Retina is the back curtain of the eye which receives the visual stimulus and sends it to the brain via the optic nerve. The retina is made up of two types of light receptors (photoreceptors) – the rods that are contrast-sensitive and important for night vision, and cones that are light-sensitive and responsible for color perception.
Retinal detachment
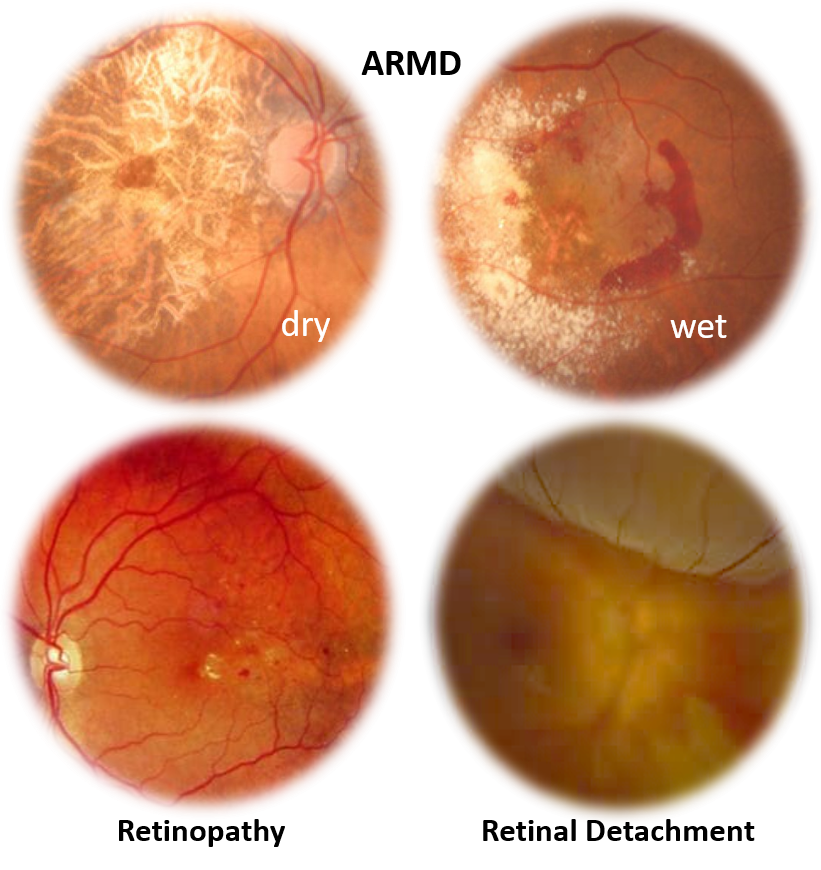
This can manifest as sudden visual loss (like a curtain falling) which can be due to trauma or occur spontaneously (especially in people with high myopia, degenerated retina, or prior retinal tears or trauma).
Retinal detachment is treated by surgery after viewing the retina with an indirect ophthalmoscope, and then sealing the tears with freezing (cryotherapy) or laser, followed by placing a buckle to attach and hold the retina. This is usually performed by a retina specialist.
Age-related macular degeneration (ARMD)
This is a common cause of gradual progressive vision loss with aging due to deterioration and deposits in the retina especially at the macula. Apart from increasing age, other risk factors linked to ARMD include family history, cardiovascular disease, and associated obesity and smoking, however many times no particular cause is established. Vision reduction usually central, manifests as an inability to work/read in dim light, blurring, dullening of colors, distortion of lines, decreased recognition ability, and noticing blind/blurred spots. Dry ARMD appears as yellowish-white deposits called ‘drusens’ in the retina that are made up of fats and degenerating glycoproteins. Sometimes the presence of abnormal new leaky vessels (neovascularization) can cause swelling and bleeding leading to quick deterioration of vision, and the ARMD is then said to be ‘wet’.
Diagnosis is established by ophthalmoscopy, optical coherence tomography (OCT), and angiography with a colored dye like fluorescein (blue) or indocyanine (green), that can help identify the leaky vessels.
