What is Uveitis
Uveitis is the inflammation of parts of the uvea or uveal tract of the eye. The uvea is a pigmented structure and is made up of the following – the iris in front that we see as the color of our eyes; the ciliary body that is the backward extension of the iris on either side which attaches the lens of the eye through zonules; the choroid which is the backward extension of the ciliary body on either side and lines the back of the retina.
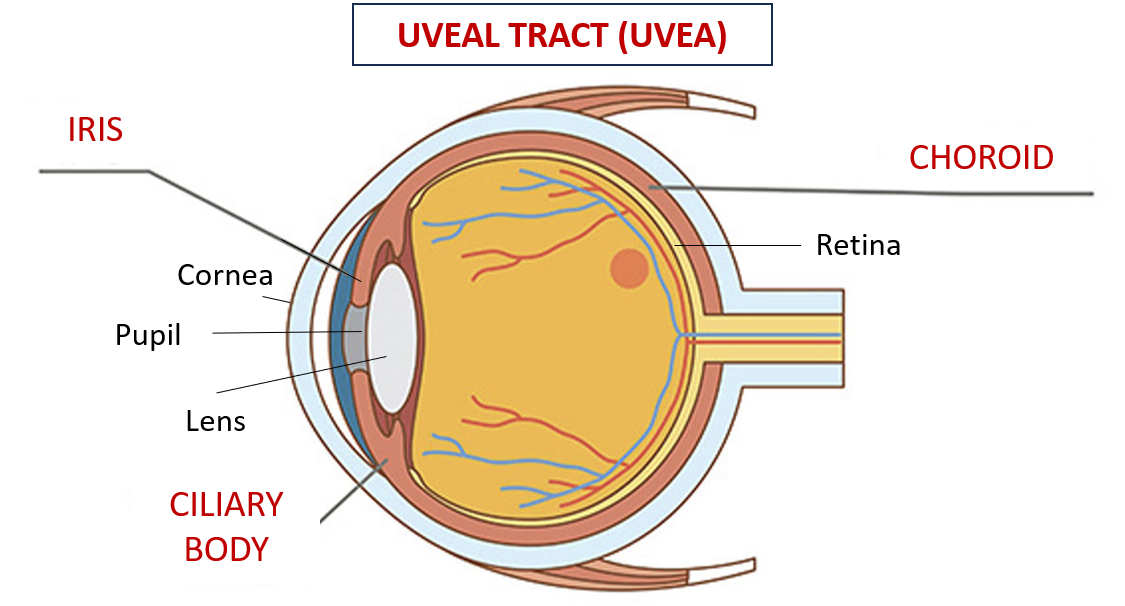
Uveitis includes iridocyclitis (inflammation of the iris and ciliary body – anterior uveitis), and choroiditis (inflammation of the choroid – posterior uveitis).
Causes
It can occur due to a variety of causes and associations (as part of syndromes).
Unilateral (one eye) uveitis can occur post-trauma, as part of an eye infection (like HIV cytomegalovirus, herpes zoster, histoplasmosis, syphilis, and toxoplasmosis), and post eye-surgery.
Bilateral (both eyes) uveitis is commonly associated with systemic conditions and autoimmune diseases causing symptoms in other body organs also. These include rheumatoid arthritis, ankylosing spondylitis, systemic lupus erythematosus (SLE), sarcoidosis, psoriasis, inflammatory bowel disease and other autoimmune diseases.
Sometimes uveitis can be a response to some eyedrops (like ant-glaucoma drugs brimonidine or prostaglandin analogs) but the inflammation is mild and reversed on stopping the drug. Eye injections of antibiotics or anti-VEGF drugs for retinal conditions can sometimes cause uveitis. Systemic drugs (taken orally/or by injection) like anti-cancer drugs, immunomodulators, some antibiotics, bisphosphonates (for osteoporosis), and some vaccines can also cause uveitis.
Very rarely uveitis may be a sign of lymphomas or eye cancers. Tattoo ink is also one of the substances that incites uveitis.
Symptoms
The symptoms include:
- eye redness
- eye pain
- light sensitivity (called photophobia)
- blurring or decreased vision
- presence of floaters in front of the eye.
