Female infertility is not an uncommon problem. Infertility is defined as a couple not being able to get pregnant (conceive) after one year (or longer) of unprotected intercourse. It could be because of male, female, or both factors, therefore infertility involves a couple’s assessment and management. It is seen in 1 out of every 6 couples.
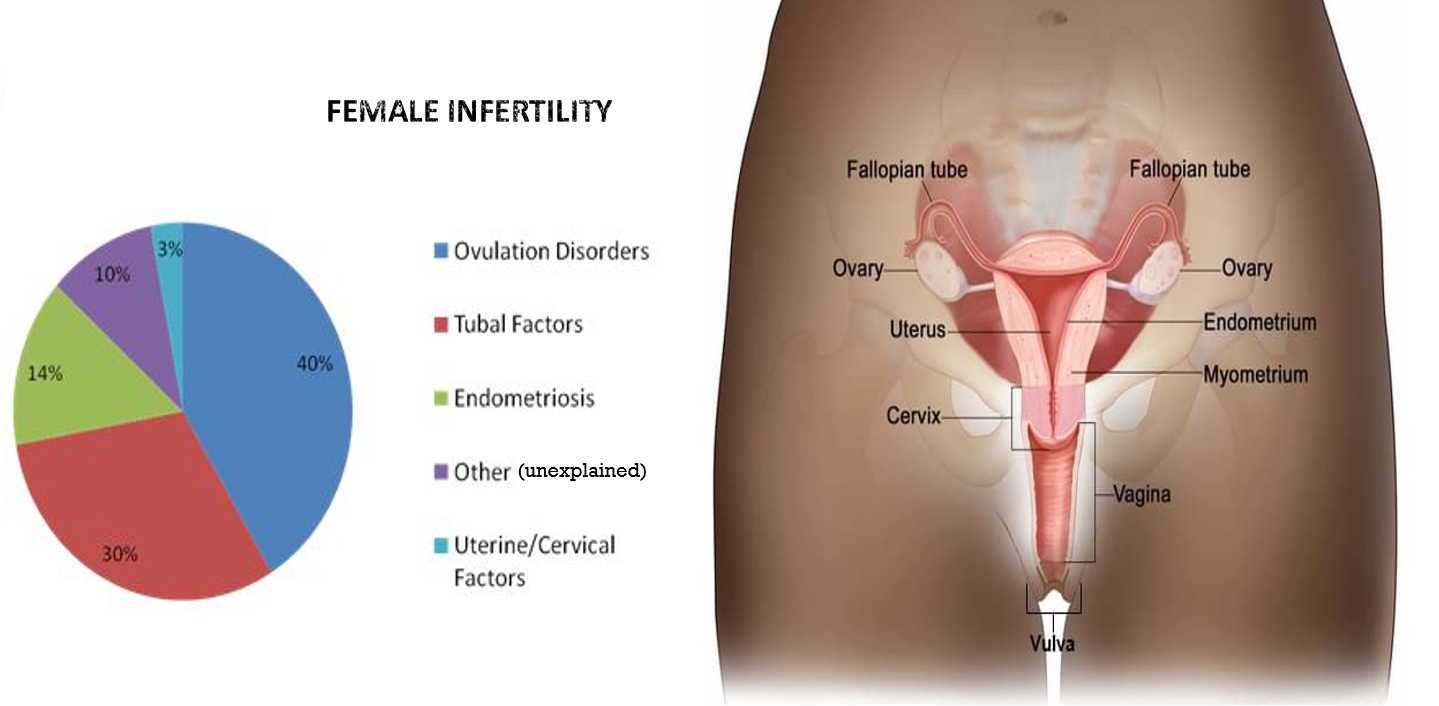
FEMALE REPRODUCTIVE ANATOMY AND FUNCTION
The female reproductive parts include the 2 ovaries and tubes (fallopian tubes) on either side, entering the uterus (womb) which leads down to the cervix and the vagina. Each of the ovaries contains a round collection of cells forming sacs called follicles, each of which contains an egg. One of these follicles releases an egg (ovulation) every month. After the egg is shed, the left-over collapsed follicle is called corpus luteum.
The onset of menstruation is called attaining menarche. A normal menstrual cycle has a usual frequency of about 25-35 days and lasts around 5-7 days.
