Tuberculosis (TB) is an infection caused by a bacterium called Mycobacterium tuberculosis. This bacterium usually attacks the lungs (pulmonary TB) and this is the most common type of TB. However, the TB bacteria can also spread via blood and attack any part of the body (extrapulmonary TB) like bones, spine, brain, lymph nodes, intestines, kidneys, and skin.
Some people infected with TB do not display symptoms or suffer from illness (latent TB infection), while those suffering symptoms are said to have TB disease. Timely diagnosis and treatment of TB are very important, otherwise, fatality can be high.
TB is more common in developing countries, however, in developed countries, there is more incidence of TB with HIV. Lowered immunity increases the rate of getting infected from and suffering from pulmonary TB, as well as developing extrapulmonary TB. People with HIV can also get infected with atypical Mycobacteria (M. avium and intracellulare -MAI or M. avium complex -MAC), that are not strong enough to cause TB in people with normal immunity (atypical TB).
According to the WHO Global TB report 2020, the annual incidence of TB globally is 10 million (with half a million being multi-drug resistant MDR cases) and a mortality of 1.2 million. India contributes 26% of the global TB load and 36% of mortality due to TB. The incidence of TB in patients with HIV is 0.8 million, with around 8% coming from India.
TRANSMISSION
TB bacteria are spread through the air by droplets from one person to another during sneezing, coughing, talking, etc. The risk of spread is higher in crowded and poorly ventilated areas or housing, and also for health workers treating TB cases. TB does not spread by touch, food/water, or material contact. TB bacteria enter the lungs and then depending on the body’s immune response, can also spread to extrapulmonary sites.
People with pulmonary TB are infectious especially to their family members and household contacts, however, if treatment is initiated the person becomes non-infectious in 2 weeks. People with latent TB or extrapulmonary TB are usually not infectious.
STAGES OF TB INFECTION
Primary infection
It refers to the first 2-3 weeks after the TB bacteria enter the lung, multiply, and stimulate the immune system resulting in local inflammation. The person is asymptomatic at this time.
Latent infection
This occurs after the primary infection stage of 3 weeks, as in >90% of cases the immune system suppresses the bacterial replication before symptoms develop. However, the TB bacteria can remain dormant and survive for a long time or many years in the lung inside ‘granulomas’ that are a focal collection of different tissue and immune cells, with cheesy necrotic centers (cavities). These foci may be visible as nodular scars on a chest X-ray (Ghon foci). At this stage the tuberculin skin test and interferon-gamma release blood assays (IGRA) become positive.
The duration of the latent infection depends on the virulence of the bacteria and the immunity of the host. In people with low immunity (children/elderly) or those who are immunocompromised (people taking corticosteroids or immunosuppressants, having illnesses like HIV, diabetes, or cancer, those undergoing surgeries or dialysis, tobacco users/smokers, or suffering intense stress), the risk to progression to active disease is much higher, and the latent period is short. At this stage, the bacteria can also spread to the blood and other organs, therefore extrapulmonary TB can manifest without symptoms of lung disease.
Active disease
This is the stage of symptoms and organ damage. Around 5-10% of healthy people infected with TB bacteria progress from the stage of latent infection to active disease, usually within 2 years, or the reactivation of infection may sometimes occur years or even decades later. Active disease can also occur due to reinfection with the TB bacteria rather than reactivation.
TB damages the affected organs by forming granulomas that destroy the tissues and cause inflammation, fibrosis (scarring), and strictures (narrowing). The lungs show typical lesions with cavities and may be associated with swelling and fluid/pus (pleural effusion and empyema). Damage of the lungs reduces expansion of the lung, gaseous exchange, and oxygen in the blood. If left untreated, lung damage can lead eventually to death.
SYMPTOMS
For pulmonary TB, the following is the criteria for symptomatic suspicion of TB:
- Cough for 2 weeks or more not responding to antibiotics.
- Cough of any duration if the person has been in contact with a confirmed TB case, is already diagnosed with extrapulmonary TB, is HIV positive, immunocompromised, diabetic, has renal failure, cancer, malnutrition, and in case of elderly, children, and pregnant women.
- Cough may initially have minimum sputum (yellow/green) that may progressively increase. Later coughing up blood may also be seen, along with chest pain and breathlessness.
Symptoms and signs common to both pulmonary and extrapulmonary TB include:
- Weight loss
- Loss of appetite
- Night sweats or chills
- Evening low-grade fever
- Weakness or fatigue
- Enlarged lymph nodes
In addition, in extrapulmonary TB, there will be symptoms related to the part affected like unexplained pain, swelling or abnormal functioning.
DIAGNOSIS OF PULMONARY TB
Screening Tests
This is done to rule out TB and for contact investigation:
- Tuberculin skin test (TST) – A skin test that involves injecting a purified protein derivative (PPD) into the skin and examination 48 to 72 hours after the injection for measuring the induration (palpable inflammatory skin thickening).
- Interferon-gamma release blood assays (IGRA) – A blood test that involves a single lab visit and results within 24 hours. The T-SPOT.TB is an IGRA test to detect TB in patients aged 2 years or older.
- Chest X-ray
Diagnostic tests
These are done when symptomatic suspicion or signs are present, there is a history of household contact or institutional exposure, and if the screening test is positive.
- Sputum: Staining-Microscopy, and Culture for TB bacteria
- Nucleic acid–amplification test (NAAT)
- Chest X-ray
Once TB is diagnosed, patients should be tested for HIV infection, and those with risk factors for hepatitis B or C should be tested for those viruses. Baseline tests of hepatic and renal function should typically be done.