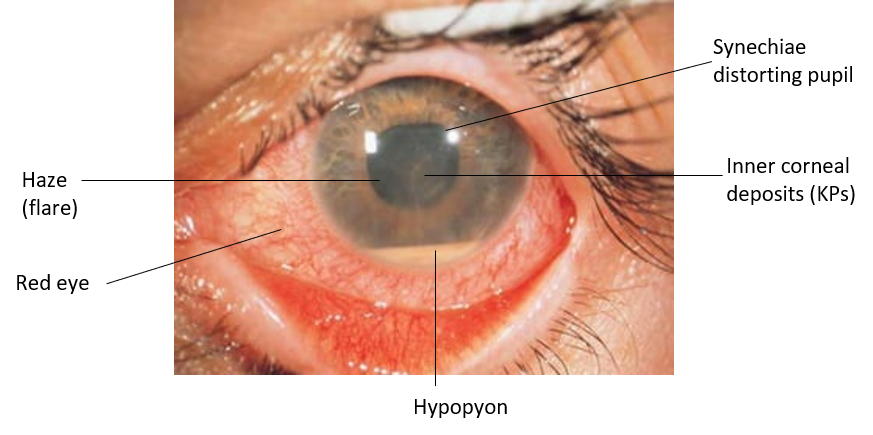
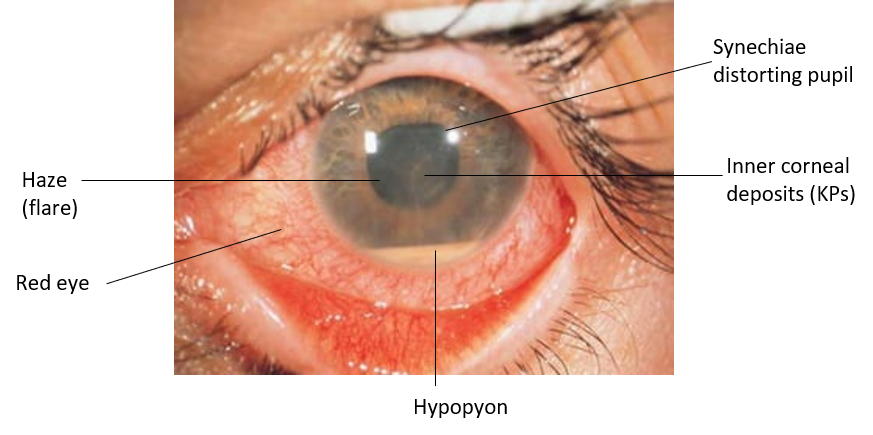
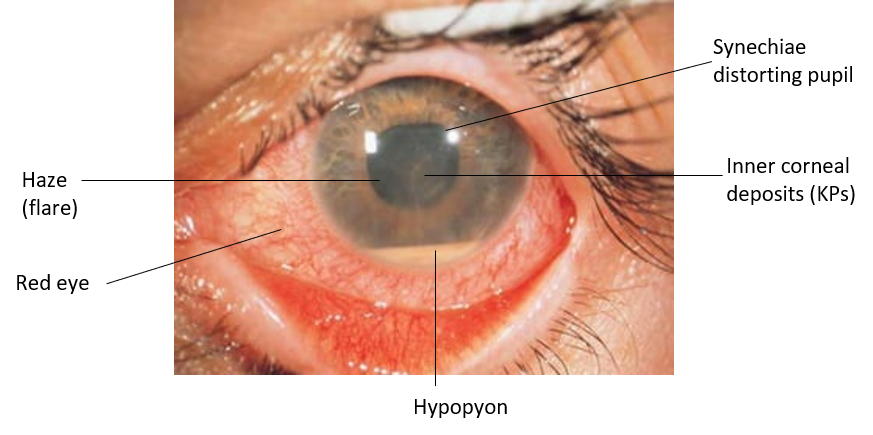
On examination through a slit lamp, one may see
- A haze in the anterior chamber (in front of the iris), called flare is present caused by an increase in protein content in the aqueous humor (front fluid of the eye). This looks like a moving projector beam in a dark, room.
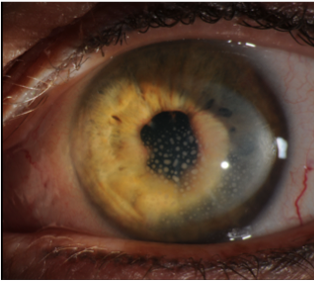
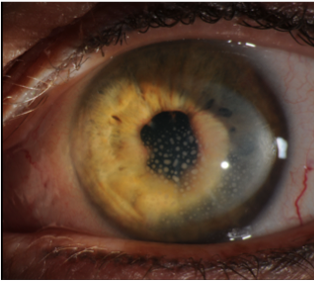
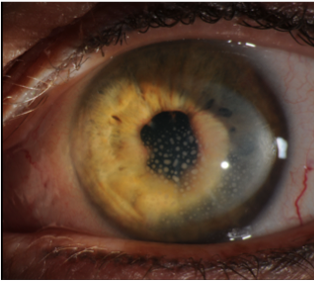
- Keratic precipitates (KPs) are clumps of white blood cell clumps on the inner corneal surface.
- Synechiae are sticky adhesions that are seen in iridocyclitis and may form between the iris and back of the cornea (anterior synechiae), and the iris and lens behind (posterior synechiae). These synechiae cause distortion of the pupil and can lead to increased eye pressure (glaucoma) as drainage of the aqueous fluid is compromised.
- Hypopyon is a layer of white blood cells in the anterior chamber, seen in severe iridocyclitis.
Management
After clinical examination, the doctor may order some blood and imaging tests to rule out associated autoimmune conditions and also refer to other specialists accordingly.
The treatment includes using corticosteroids as eye drops, or sometimes as eye injections or oral tablets to control the inflammation. In severe cases, stronger immunosuppressive injections may be needed. Eye drops to widen (dilate) the pupil called mydriatics are also given as this helps to relieve pain and reduce the formation of synechiae. Infection, when present is treated with antibiotics or anti-viral medication.
Complications
Uveitis can present with some short-term and long-term complications.
Secondary glaucoma is sometimes seen due to synechiae blocking the drainage angle and preventing aqueous flow (closed-angle glaucoma), or the inflammatory cells clogging the trabecular meshwork at the angle through which the aqueous fluid drains out (open-angle glaucoma). Therefore, eyedrops to lower intraocular pressure may need to be temporarily used.
Cataracts can develop due to inflammation, posterior synechiae, or due to prolonged use of corticosteroid medicines.
Choroiditis (posterior uveitis) can sometimes cause inflammation of the adjoining retina (chorioretinitis) which can cause swelling of the retina, especially of the macula (macular edema), leading to a reduction in vision. Chorioretinitis can also cause proliferative retinopathy where abnormal new blood vessels grow on the surface of the retina, which can bleed on the retina or into the vitreous, and such hemorrhage can cause severe vision loss.
Also read:
Autoimmune Diseases: 15 Well-Known Types and Medical Management
Vision Reduction and Loss – Understanding Causes and Points for Timely Action

