Male infertility is not an uncommon problem. Infertility is defined as a couple not being able to get pregnant (conceive) after one year (or longer) of unprotected intercourse. It could be because of male, female, or both factors, therefore infertility involves a couple’s assessment and management. It is seen in 1 out of every 6 couples.
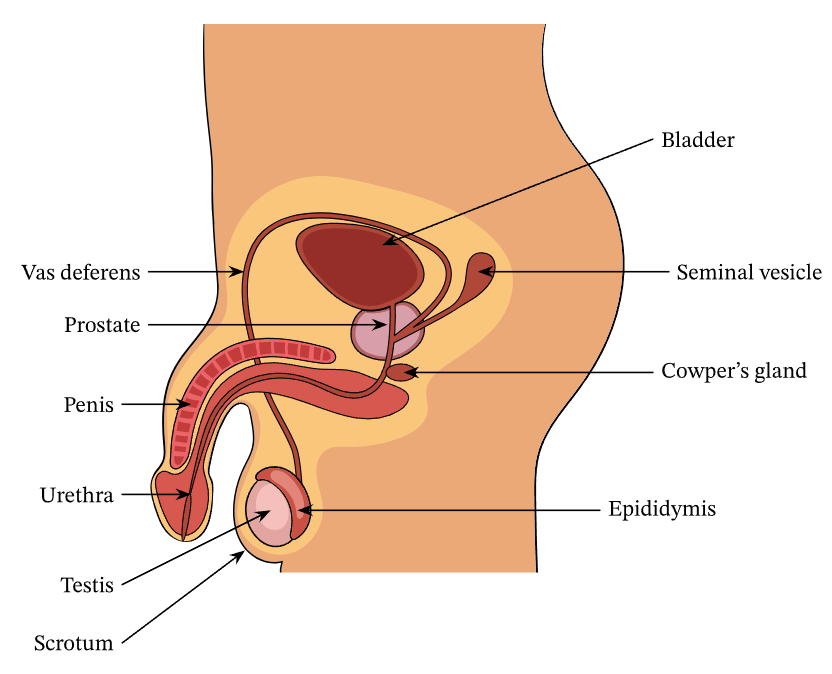
MALE REPRODUCTIVE ANATOMY
Sperms are produced in the testes (testicles) of the male, which are placed in sacs called scrotum. The epididymis stores the mature sperms and transports it via the vas deferens (sperm duct) to the urethra (inside the penis). Other glands like seminal vesicles, prostate, and Cowper’s gland help to produce the sticky alkaline milky fluid in which sperms swim (this liquid along with the sperms is called SEMEN). The semen is ejaculated through the urethra when the penis is erect.
Sperms are produced daily in a man’s body. During sperm production, also known as spermatogenesis, each testicle will produce about a few million sperm per day, meaning that every second that passes, 1500 sperm are born. A full cycle of spermatogenesis takes about 64 days
CAUSES OF MALE INFERTILITY
Male infertility can occur due to:
- Low sperm production (Low sperm count)
- Abnormal sperm function (Abnormal morphology or motility)
- Blockages that prevent sperm transport
- Ejaculation problems: Erectile dysfunction (difficulty getting and keeping an erection) or Premature ejaculation (ejaculating early during intercourse)
Causes of Low Sperm Count and Function:
Increasing age, poor diet, and lifestyle factors may all contribute to low sperm production and function. Mental and physical stress, inadequate sleep and exhaustion, sedentary habits, obesity, anxiety and/or depression, smoking and alcohol abuse, overuse of anabolic steroids, narcotic and recreational drug abuse, exposure to radiation/chemicals, and constant exposure to intense heat, are some known risk factors.
A poor diet with vitamin-mineral deficiency, and being high on processed and unhealthy foods, refined carbohydrates, and saturated/trans fats and low on natural food like green vegetables, fruits, omega3 fatty acids, other polyunsaturated fatty acids (PUFAs), and proteins, may also be a contributing factor.