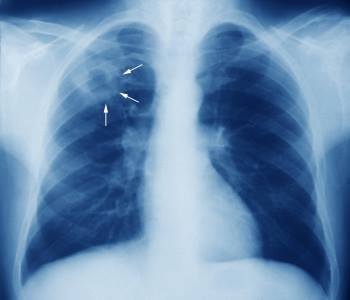
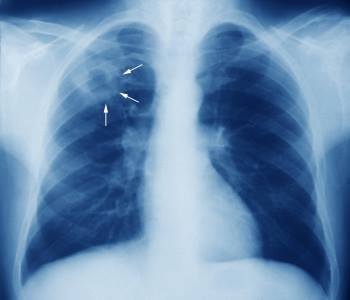
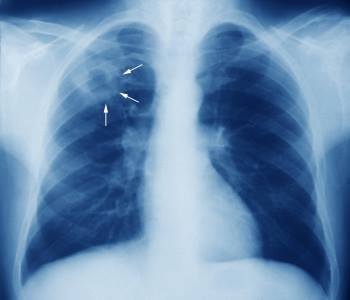
Chest X-ray
Chest X-ray is used as both a screening test and a diagnostic test to see lung involvement in TB. The characteristic signs include the typical upper nodular cavity (as shown), the suspicious but non-specific middle and lower lesions, or calcified nodes.
Sputum Smear Microscopic Examination
Sputum testing is the most important diagnostic test for the diagnosis of pulmonary tuberculosis. Sputum is obtained by spontaneous coughing up, or by hypertonic saline induction or bronchoscopy when needed. The person conducting the sputum sample collection should be well protected with an N95 mask).
TB bacteria take up the Ziehl–Neelsen stain and appear bright red against a blue background, under the microscope. They are thus called acid-fast bacilli (AFB), and this is due to a substance called mycolic acid in their cell wall. Although the presence of AFB in a sputum smear is highly diagnostic of TB, definitive diagnosis requires a positive culture or nucleic acid amplification test (NAAT).
Culture
Culture can detect as few as 10 bacilli/mL of sputum and can be done using solid (egg-based LJ media) or liquid media (BACTEC MGIT 960). It can take up to 3 months for final confirmation of culture results, however, liquid media are more sensitive and faster than solid media, with results available in 2 to 3 weeks.
Rapid antigen testing to detect the MPB64 antigen of TB bacteria can confirm that organisms growing on culture are M. tuberculosis. Culture is also needed to isolate bacteria for drug-susceptibility testing and genotyping.
NAAT
These are rapid diagnostic molecular tests. Two types of NAAT are available for TB diagnosis: Xpert MTB/RIF and LPA.
Xpert MTB/RIF (GeneXpert MTB/RIF) is an automated rapid cartridge-based NAAT (CBNAAT) that identifies M tuberculosis DNA in a sputum sample as well as detects resistance to rifampicin. It takes around 2 hours and is more sensitive than sputum smear microscopy and as sensitive as culture, for diagnosing TB. If the Xpert MTB/RIF test on a sputum sample is positive, the diagnosis of pulmonary TB is considered confirmed. In such cases, treatment can be started based on rifampicin susceptibility.
Line probe assay (LPA) can identify the presence of M. tuberculosis and resistance to rifampin and isoniazid (first-line FL-LPA), along with fluoroquinolones and the second-line injectable drugs (second-line SL-LPA). It is less sensitive than GeneXpert MTB/RIF and is therefore done for smear-positive specimens.
If NAAT is negative with AFB smear results positive, clinical judgment has to be used to decide starting of treatment, while culture is awaited.
Drug Susceptibility Tests
Drug susceptibility tests (DSTs) should be done on initial sputum samples and also repeated if patients continue to produce culture-positive sputum after 3 months of treatment or if cultures become positive again after a period of being negative.
Results of DSTs with conventional bacteriological methods may take up to 8 weeks, but new molecular DSTs with CBNAAT and LPA can detect drug resistance within a few hours. If drug resistance to rifampicin is seen, further first and second-line LPA (FL-LPA and SL-LPA) are done. Thereafter, additional liquid culture drug sensitivity tests (LC-DST) are performed to evaluate resistance to other drugs including newer TB drugs used for drug-resistant TB.
Drug-resistant TB is called Multidrug-resistant TB (MDR TB) if the tuberculosis bacteria are resistant to at least isoniazid and rifampicin, the two most potent TB drugs. Extensively drug-resistant TB (XDR TB), though rarer, is the resistance of the tuberculosis bacteria to isoniazid and rifampin, plus any fluoroquinolone (FQ) antibiotic (ofloxacin, levofloxacin, moxifloxacin) and at least 1 of the 3 injectable second-line antibiotics- amikacin, kanamycin, or capreomycin.
Now genotyping and DNA sequencing are available for evaluating MDR-TB. Deeplex Myc-TB is an all-in-one test for species-level identification, genotyping and prediction of antibiotic resistance in Mycobacterium tuberculosis bacterial strains. As the first ever tool to exploit in-depth DNA sequencing technology and thus detect and analyze antibiotic resistance, Deeplex Myc-TB detects mutations responsible for antituberculosis drug resistance.
Tuberculin Skin Test (TST)
The TST (Mantoux or PPD purified protein derivative test) is positive in latent and active infection and cannot differentiate between the two. It is a screening test for TB exposure and infection. The standard dose of 5 tuberculin units (TU) of PPD in 0.1 mL of solution is injected on the palm side (volar) forearm intradermally. A well-demarcated bleb or wheal should result immediately. The diameter of induration (hardness, not redness) is measured 48 to 72 hours after injection.
The cut-off for a positive test depends on patient factors:
- 5mm for high-risk cases: immunocompromised (HIV, use of corticosteroids or immunosuppressants), X-ray evidence of past TB, or household contacts.
- 10 mm for medium risk: Patients with certain conditions (silicosis, renal insufficiency, diabetes, head-neck cancer, undergone gastrectomy or jejunoileal bypass surgery), injection drug users, recent immigrants from high-prevalence areas, and residents of prisons or homeless shelters.
- 15 mm for no risk: Patients not requiring testing except as screening requirements for starting medicines, or other reasons.



False-negative results may be seen in fever, the elderly, HIV (CD4 < 200 cells/μL), or very ill and showing no reaction to any skin test (anergy).
False-positive results may occur if patients have nontuberculous mycobacterial infections or have received the BCG vaccine. However, the effect of BCG vaccination on TST wanes after several years, after which a positive test is likely to be due to TB infection.
