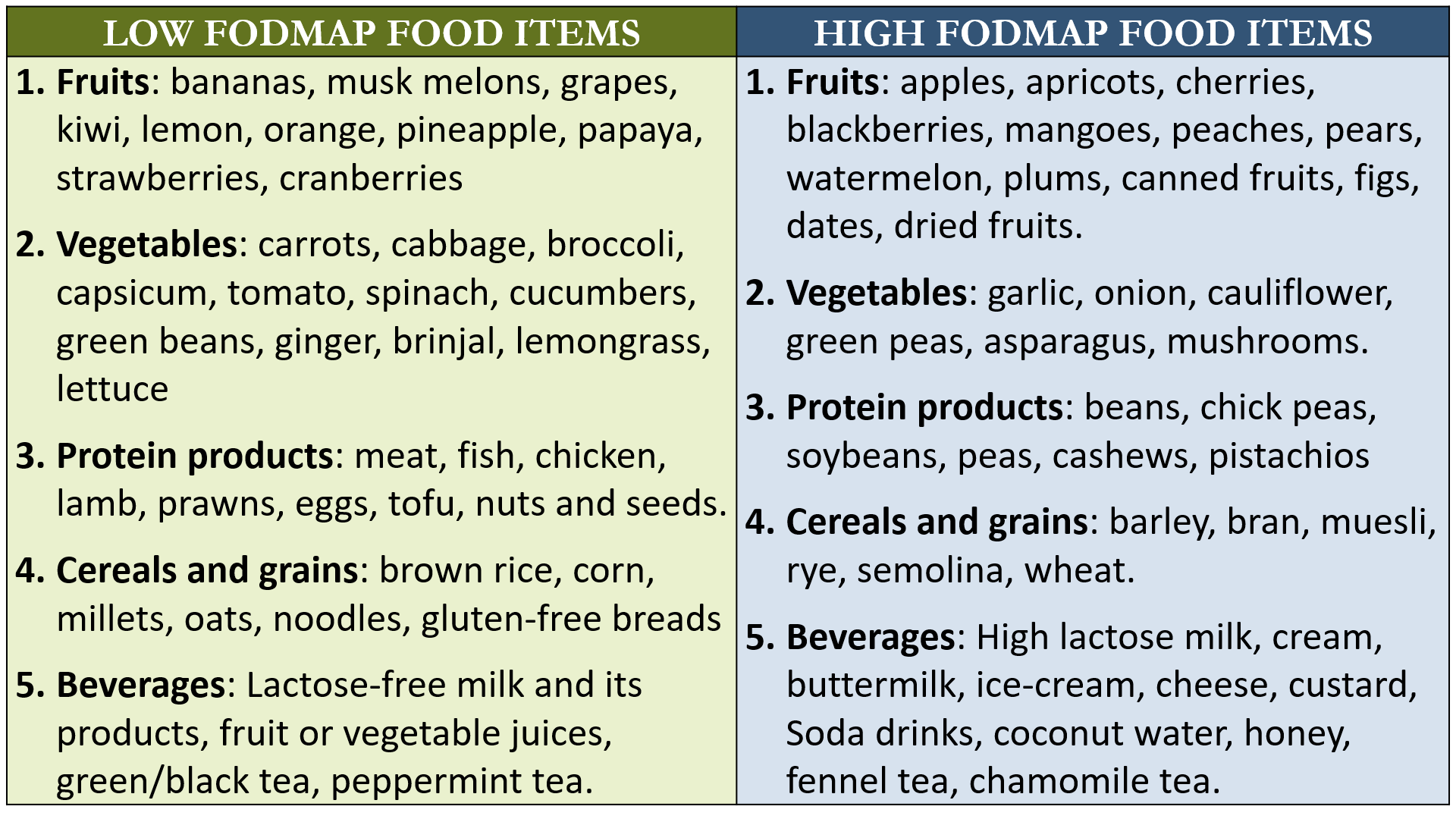
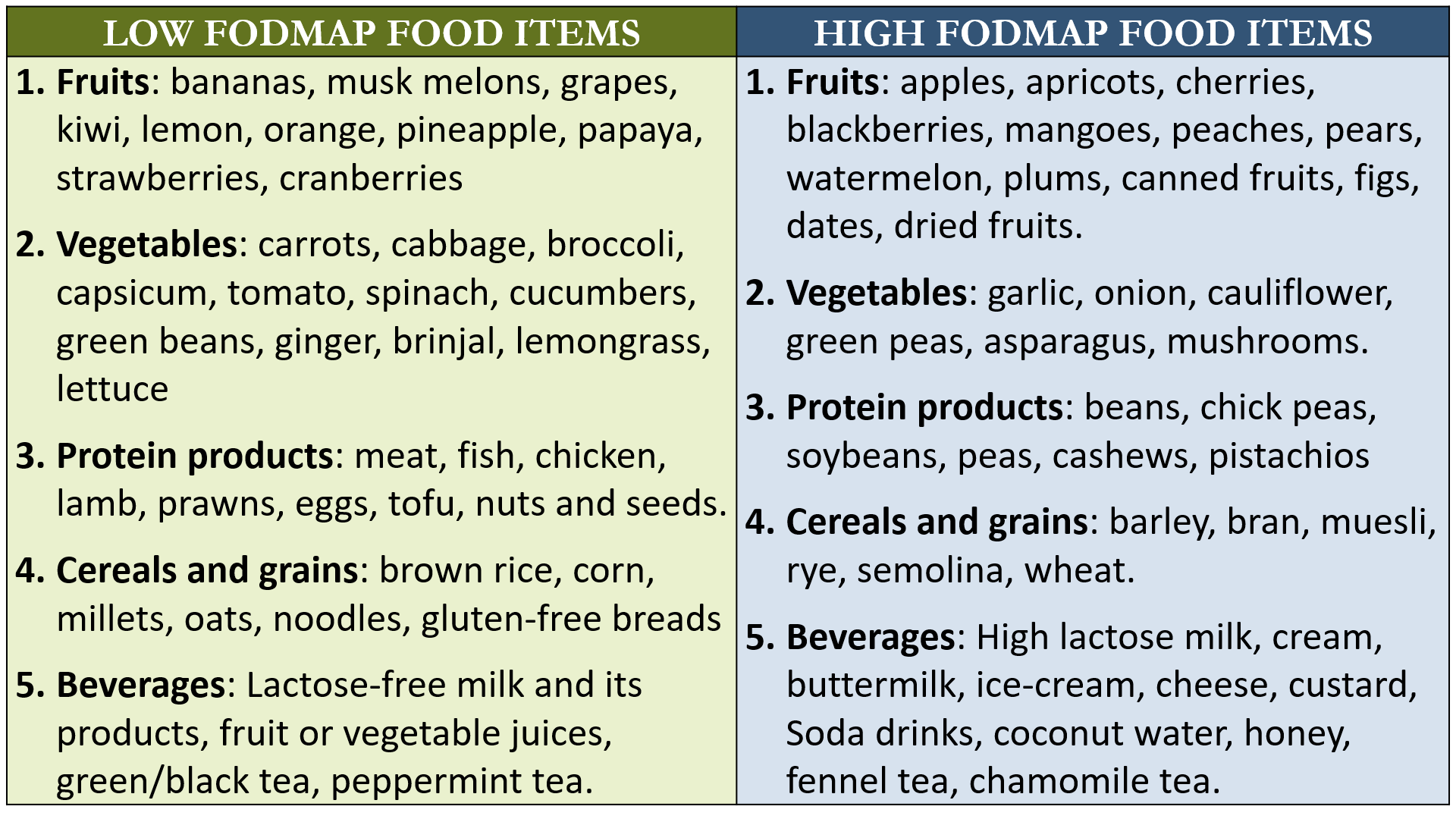
Patients who have significant and ongoing diarrhea, bloating or gas symptoms, may benefit from a Low FODMAP diet. This diet is routinely recommended in patients with IBS, and is also sometimes tried in IBD patients who have such persistent symptoms.
Nutritional supplements may be required if tests show deficiency, like calcium, iron, Vitamin D and Vitamin B12/B complex supplements. Substituting good Gut bacteria (Probiotic supplements) are also commonly given to IBD patients.
Regular physical exercise and adequate rest (at least 8 hours sleep at night), along with stress management (through Yoga, breathing exercises and relaxation activities) are recommended and beneficial and recommended.