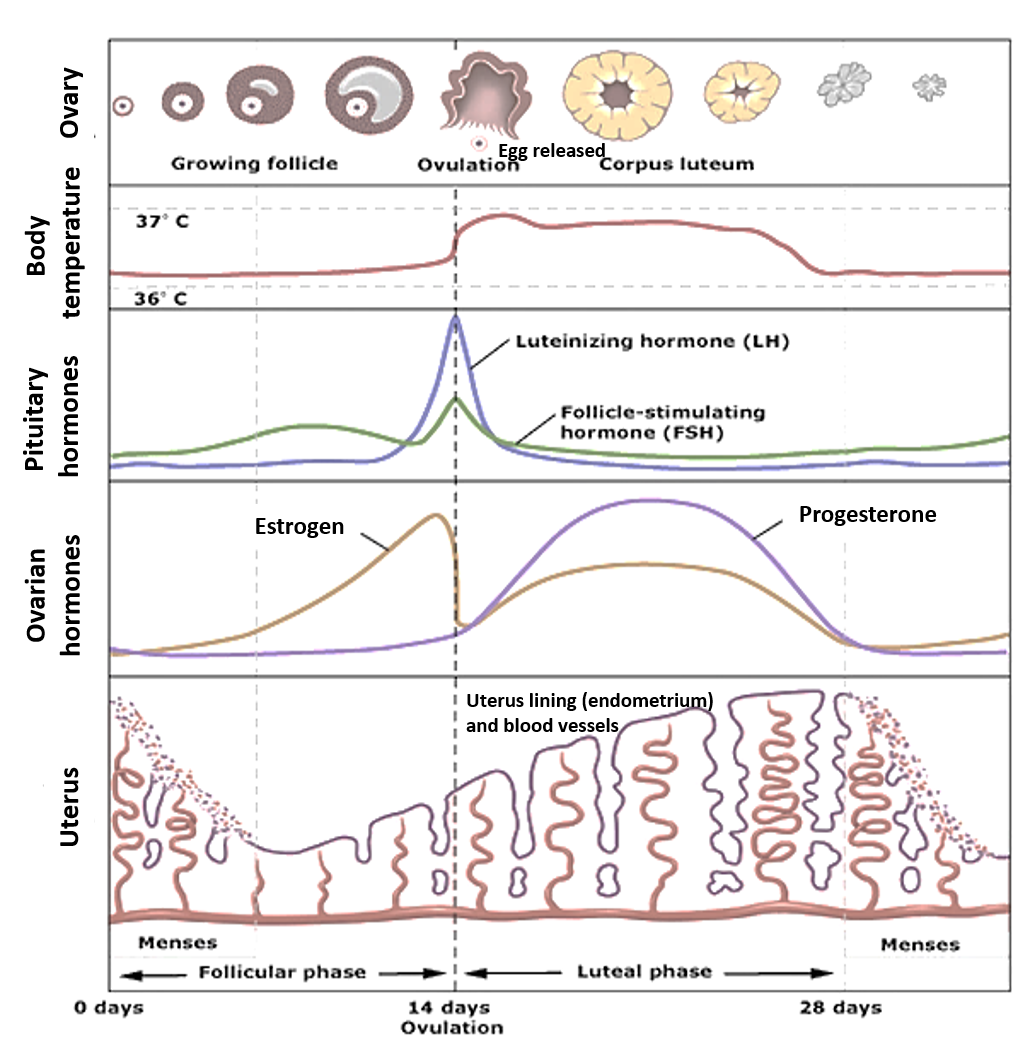
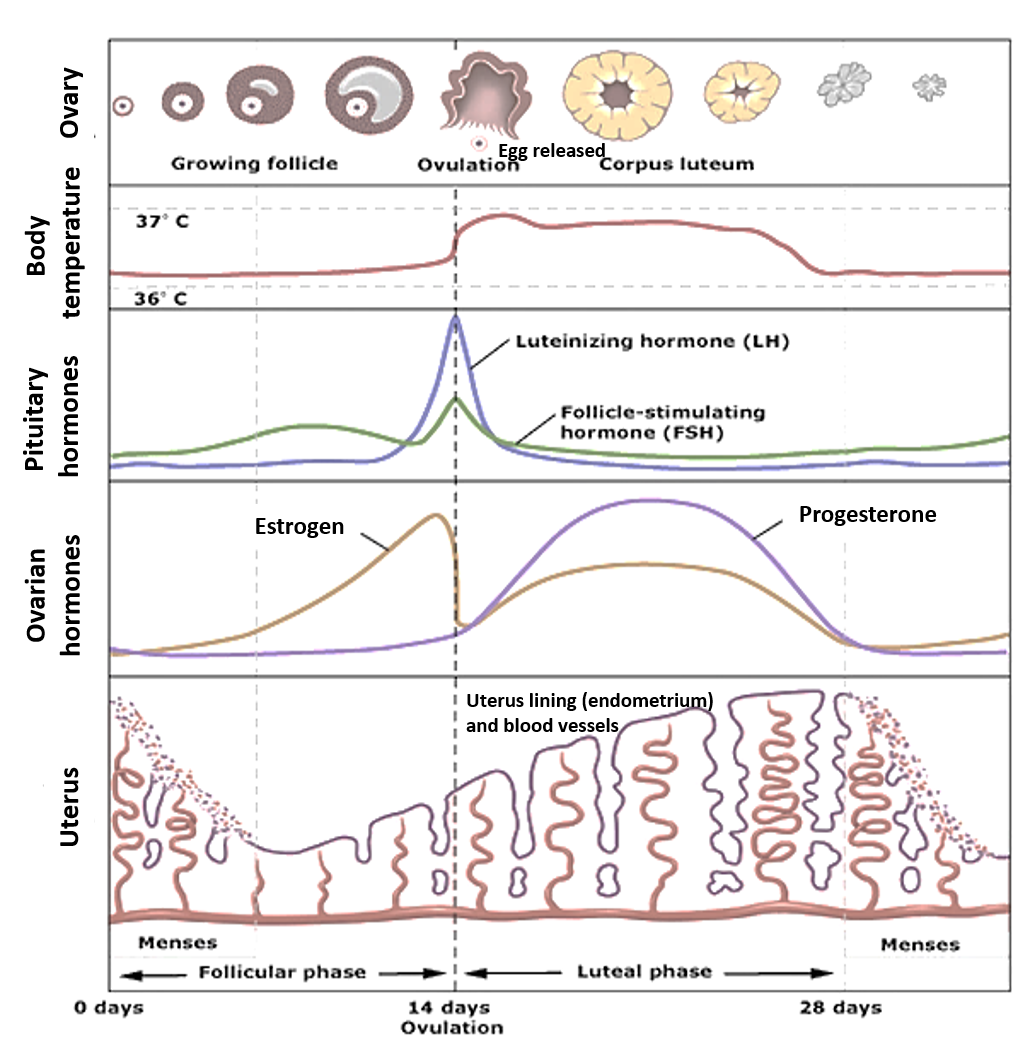
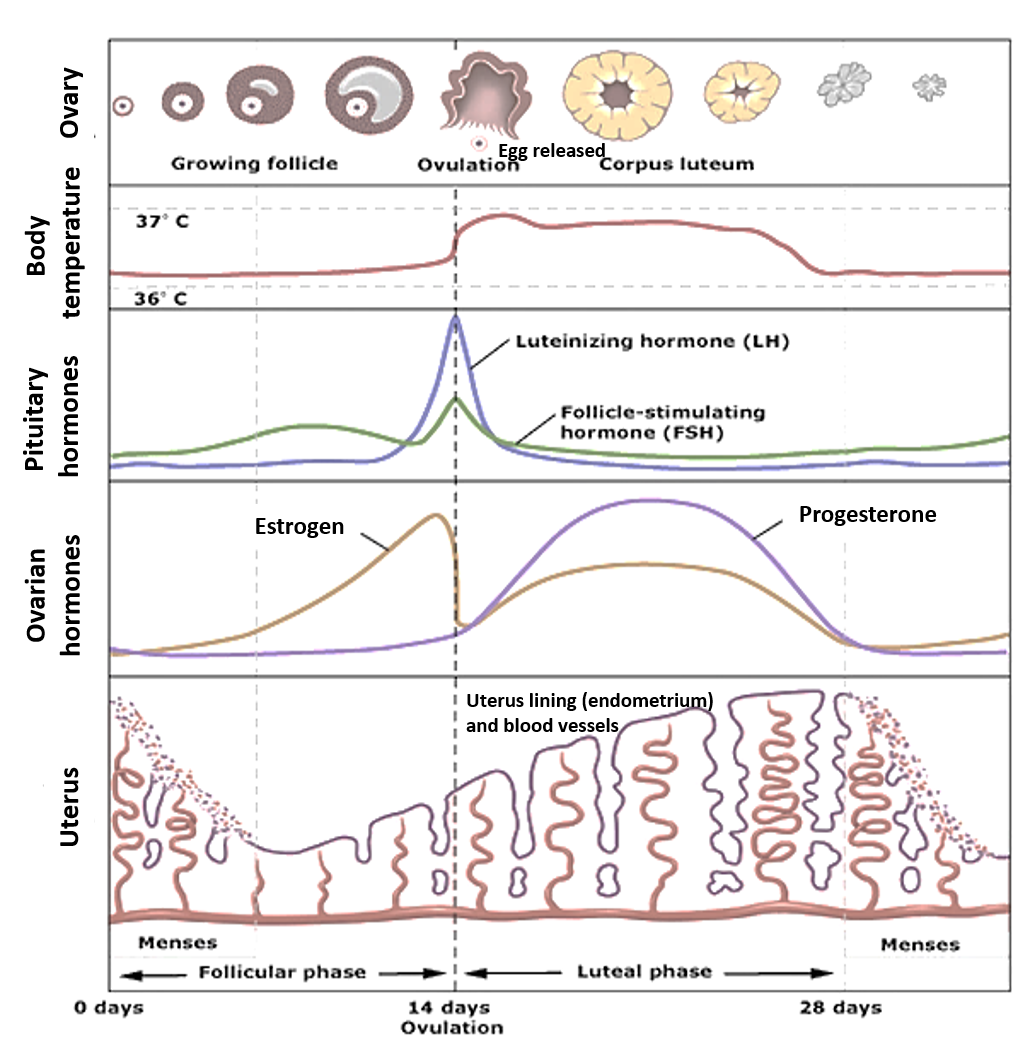
A woman’s menstrual cycle is an interplay and balance of hormones. The ovarian hormones estrogen (produced by the developing follicle) and progesterone (produced by the corpus luteum) are dominant respectively in the stages of menstruation before (follicular phase) and after (luteal phase) ovulation. These hormones are regulated by other hormones called gonadotropins (follicle-stimulating hormone- FSH, and luteinizing hormones-LH) released from the pituitary gland at the base of the brain.
Estrogen (estradiol) helps in the development of the follicles and the egg contained in them till one of the follicles ‘ripens’ and is ready to release the egg. FSH helps to maintain adequate estrogen levels. Estrogen level thereafter drops and a surge in LH causes the egg to be released (ovulation). The remaining follicle now called the corpus luteum produces progesterone the levels of which rise to further thicken the lining of the uterus (endometrium) and increase its blood supply. If conception does not occur, progesterone levels fall, and menses (bleeding) start to shed the thickened uterus lining and extra blood supply.
A hormone called Anti Mullerian Hormone (AMH) has a balancing effect on the monthly cyclical actions of FSH and LH during the process of egg maturation and release (ovulation). The amount of AMH present is a reflection of follicular growth.
Prolactin is a hormone that increases milk production in the breast and its main role is post-pregnancy during lactation. In some women there may be subclinical rise in prolactin levels that could lead to suppression of ovarian and pituitary hormones, leading to impaired egg development and ovulation.