Interferon-gamma release blood assays (IGRA)
This is a blood test based on the release of interferon-gamma (an inflammatory cytokine) by lymphocytes exposed to TB-specific antigens. It is as sensitive as and more specific than TST in contact testing and screening, and is not false positive due to TB in the remote past or BCG vaccination. However, it is limited by its high price.
Other baseline investigations
These include complete blood counts (CBC), sugar, kidney and liver function, blood proteins, thyroid tests, serum electrolytes, and inflammatory markers like ESR and CRP. HIV, and Hepatitis B, C are also tested for. A baseline eye examination is also recommended.
TREATMENT OF PULMONARY TB
Patients diagnosed with TB can be classified for treatment as follows:
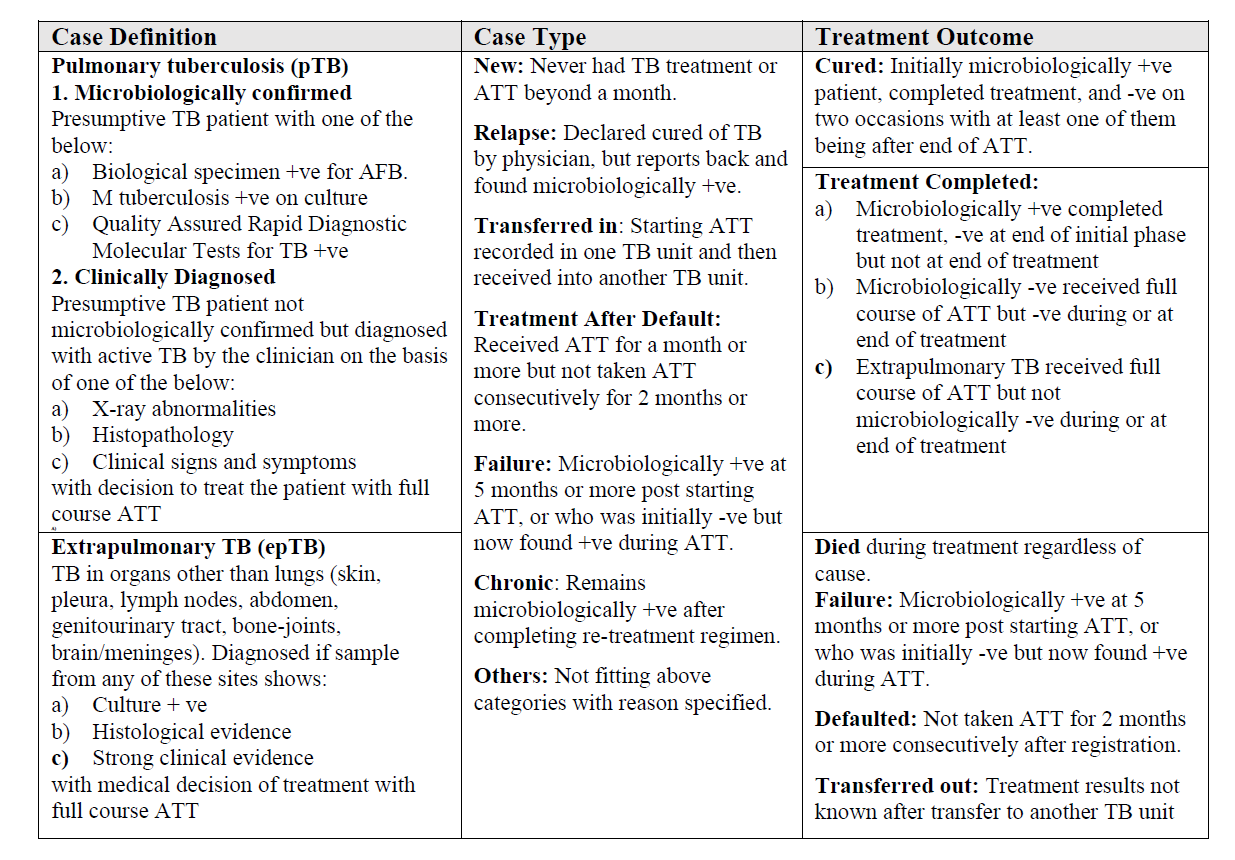
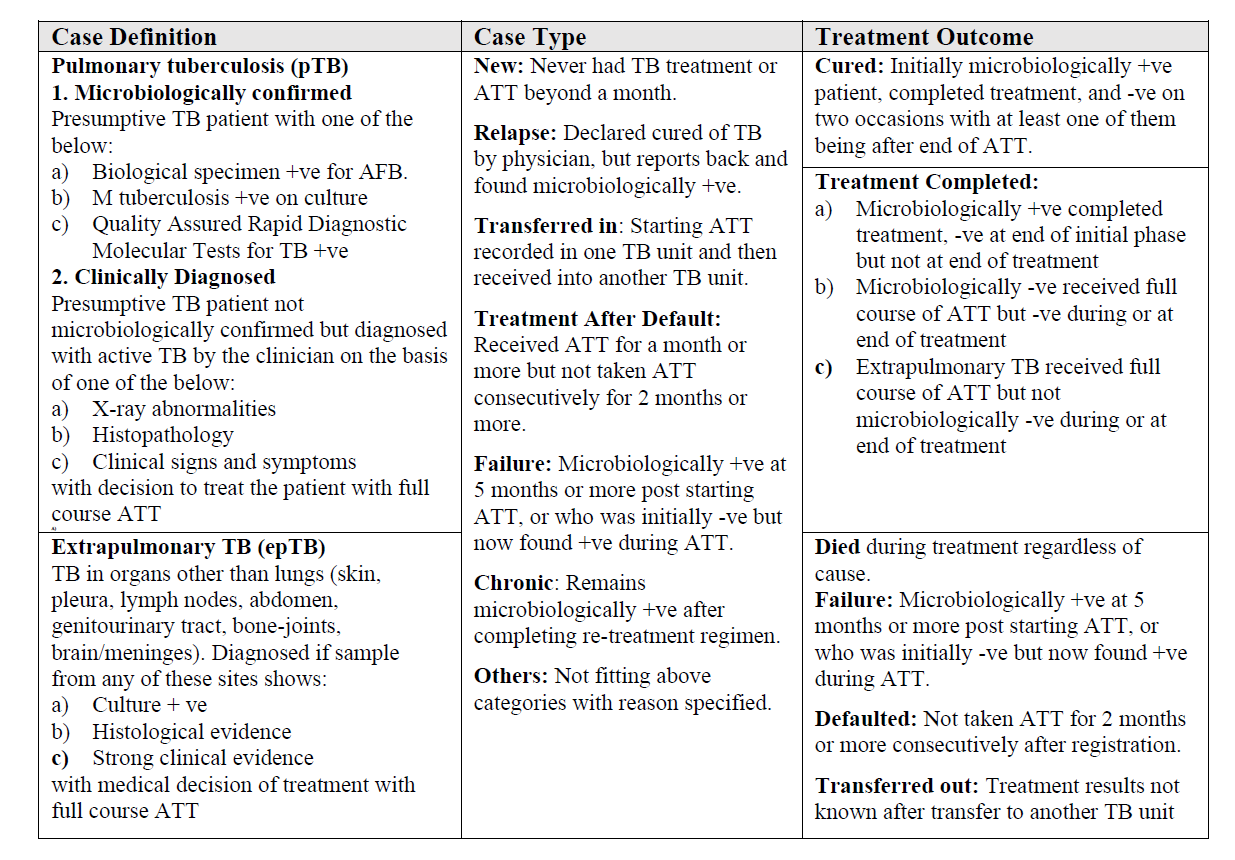
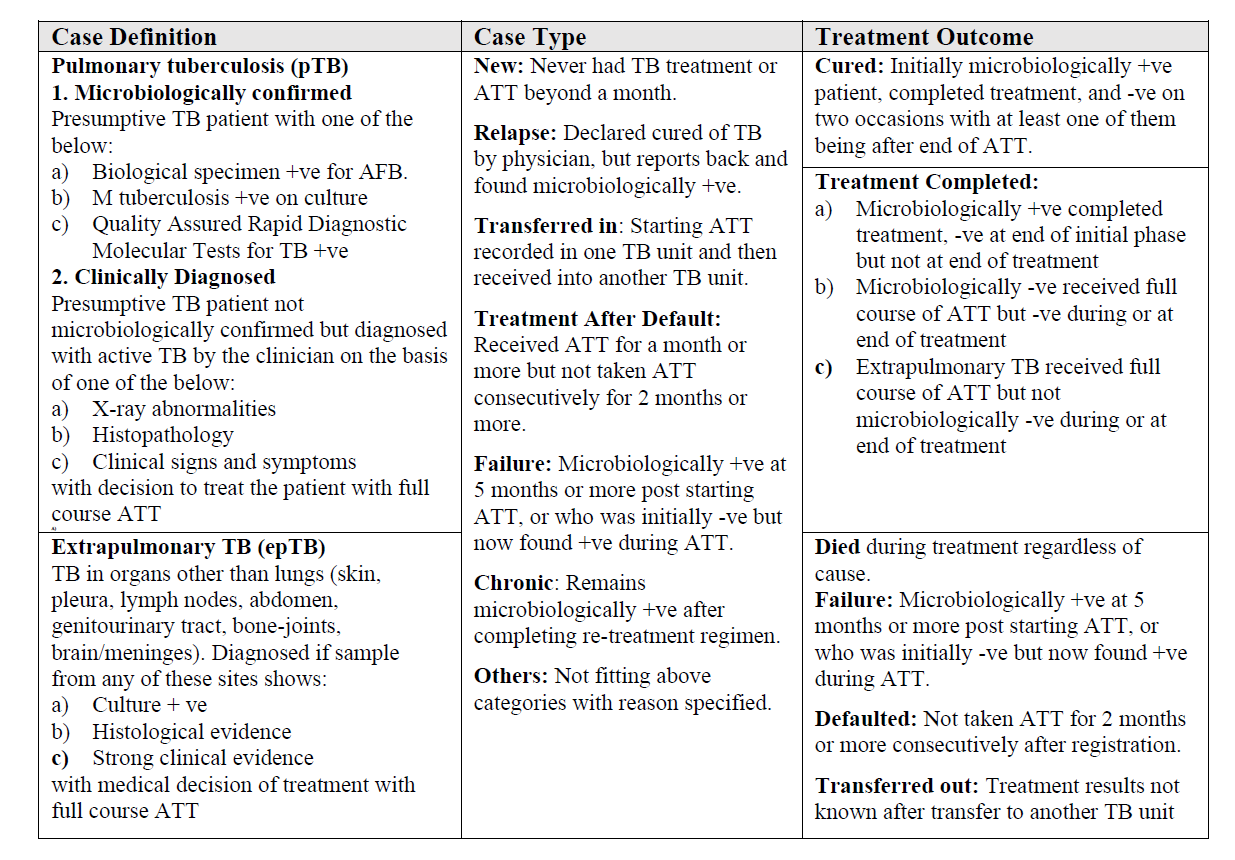
TB is a notifiable disease, and all doctors treating any TB case are required to notify the authorities under the national TB programs. The Revised National Tuberculosis Program (RNTCP -India) launched in 1997, was renamed in 2020 as the National Tuberculosis Elimination Program (NTEP) to emphasize the aim of the Government of India to eliminate TB. The TB drugs under RNTCP/NTEP are supplied in an individual patient-wise box that contains the entire course of treatment for the patient. In each box, there are two pouches for IP and CP. The boxes are color-coded with red for new patients and blue for previously treated patients.