Dry ARMD is managed with low vision aids, nutritional vitamin-mineral and antioxidant supplements with regular eye check-up and controlling cardiovascular disease risk factors. Wet ARMD is treated by eye injections of medicines that reduce leaky vessels (anti-VEGF drugs: ranibizumab, bevacizumab and aflibercept), and by sealing the leaky vessels with laser (photocoagulation) or using a photoactive drug (photodynamic therapy with verteporfin).
Retinopathy
It occurs due to the damage of the walls of the delicate blood vessels of the retina over time. The most established cause is diabetes (diabetic retinopathy) but it can also be linked to high blood pressure (hypertensive retinopathy) or cardiovascular disease and formation of plaques (atherosclerosis).
The damaged vessels can leak and bleed causing swelling and hemorrhages in the retina, especially the macula (maculopathy). This causes visual deterioration, blurring, distortion and seeing spots. Sometimes abnormal new leaky vessels can grow and bleed significantly (proliferative retinopathy) or an entire major retinal blood vessel may get blocked (retinal vascular occlusion) causing sudden vision reduction or loss.
Treatment involves meticulous sugar control, and managing other cardiovascular risk factors including blood pressure. A retinal angiography is performed followed by laser (photocoagulation) which can be focal for certain leaky vessels, done mainly in the macula region, or scattered all over the retina. Other treatments especially in proliferative diabetic retinopathy include anti-VEGF drugs: ranibizumab, bevacizumab and aflibercept), and photodynamic therapy (with verteporfin).
Retinal pigment diseases
These are rare and can be hereditary with the most well-known being retinitis pigmentosa. Symptoms are gradual reduction in vision especially of contrast, peripheral or night vision. These conditions are diagnosed on a retina examination, and treatment usually involves low vision aids and rehabilitation.
Vitamin A deficiency
Vitamin A is a part of the rods of the retina that perceive contrast, so its deficiency can also cause night blindness (reduced vision in dim light and low contrast). This is a significant problem in children from underdeveloped or poorer areas and is far rarer today due to the fortification of many food items with vitamin A as well as social programs for both nutrition awareness and administering vitamin A to children.
Vitreous hemorrhage
Hemorrhage and leakage of blood in the vitreous is usually caused by proliferative diabetic retinopathy, wet ARMD, retinal detachment or trauma. Vitreous hemorrhage is usually managed by observation for spontaneous clearance. If it is not resolving and is significantly affecting vision, a procedure called vitrectomy may be performed sometimes along with the sealing of the underlying tear/bleeding site with cryotherapy or laser, combined with retinal detachment surgery where needed.
Sometimes black shadowy specks called floaters may appear in front of the eye which move directionally with eye movement and are more prominent against clear backgrounds. These do not need any intervention as these are usually due to protein particles, fibers or blood cells in the vitreous. However, if they increase suddenly and significantly, it may suggest a vitreous hemorrhage or detachment.
OPTIC NERVE
Optic neuritis
It is the inflammation of the optic nerve. It maybe associated with multiple sclerosis, other autoimmune diseases, or infections, but often no cause maybe found.
Symptoms include eye pain which is worsened by eye movement, seeing flashes or flickering of light, along with reduced/loss of vision which can be full, central, one side or color perception.
Ophthalmoscope examination of the optic nerve head, optical coherence tomography-OCT, visual field test (perimetry) and magnetic resonance imaging (MRI)) along with some blood antibody markers are the diagnostic tests.
It is treated with corticosteroid drugs (usually methylprednisolone) given by intravenous injection. Vision usually improves with treatment, but may take a few months to return to normal with residual loss of some vision and/or color perception in certain people.
Optic neuropathy
This condition is sometimes called optic atrophy, and refers to the damage to the optic nerve. This can happen due to different causes like lack of adequate blood supply (ischemia), trauma, radiation, compression by swellings/tumors, infections, toxicity (due to certain drug/alcohol/chemicals/smoking), repeated attacks of optic neuritis, certain nutritional deficiencies (like vitamin B12, B1) and sometimes hereditary/genetic conditions. The symptoms are visual clouding, a decrease in visual quality and color perception, and loss of vision over time.
Also read:
Vision Reduction and Loss – Understanding Causes and Points for Timely Action

