WHAT IS GLAUCOMA
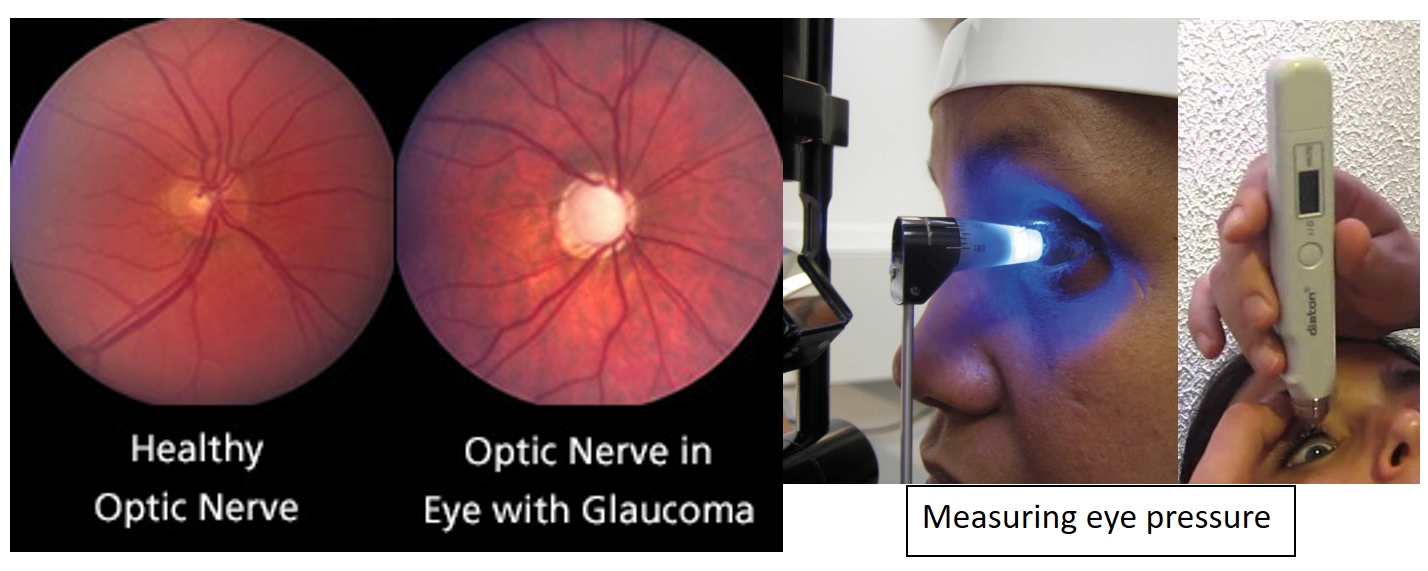
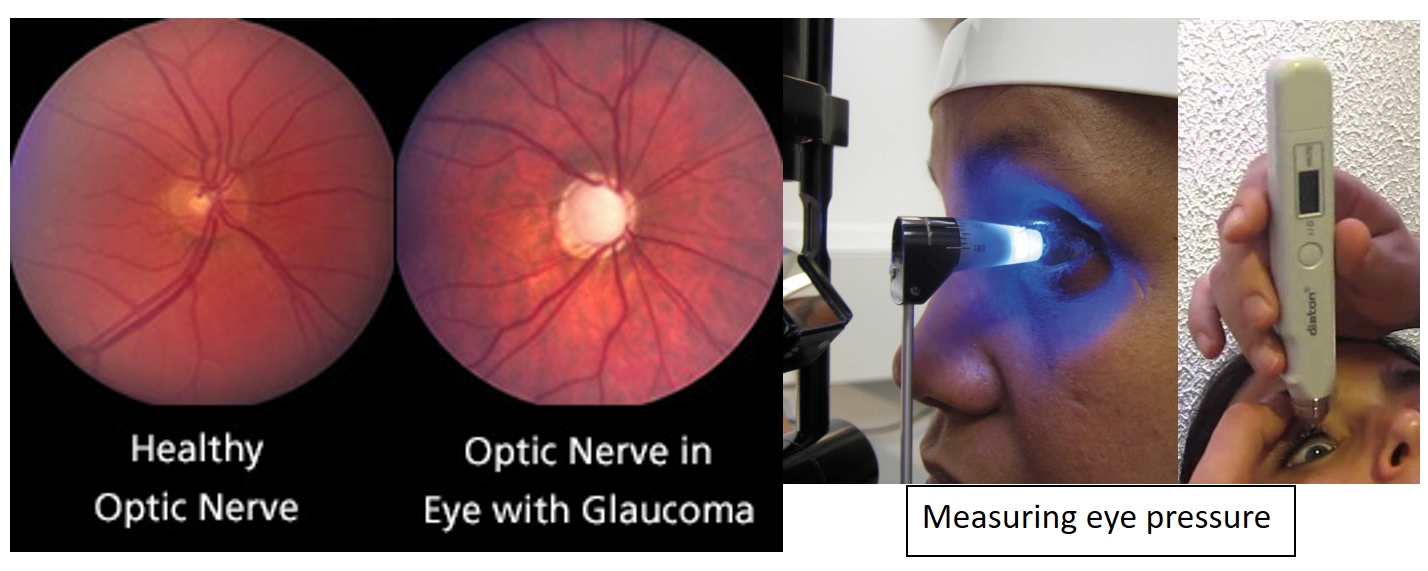
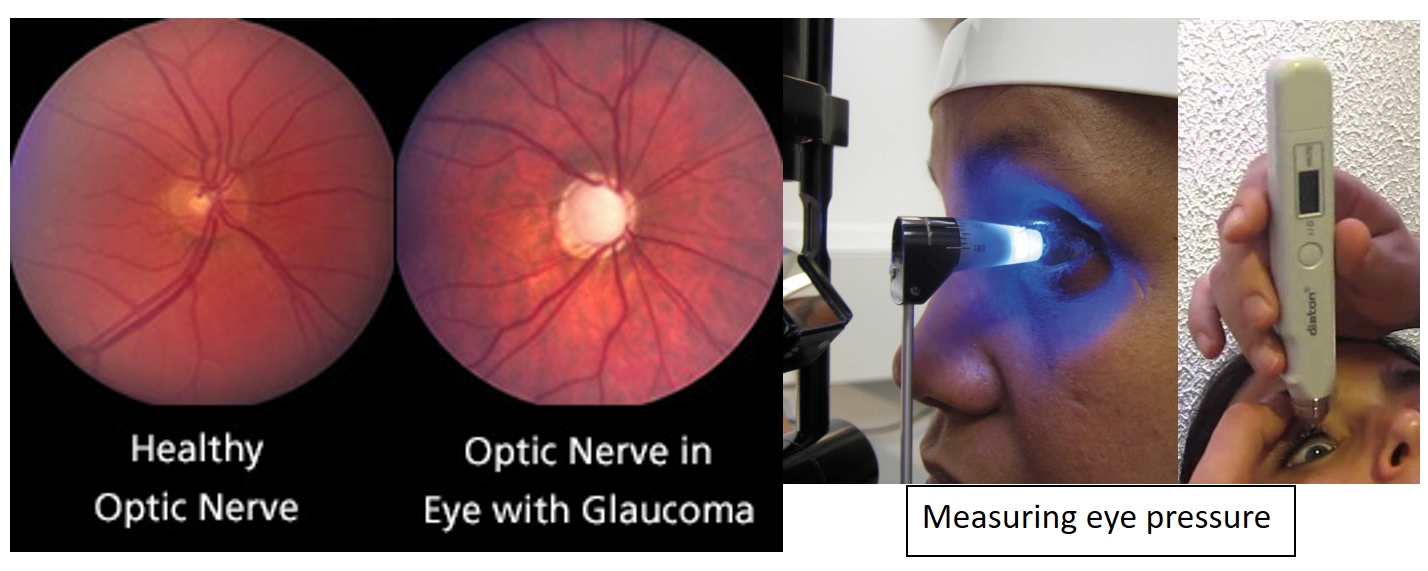
Glaucoma comprises of a group of different eye diseases, which result in vision loss. Usually, there is damage to the optic nerve due to the increase in eye pressure. This results in loss of peripheral vision initially, and extends later to central vision also.
When there is no underlying cause for this damage, it is classified as primary glaucoma. In case, the disease is because of a reason such as trauma, surgery, other eye diseases like uveitis, or use of medicines like steroids, it is said to be secondary glaucoma.
Another classification is based on the drainage of the eye fluid (called aqueous humor) out through the angle of the eye: if the drainage angle is open, and there is no mechanical barrier to the drainage of the fluid within the eye, the glaucoma is said to be Open Angle Glaucoma. If the drainage angle is narrow or closed, the glaucoma is called Angle Closure Glaucoma.
In a subgroup of patients, the optic nerve gets damaged, even though eye pressure remains normal. This is called Normal Tension Glaucoma.
SYMPTOMS
Usually, patients have no symptoms, until the advanced stages. Therefore, an annual comprehensive eye examination is essential for early diagnosis especially if risk factors are present.
Since the irreversible vision loss continues silently, glaucoma is often called the silent thief of sight. That said, a diagnosis of glaucoma should not scare you since it can be controlled with timely treatment.