DIAGNOSIS
It is important to simultaneously also evaluate for female infertility of the partner.
The initial diagnostic evaluation for male infertility is clinical where a physician evaluates in the following ways:
- General Physical Examination
- Clues for genetic predisposition or hormonal issues like reduced body hair and other male secondary sexual characteristics.
- Erection or ejaculation problems
- Psychological evaluation for low sex drive, stress, anxiety, depression, etc.
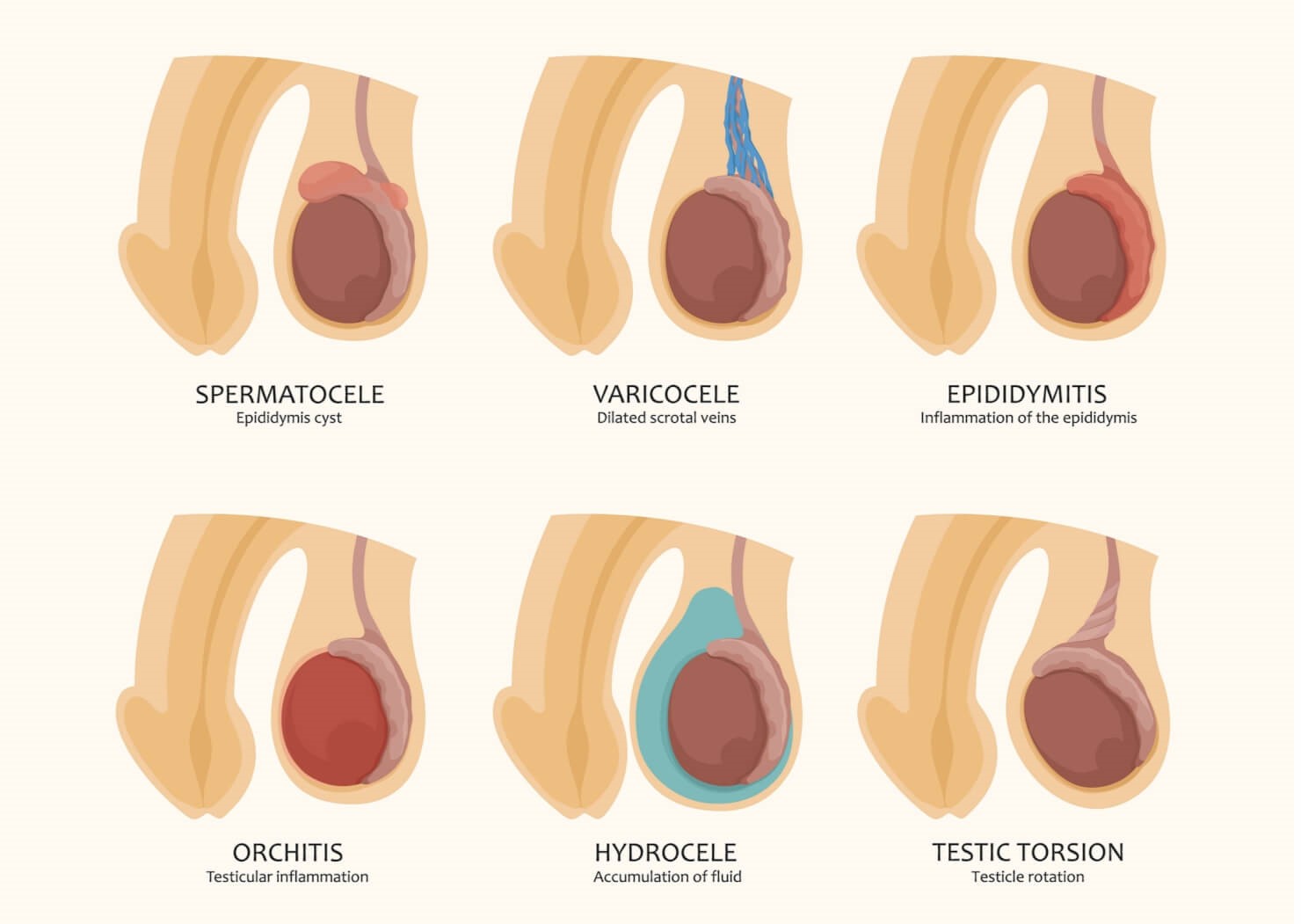
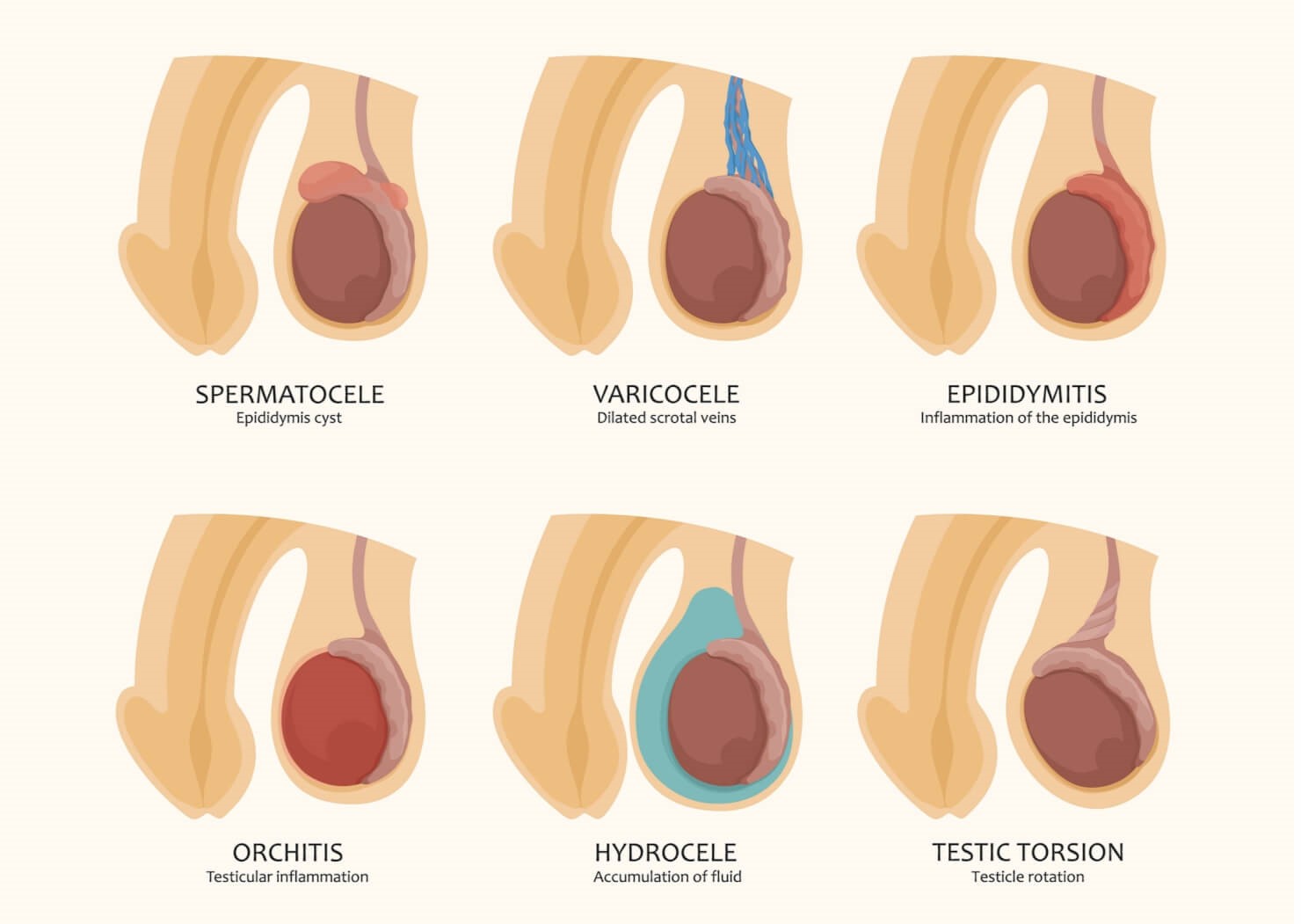
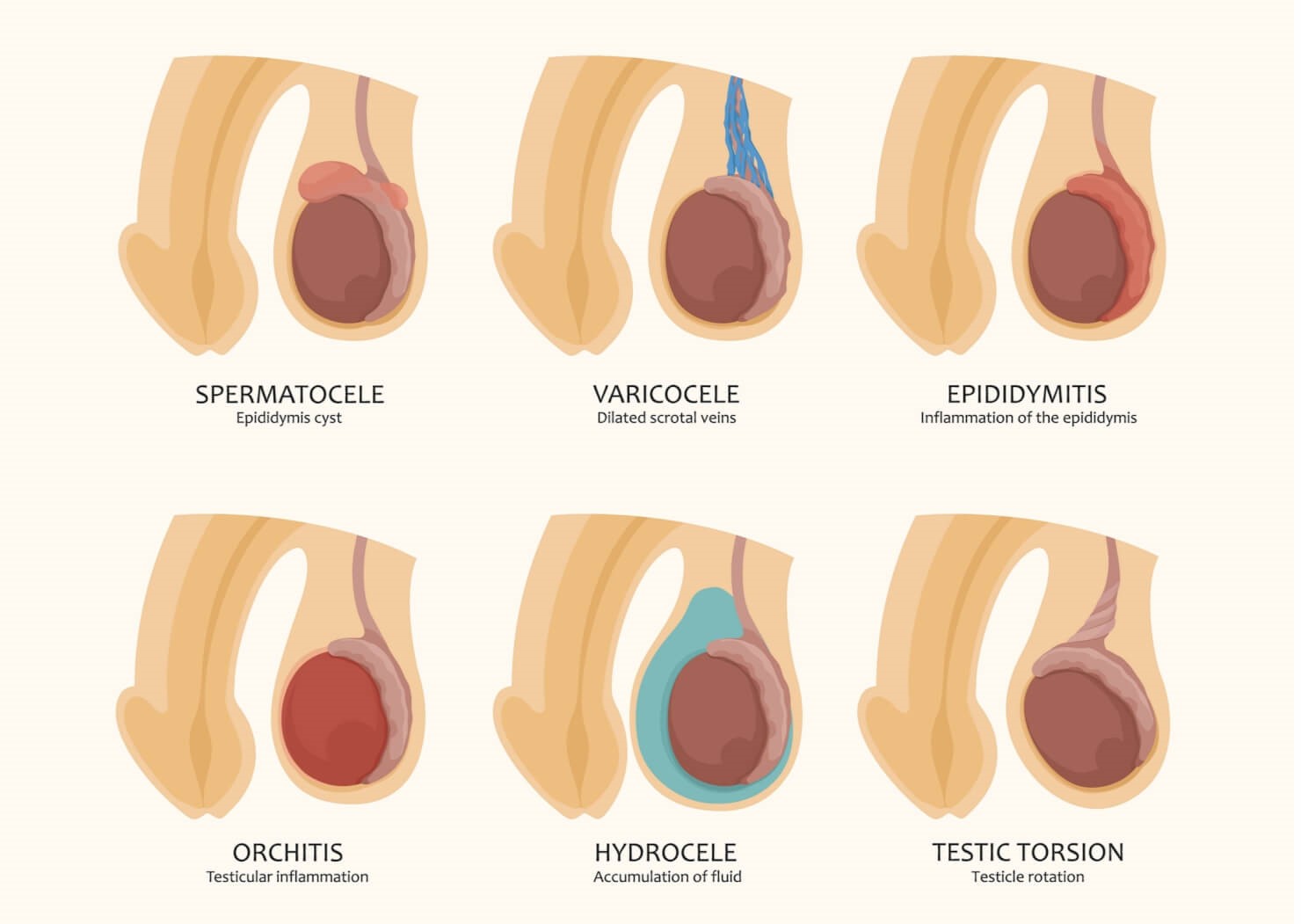
- Examination of testes, scrotum, and groin – Pain, discomfort, a lump or swelling in these