New Cases
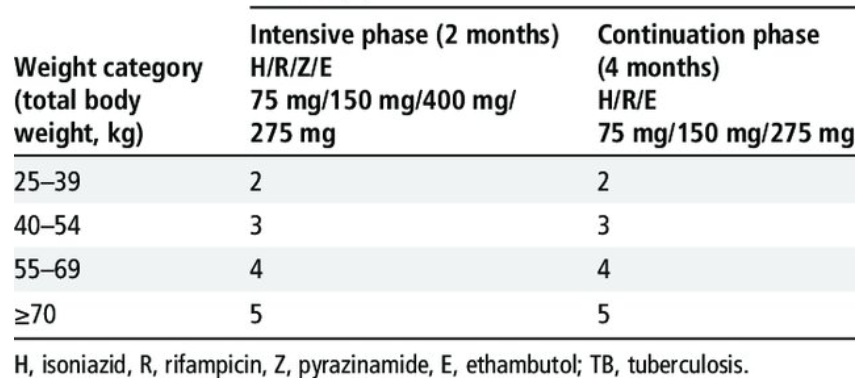
All new TB patients in India should receive an internationally accepted first-line regimen of anti-tubercular treatment (ATT). Group 1 drugs for tuberculosis (TB) are the first-line oral antibiotics: isoniazid, rifampicin, pyrazinamide, and ethambutol. These are the most potent and best-tolerated drugs, typically used for drug-susceptible TB and new cases.
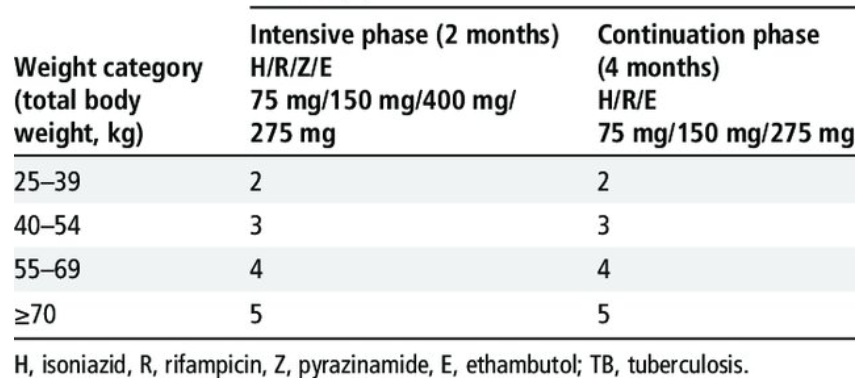
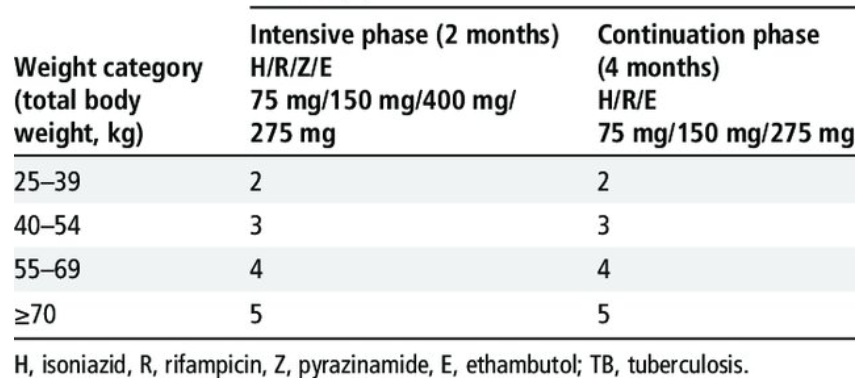
2HREZ/4HRE. The initial intensive phase consists of 8 weeks (2 months) of 4 drugs- isoniazid (H), rifampicin (R), pyrazinamide (Z), and ethambutol (E). The continuation phase should consist of the 3 drugs isoniazid, rifampicin, and ethambutol given for at least another 16 weeks (minimum 4 months). The drug dosages are given according to body weight (there are 4 weight band dosage categories). There are also fixed-dose combinations available of HR, HRE, and HREZ) for convenience and reduced pill burden.
DOTS (Directly Observed Therapy Short Term) is the method followed for administering the treatment under the RNTCP-India, where the patient takes the daily TB medication in front of a DOTS agent, who is a community volunteer or family member. Each patient gets a month’s supply of drugs and is supervised when taking the drugs using the DOTS strategy. Monthly food and nutritional support are also given to underprivileged TB patients.
Examination of a sputum smear at the end of the 2-month initial phase of treatment is done. If the smear is positive, the initial phase may be continued for another 1 month before proceeding with the 4-6 months continuation phase. Follow-up smear examinations are also done during and at the end of the continuation phase.
Multi-Drug Resistant TB (MDR-TB)
MDR-TB – resistant to isoniazid (H) and rifampicin (R), and RR-TB resistant to rifampicin, and a surrogate marker of MDR-TB) are major issues to be tackled. Isoniazid-resistant TB (Hr-TB) refers to Mycobacterium tuberculosis strains in which resistance to isoniazid and susceptibility to rifampicin has been confirmed in vitro (KatG is a catalase-peroxidase enzyme in Mycobacterium tuberculosis that plays a crucial role in activating isoniazid and is a major cause of resistance when mutated, while the InhA mutation is associated with low-level resistance to isoniazid and can also confer resistance to ethionamide, a structural analog of isoniazid).
The stress is now on NAAT (Nucleic Acid Amplification Tests) to provide rapid and accurate diagnosis of tuberculosis and drug resistance, enabling timely treatment initiation and improved patient outcomes. and using newer MDR drugs, such as bedaquiline (BDQ) and delaminid (DLM), in the DOTS-Plus regimen, reducing the use of injectables. Other drugs like fluoroquinolones (FQ – Lfx, Mfx) and other antibiotics have also been used and categorized, and regimens have been recommended based on the availability and resistance of these individual drugs. Patients with MDR-TB can show additional resistance to fluoroquinolones (Pre-XDR TB).
The emphasis now is on Universal Drug Sensitivity Testing (DST) or liquid culture DST (LC-DST) in Culture and Drug Susceptibility Testing laboratories (C&DST) to treat each individual patient as per his/her requirement. CBNAAT/GeneXpert (Cartridge-Based Nucleic Acid Amplification Test), FL-LPA, SL-LPA (First/Second-line Line Probe Assay) are the pillars in the current TB strategy.