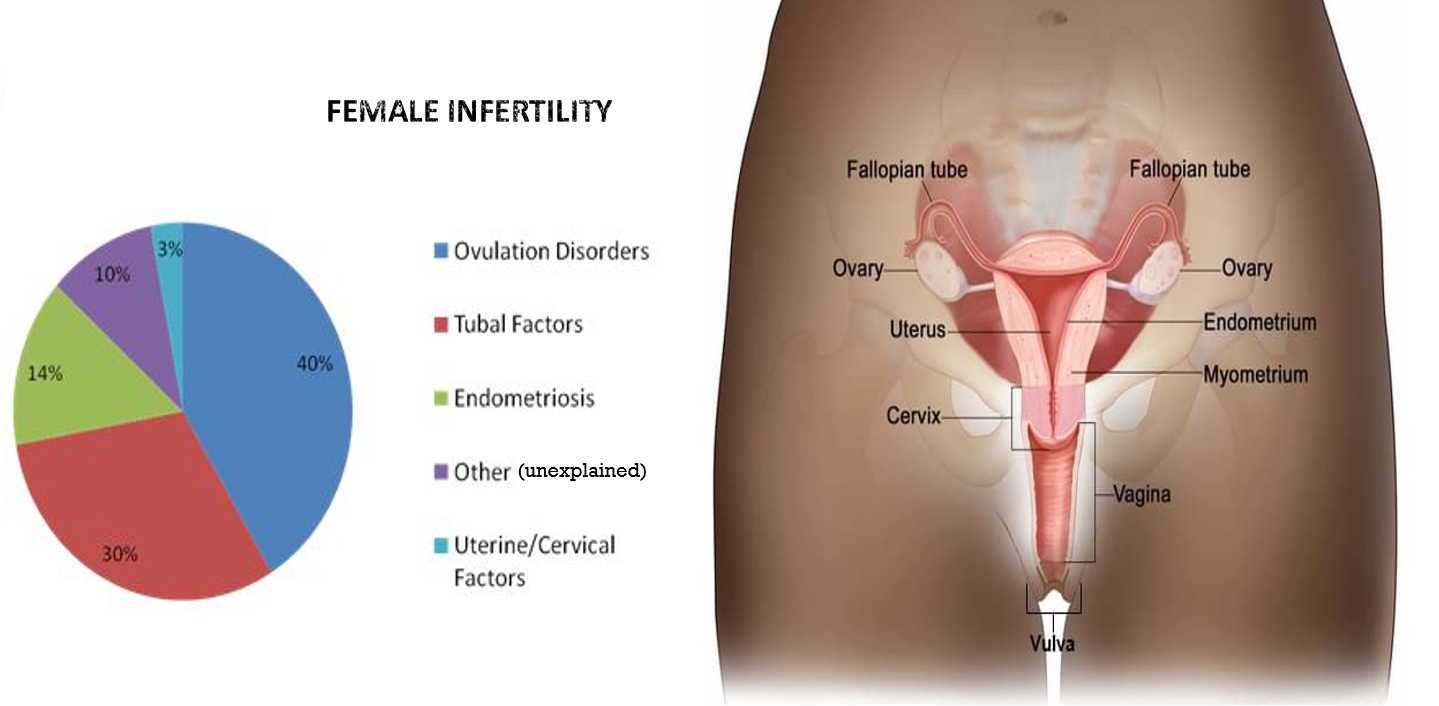
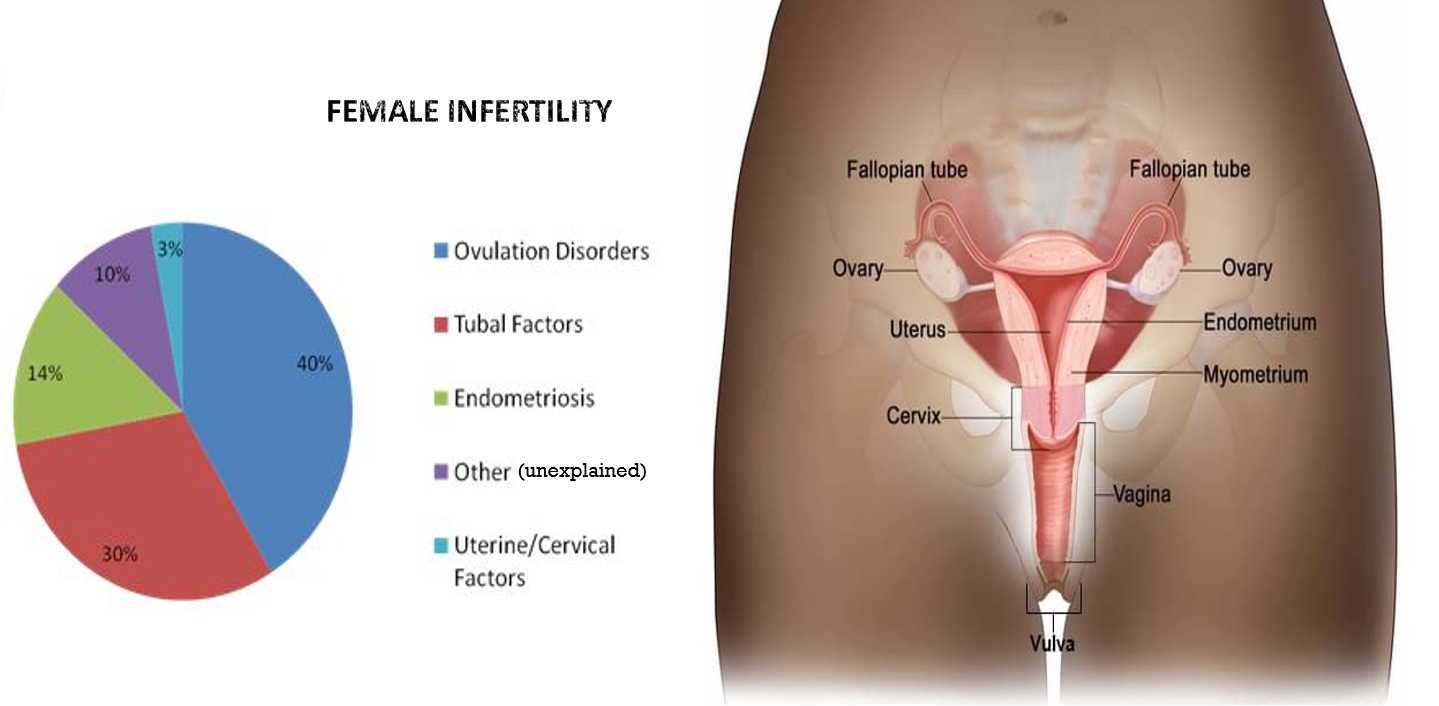
CAUSES OF FEMALE INFERTILITY
The causes could be classified as following:
Ovulation disorders
These affect the ovary, development of the follicle and egg, and its release (ovulation), and include:
- Increased age
- Nutritional factors – Vitamin-Mineral deficiency, high processed carbohydrates, and trans/saturated fat, low natural foods, fruits-vegetables, PUFA including omega 3 fatty acids, and protein.
- Lifestyle factors – Stress, inadequate sleep, fatigue, sedentary habits, obesity, smoking, alcohol abuse, use of narcotic/recreational drugs.
- Hormonal imbalance – Seen in PCOS, irregular contraceptive use, increased prolactin, abnormal thyroid hormone levels, and premature ovarian failure.
Tubal causes
- Blocked fallopian tubes due to previous tubal surgery (salpingectomy),
- Ectopic pregnancy in the past (implantation in the tube leading to its damage and scarring)
- Pelvic inflammatory disease (tubal infections).
Uterus/Cervix causes
- Endometriosis (most common cause)
- Thick cervical mucus blocking sperm entry
- Uterine anatomical anomalies and Fibroids preventing implantation
- Infections of the uterus and cervix
Sometimes it may be difficult to find a cause, and infertility may remain unexplained.
DIAGNOSTIC EVALUATION
It is important to simultaneously also evaluate for male infertility in the partner.
Female infertility evaluation includes a general physical examination, a pelvic examination to check for growths/other abnormalities, and when needed collection of swabs (to check for infection and mucus quality).
This is followed by blood tests for hormones and pelvic ultrasonography (USG)
Hormones that are tested in the blood are estradiol (estrogen), progesterone, prolactin, AMH, FSH, LH, thyroid and insulin. The timing of testing blood hormones is the 2nd or 3rd day of the menstrual cycle for AMH, prolactin, estrogen, FSH and baseline LH. On 13-15th day, LH levels are repeated to check for surge. In luteal phase (2-3 days before the expected period date progesterone levels are tested. Thyroid hormone, and insulin levels can be tested anytime.
Primary Ovarian Failure refers to a woman younger than age 40 beginning to have irregular periods or stops having periods for 4 months or longer, with consistently high FSH (as high as menopause), high LH, and low estrogen in 3 blood tests 15 days apart.