Sometimes, especially in secondary and angle-closure glaucoma types, patients may complain of one or more of the following symptoms:
1. Eye pain
2. Headaches
3. Blurring of vision
4. Frequent change of glasses
5. Coloured haloes around bright lights
RISK FACTORS
Only a comprehensive eye examination by a trained eye doctor can diagnose glaucoma, or even calculate the risk for glaucoma in any individual person. However, listed below are the significant risk factors:
• High intraocular or eye pressure (IOP)
• Age 60 or above for Open-angle glaucoma; 40 or above for Angle-closure glaucoma
• Racial predilection: Africans and Hispanics have a higher risk; Indians and South East Asians are more prone to Angle-closure glaucoma
• Family history of glaucoma
• Optic nerve appearance (increased cup-disc ratio) or decrease in the nerve fibers of the retina
• Thin cornea
• High Myopia or Hypermetropia (use of glasses for high minus or plus numbers)
• Eye inflammation (Uveitis) or long-term use of corticosteroid medicines
• Diabetes
• Eye Injury or Surgery
TESTS AND DIAGNOSIS
The eye doctor, after a complete eye evaluation, may recommend some extra investigations, if you are at risk for glaucoma.
These include:
1. Visual field (Perimetry) -analyses the optic nerve function by detecting a loss in peripheral vision
2. Pachymetry- measures the thickness of the cornea
3. Optic nerve photographs
4. Optical coherence tomography (or OCT) or GDx (which uses a scanning laser) to analyze the optic nerve structure and the retinal nerve fiber layer (RNFL)
5. Diurnal variation of IOP or Water Drinking Test to see how the eye pressure fluctuates
6. Gonioscopy- assesses the drainage angle of the eye
These tests may be repeated once or more, annually, to monitor progression if clinical suspicion is high. In diagnosed cases especially with advanced disease, the tests may be done more often, depending on the severity of the disease.
TREATMENT OPTIONS
It is important to remember that even though there is no one-shot cure, glaucoma progression and blindness can be adequately controlled and prevented respectively, by proper, timely and regular treatment.
The treatment options include:
- Eye drops: Primary Open-angle glaucoma can usually be controlled with the use of eye drops in most cases. However, one must remember that these drops must not be missed, and are to be used lifelong.
Depending on the severity of the disease, you may require more than one kind of eye drops. Often, your doctor will start with one eye drop, and add more eye drops, if required, during subsequent follow-up visits.
Angle-closure and secondary glaucomas also can be managed medically. The former, however, usually requires a laser treatment in addition to eye drops.
Medical therapy may be augmented or substituted by both, laser, or/ and surgery. - Laser: As mentioned earlier, Angle-closure glaucoma is treated first by a laser procedure called laser peripheral iridotomy, which restores the drainage of fluid inside the eye. In this, a small hole is made in the iris (the brown or black part of the eye that gives it colour), using a laser.
Another laser procedure called selective laser trabeculoplasty is sometimes used in Open-angle, and some cases of Angle-closure after laser peripheral iridotomy. This procedure increases the drainage of the fluid within the eye from the already patent drainage angle, and helps in better eye pressure control. Sometimes, it means that the patient may not require eye drops, or fewer number of eye drops. This procedure is, however, not effective lifelong, and may require repeating. - Surgery: Some patients, especially with advanced disease or secondary glaucomas, may need surgery for the control of eye pressures. The main surgical modalities include:
a. Trabeculectomy,
b. Non-penetrating surgery
c. Shunt or implant surgery: Ahmed Glaucoma Valve (AGV) or AADI (Aurolab Aqueous Drainage Implant)
d. Minimally Invasive Surgery
Points to remember
- Timely diagnosis and appropriate treatment are key to glaucoma prevention.
- A comprehensive annual eye check is essential for everyone above the age of 40, especially if any risk factors are present.
- Even though glaucoma cannot be prevented or cured, blindness or significant vision loss from glaucoma can be prevented if the disease is diagnosed and treated in time.
- You must follow your doctor’s advice about the need for glaucoma investigations, and get the tests done on time. This is true even if you have no symptoms or vision disturbances.
- In case you are diagnosed with glaucoma, there is no need to panic or despair. As long as you adhere to the treatment prescribed, you will not lose vision.
- When advised treatment, you must discuss the risks and benefits with your eye doctor, and participate actively in treatment planning.
- In case of any side effects, please contact your eye doctor, and discuss the change in treatment plans.
- In case you are using any other medicines, or alternate and complementary therapy, please do let your glaucoma doctor know.
Dr. Shibal Bhartiya is an ophthalmic surgeon at the Fortis Hospital and Research Institute, Gurugram. She has a special interest in the diagnosis and management of Glaucoma and Ocular surface diseases. Prior to Fortis, she was a Senior Clinical Research Fellow in Glaucoma services of the Department of Clinical Neurosciences, University of Geneva, and Senior Research Associate at Dr. R P Centre for Ophthalmic Sciences, AIIMS, New Delhi. Dr. Bhartiya is the Managing Editor of the Journal of Current Glaucoma Practice, the official journal of the International Society of Glaucoma Surgery.
Also read-
Vision Reduction and Loss – Understanding Causes and Points for Timely Action