Regimens with a BDQ and DLM combination have shown good culture conversion and safety after 6 months of treatment. The WHO has regrouped anti-TB drugs and recommended including drugs from both groups A and B to have at least 4 effective medicines in a regimen.
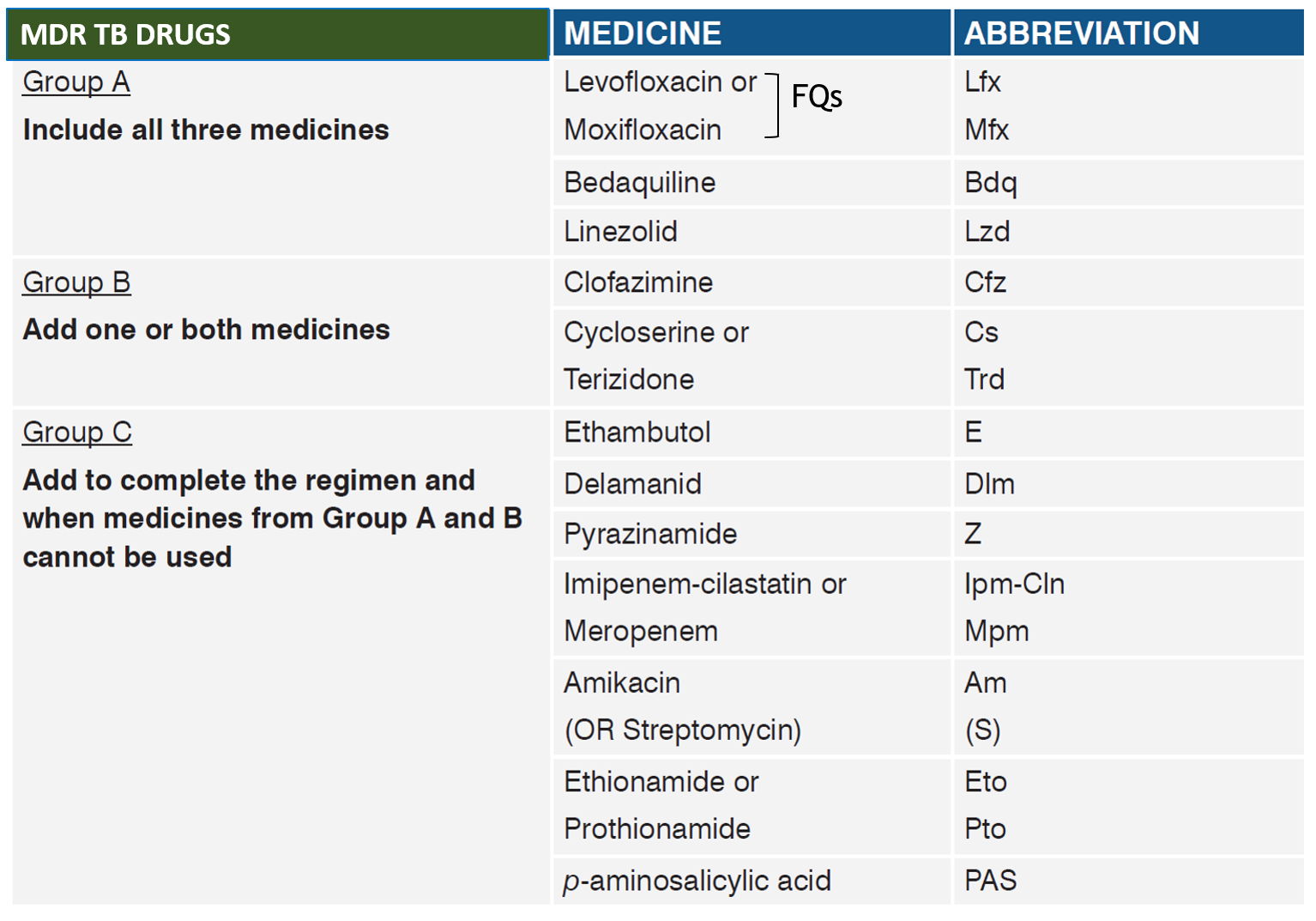
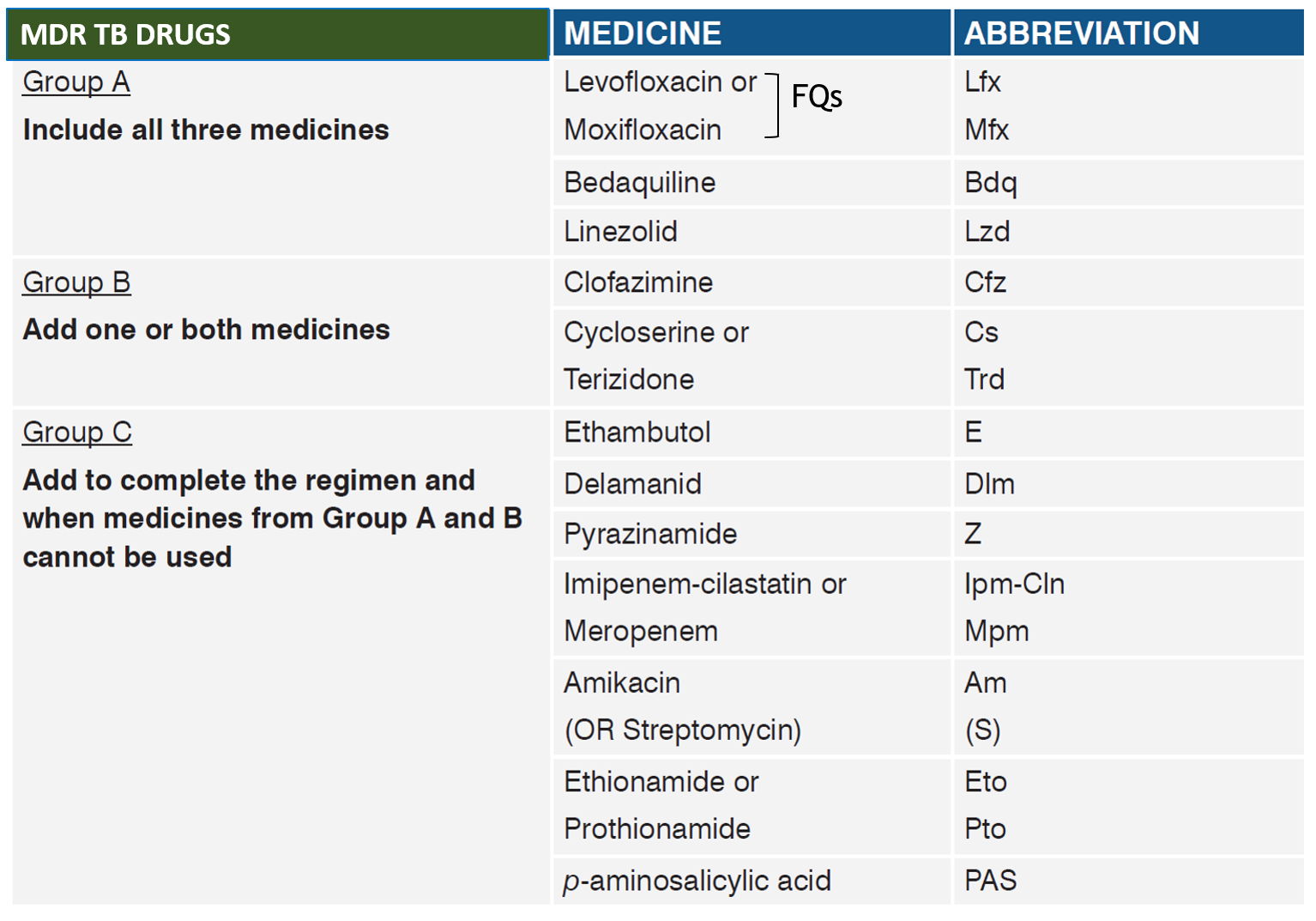
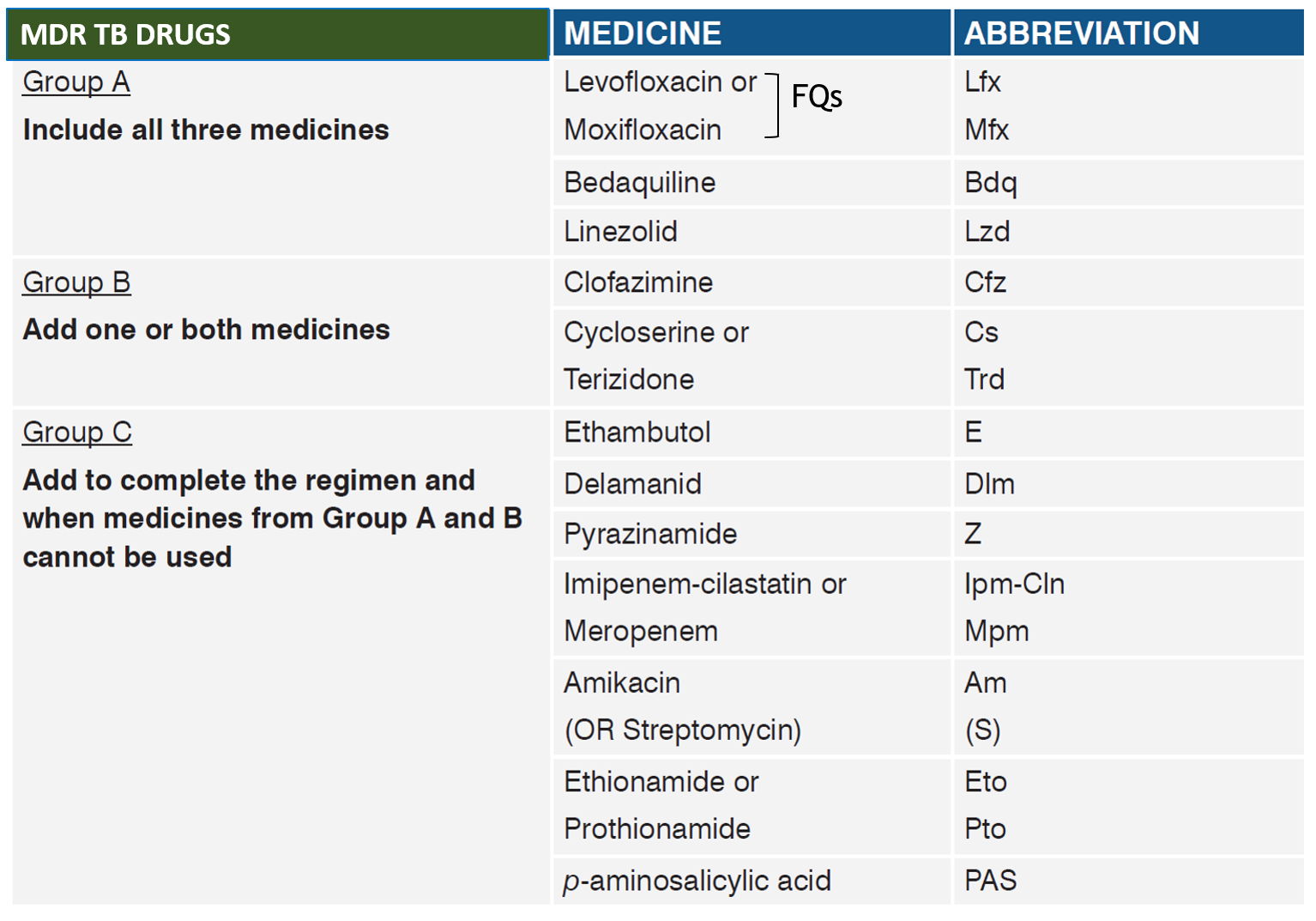
For MDR/RR-TB, the focus is on shorter Bdq containing oral regimen (BPaLM-6-month, all-oral treatment for drug-resistant tuberculosis consisting of bedaquiline, pretomanid, linezolid, and moxifloxacin). In case of issues with one of bedaquiline or delaminid/pretomanid, longer all oral regimen may be required. Patients who were on a longer oral MDR/XDR-TB regimen based on the history of exposure for >1 month and in whom resistance is not detected to Isoniazid (H) or FQ may be switched to shorter oral bedaquiline containing MDR/ RR-TB regimen based on the FL/SL-LPA results if the duration of longer oral MDR/XDR-TB regimen drugs consumed is <1 month. For Pre-XDR, with quinolone resistance, BpaL may have to be used. Treatment of each patient needs to be individualized to achieve greater success.