Pelvic ultrasonography (USG) looks for the development of follicles and eggs. Normal follicle count on USG is 6-12 (<6 is low reserve). Ovarian reserve determinants are AMH level + follicular count, with estradiol and FSH level on day 2-4 of the cycle. A count >12 follicles of 2-9mm in size suggests PCOS. Overall, follicles of 16–22 mm are more likely to contain mature eggs than smaller follicles (to be kept in mind for egg retrieval during assisted reproductive techniques), while larger follicles are more likely to contain post-mature eggs.
Other tests done to diagnose structural abnormalities and patency of the tube include Hysterosalpingography and Laparoscopy.
TREATMENT
One always begins with lifestyle solutions and natural therapies, and then moves on to hormones, drugs and procedures as required.
Improving sexual productivity through more frequent intercourse, especially around the period of ovulation (like daily or alternate day), from 5 days before to after predicted ovulation in the middle of the cycle) will be advised. The avoidance of lubricants by the female may also help preserve the sperms better.
Diet should be rich in green vegetables, fruits, curd, PUFA, and whole grains, with adequate amounts of water. Avoidance of high-sugar items, and too much trans/saturated fat, alcohol, and refined carbs is beneficial. Adequate sleep, stress management, adequate physical exercise, quitting smoking, and intake of recreational drugs is important.
Natural or dietary supplements that have some scientific evidence of benefit, may be prescribed by many doctors to improve general health, improve sperm production and function, and reduce oxidative stress in the body. These include L-arginine, coenzyme Q10, vitamin E, B6, B12, folic acid, selenium, and zinc. Herbal supplements include vitex agnus castus, ashwagandha, ginseng, red clover and soy which may also be available as combinations, but still need more robust clinical evidence.
Psychological treatment may be needed if the evaluation reveals underlying stress, anxiety, or depression which is affecting sexual desire. In such cases, some relaxation techniques like breathing exercises, mindfulness, meditation, counseling and psychotherapy (cognitive and behavioral therapy) may be advised and be beneficial. Medicines for anxiety-depression may be given for some time.
Treating Gynecological infections like vaginitis, cervicitis, endometritis, or pelvic inflammatory disease, requires a course of appropriate antibiotics that may be given to both partners in certain kinds of infections.
Treating Underlying Conditions like PCOS, endometriosis, and thyroid problems is important.
Drugs and hormonal treatments that regulate the menstrual cycle and stimulate ovulation are given to improve the chances of conception.
Clomiphene citrate and letrozole work like hormones to trigger ovulation and improve egg development and quality, with the latter being preferred in PCOS patients.
Gonadotropins are given as injections and stimulate the ovary to produce eggs (FSH) or help in egg maturation and release (hCG-human chorionic gonadotropin). These are also used along with assisted reproduction techniques like IVF. There is an increased risk of multiple pregnancies (twins, triplets) and premature babies with gonadotropin use. Rarely a condition called ovarian hyperstimulation syndrome (OHSS) can occur that causes swollen and painful ovaries, abdominal pain, and nausea-vomiting, and sometimes breathlessness.
Bromocriptine is used when ovulation problems are caused by excess production of prolactin (hyperprolactinemia).
Surgery is reserved for structural problems or specific conditions like endometriosis, fibroids, polyps, blocked tubes, adhesions in the pelvic region, etc. Hysteroscopy or laparoscopy are the two most common surgical approaches for female infertility.
Assisted reproductive technology (ART) involves obtaining the sperms (semen) from the male through normal ejaculation, sperm retrieval techniques, surgical extraction, or from donor individuals. The sperms are then inserted into the female genital tract, or used to perform in-vitro fertilization (IVF). IVF involves an egg being combined with sperm in vitro. The process involves monitoring and stimulating a woman’s ovulatory process, egg retrieval or removal from the ovarian follicles using a thin needle guided by ultrasound, and letting a man’s sperm fertilize the egg in a culture medium in a laboratory (test-tube baby) and then reimplanting the fertilized egg in the woman’s womb.
Alternate options include considering surrogacy or adoption, if all other treatments do not work out.
Also read:
Endometriosis: 5 Important Points for Understanding and Awareness
Gynecological Infections – Vaginitis and Pelvic Inflammatory Disease