Drug therapy
The medicines used in treatment depend on the severity and responsiveness of the disease. These drugs act by controlling and suppressing inflammation and modifying the abnormal response of the immune system. Some of these medicines like Mesalamine and Sulfasalazine (Aminosalicylate drugs) or Budesonide and Hydrocortisone (Corticosteroids drugs) can be given by both Topical (through rectal route as an enema, suppository or foam), or by the oral route. Antibiotics are also prescribed to control bowel infection and overgrowth of harmful bacteria which may be responsible for triggering the inflammation. Immunomodulator drugs used in more severe cases include Methotrexate, Cyclosporine and Azathioprine. The latest group of drugs which are biological antibodies against specific inflammatory mediators include the anti TNF-A Biologics Infliximab and Adalimumab which are given by injectable route.
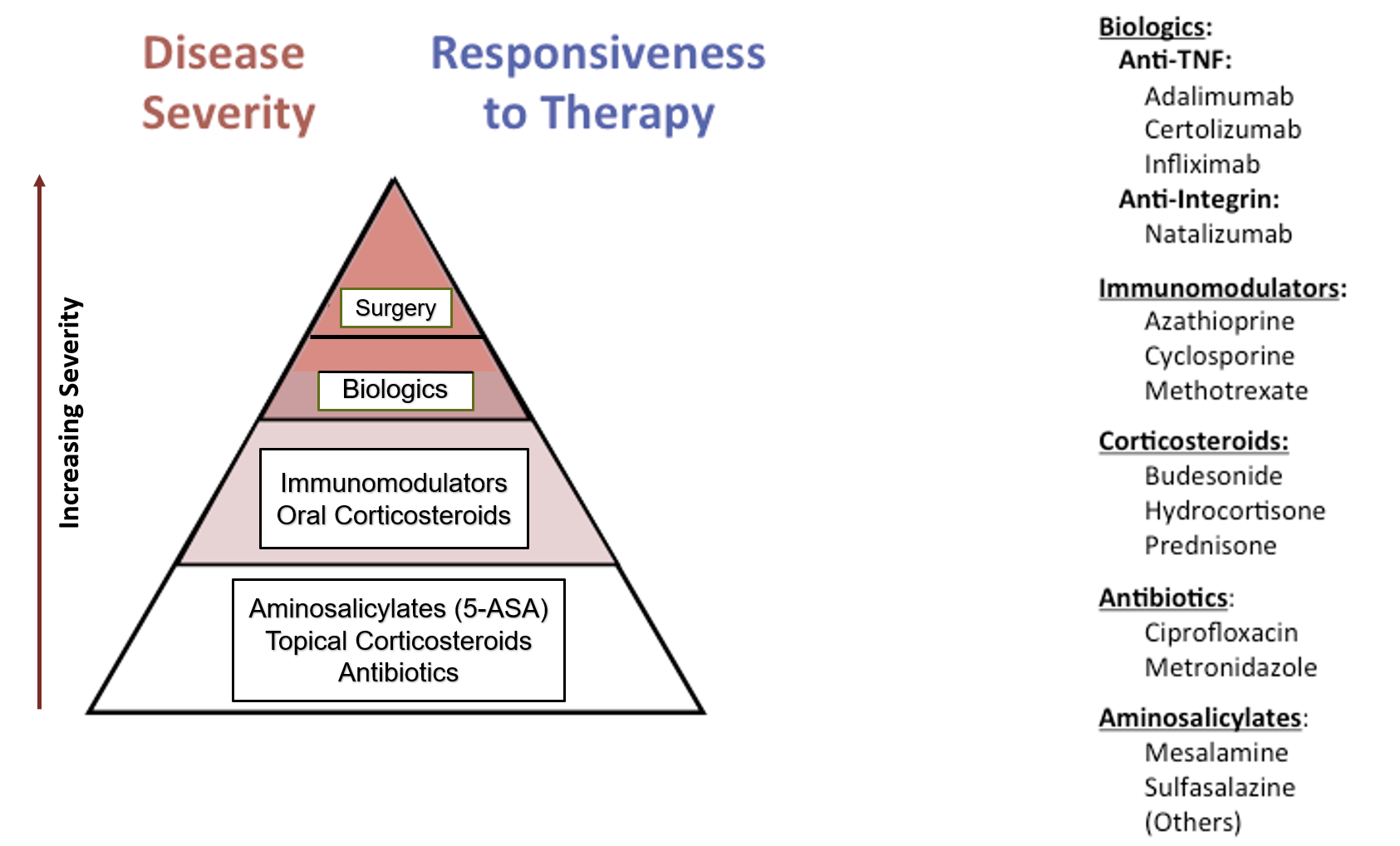
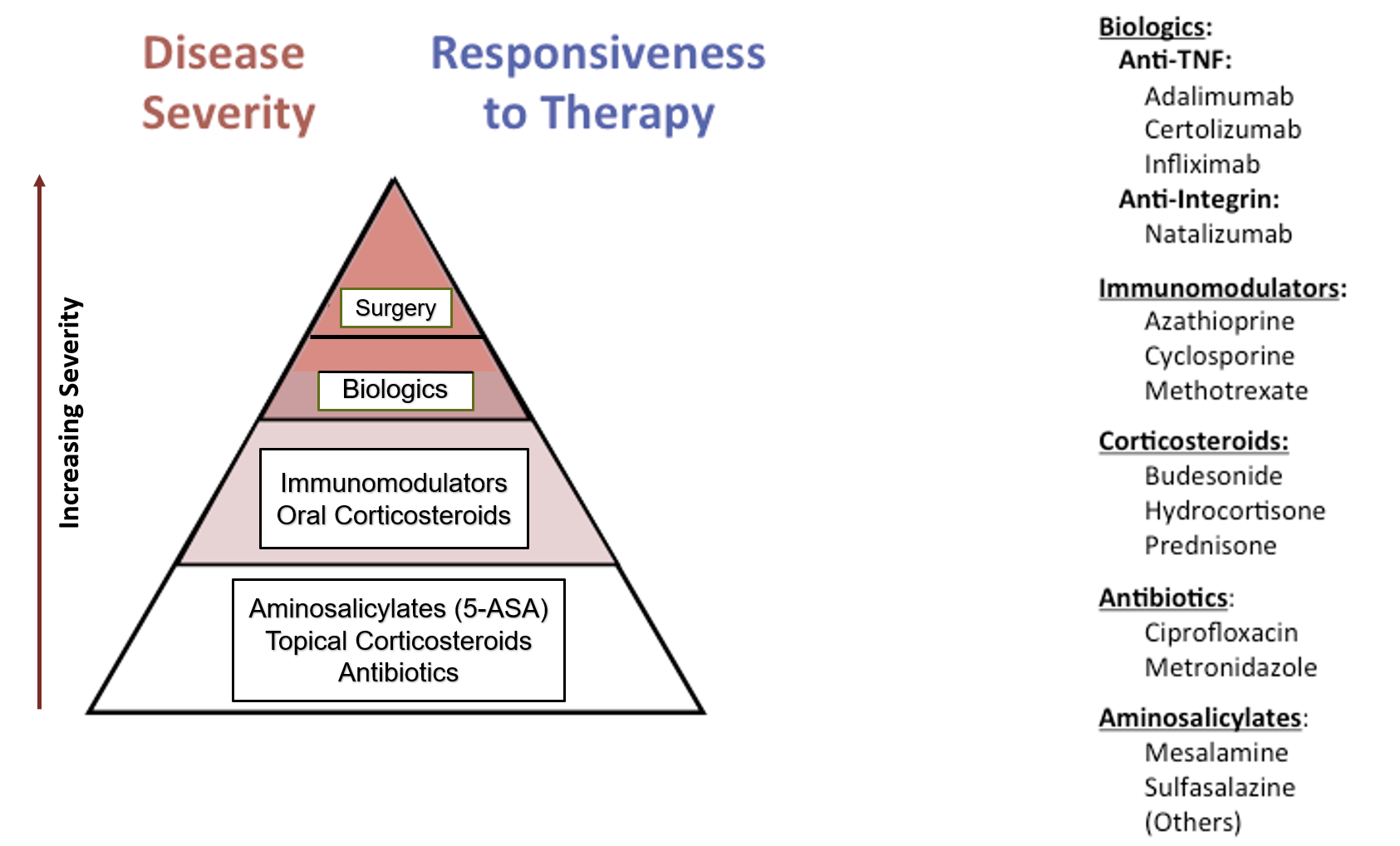
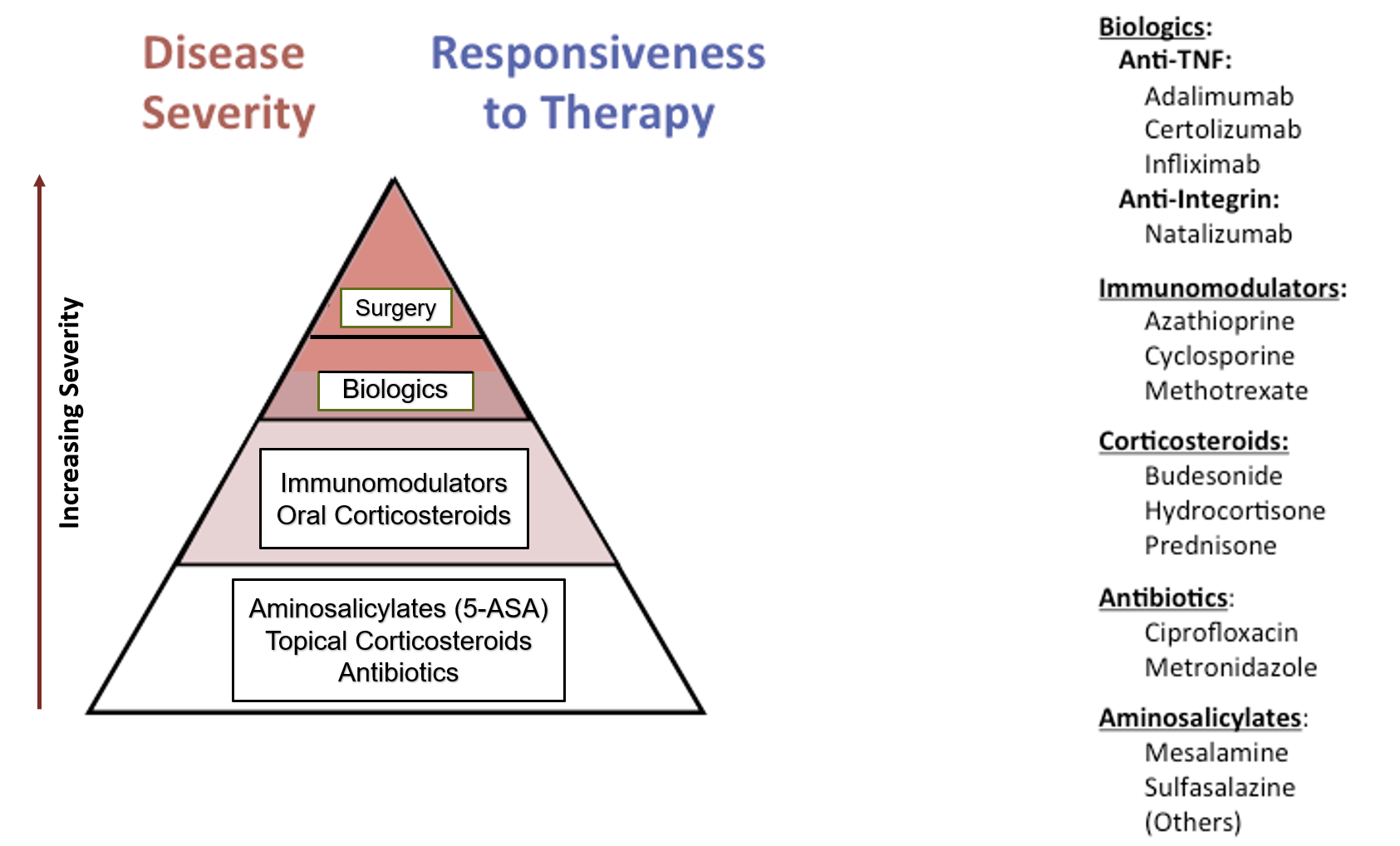
Surgery is required to manage bowel obstructions (strictures), to remove a section of severely damaged bowel, or to treat fistulas.
Screening for Colon cancer is advised periodically in patients suffering from IBD (especially UC type).
Dr Subhash Agal is currently heading the Department of Gastroenterology and Human Nutrition at Kokilaben Dhirubhai Ambani Hospital, Mumbai. He has done his DNB (Gastro) under the able guidance of Late Dr H G Desai who was a doyen in the field of Gastroenterology. Subsequently he acquired endoscopy skills from the best in the field. He has been practicing gastroenterology for more than 29 years and his clinical acumen is well known by the doctors’ peer group. He figured in the list of 10 best gastroenterologists in Mumbai in the year 2009 as per an independent peer journal survey..
Also read-