Short Regimens:
- BPaLM Regimen (6 months) : This regimen includes bedaquiline, pretomanid, linezolid, and moxifloxacin.
- 9-Month All-Oral Regimen: This regimen includes bedaquiline, levofloxacin/moxifloxacin, ethionamide, ethambutol, high-dose isoniazid, pyrazinamide, and clofazimine.
Longer Regimens:
- 18-20 Month Regimens: These regimens are considered for patients who cannot tolerate shorter regimens, or in cases of extensively drug-resistant TB, extensive forms of extrapulmonary TB, or previous treatment failure.
Monitoring and Follow-up
It is important to note that all drugs for TB have side effects. Monitoring for these side effects by both clinical evaluation and laboratory tests is very important, and in some cases, drug stoppage and replacement may be needed. Medicines should never be modified, stopped, or started unless advised and guided by the treating doctor.
Regular follow-up is the most important aspect of treatment, as some of the drugs in the regimens may need a change of dose after a certain time period. Follow-up also enables timely sputum smear and culture tests, as well as monitoring of drug side effects. With proper treatment, monitoring, and follow-up, TB in most cases is curable.
EXTRAPULMONARY TB
Tuberculosis can also affect other parts of the body. The sites outside the lung include lymph nodes (scrofula), abdominal organs (like intestines), heart covering or pericardium, bones (TB spine- Pott’s disease), kidney, fallopian tubes (can cause infertility), skin (lupus vulgaris), brain (TB meningitis), and all over the body (disseminated or miliary TB).
Diagnosis of extrapulmonary TB (EPTB) presents challenges with regards to collecting a sample for microscopic smear examination (for AFB), culture, and NAAT. Depending on the site of involvement, the specimen can be cerebrospinal fluid (CSF) by lumbar puncture in TB meningitis, pericardial/pleural/peritoneal fluid, or urine in genitourinary TB. Often repeat samples are needed for positive results. Other tests include tissue biopsy and histology (showing caseating granulomas), fine needle aspiration cytology (FNAC) with PCR and CT scans. DSTs should preferably be performed even though there is less data on drug resistance in EPTB. Concomitant sputum testing for pulmonary TB should be done.
Treatment with anti-TB drugs is the mainstay in the management of EPTB, and most guidelines recommend the same regimen for both EPTB and PTB. However, for TB meningitis, the drugs should be able to cross over the blood-brain barrier (isoniazid, pyrazinamide, levofloxacin, moxifloxacin, and cycloserine penetrate well into the CSF, ethambutol and PAS have poor or no penetration, while rifampicin and kanamycin penetrate the CSF well when the meninges are inflamed in meningitis). While 6 months of standard anti-TB medical therapy is generally considered adequate for most forms of EPTB, longer treatment is suggested for TB meningitis and for bone and joint TB. EPTB that is drug-resistant is treated with the same strategy and duration as drug-resistant PTB.
Monitoring and evaluation of the response to treatment in EPTB are often limited by the difficulty in obtaining follow-up specimens. Therefore, the response and cure are often assessed based on clinical and radiographic findings.
PARADOXICAL REACTION
A paradoxical reaction is generally defined as the clinical or radiological worsening of preexisting TB or the development of new lesions in a patient who initially improves with anti-TB therapy. A paradoxical reaction occurs more frequently in EPTB than in PTB. Tuberculosis-immune reconstitution inflammatory syndrome (TB-IRIS) is an abnormal, excessive immune response against alive or dead Mycobacteria tuberculosis that may occur in either HIV-infected or, more rarely, non-HIV TB patients.
Investigations should be performed to rule out other causes of clinical deterioration, such as secondary infections, treatment failure, multidrug resistance, poor compliance, or drug toxicity. DST is important to distinguish between a paradoxical reaction and treatment failure due to drug resistance.
Anti-TB treatment is continued as usual. In select patients with severe symptoms, corticosteroids may be given, and in some additional treatments like fluid tap/drainage and surgery may help.
CORTICOSTEROIDS IN TB
Corticosteroids have been used as an adjunctive in the treatment of EPTB for the prevention of fibrotic complications like strictures and adhesions. Corticosteroids have an established role mainly in TB meningitis and TB pericarditis to decrease morbidity and mortality. They may also help in pulmonary TB with associated pleural involvement. However, convincing evidence is lacking for abdominal or genitourinary TB. As mentioned, corticosteroids have some role in severe paradoxical pulmonary TB or EPTB.
TB PREVENTIVE TREATMENT
TB preventive treatment (TPT) consists of a course of one or more anti-TB medicines given to prevent the development of active TB disease in those who are infected or have been exposed to TB and are at a high risk of developing active TB or suffering from its complications. This includes close contacts of active TB patients, people with HIV, those undergoing dialysis or organ transplant, those taking immunosuppressive drugs, and vulnerable groups like health workers, migrants, the homeless, drug abusers, prisoners, etc.
Such people are diagnosed by testing positive with TB screening tests and a chest X-ray. TPT is different from the treatment of TB. Therefore, before starting TPT, active TB should be ruled out by sputum smear examination, culture, and NAAT.
The TPT regimens include isoniazid given daily for 6-9 months (6H), or rifampicin alone for 4 months (4R), or with isoniazid for 3 months (3HR). Another drug called rifapentine can be given together with isoniazid in a weekly dose for 3 months (3HP) or daily for one month (1HP). Rifapentine (300mg, also available as a fixed dose combination with 300mg Isoniazid) is approved and indicated for the treatment of latent tuberculosis in India as part of NTEP.
REFERENCES
Also read:
Interstitial Lung Disease (ILD) – Types, Risks, and Health Measures