areas can suggest other pathologies like inflammation of testes or epididymis (orchitis or epididymitis – due to mumps, STD – sexually transmitted diseases), hydrocele (fluid in the scrotum), varicocele (enlarged veins in the scrotum), torsion (testicle rotates, twisting the spermatic cord that brings blood to the scrotum), spermatocele (an abnormal sac/cyst in epididymis), hernia (protrusion of contents through a weak area), cancerous changes, or post-injury hematoma (blood collection due to bruising).
- History of testicle, prostate, groin, or penis injury or surgery
- Urinary problems
Thereafter, a semen analysis is recommended.
SEMEN-SPERM LAB ANALYSIS
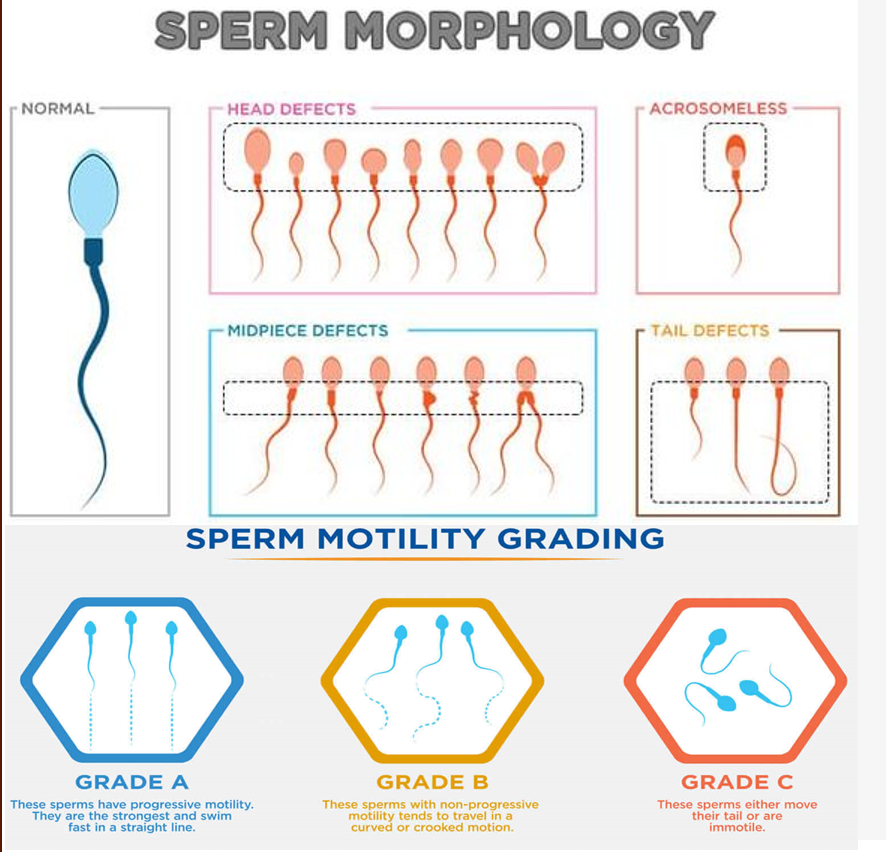
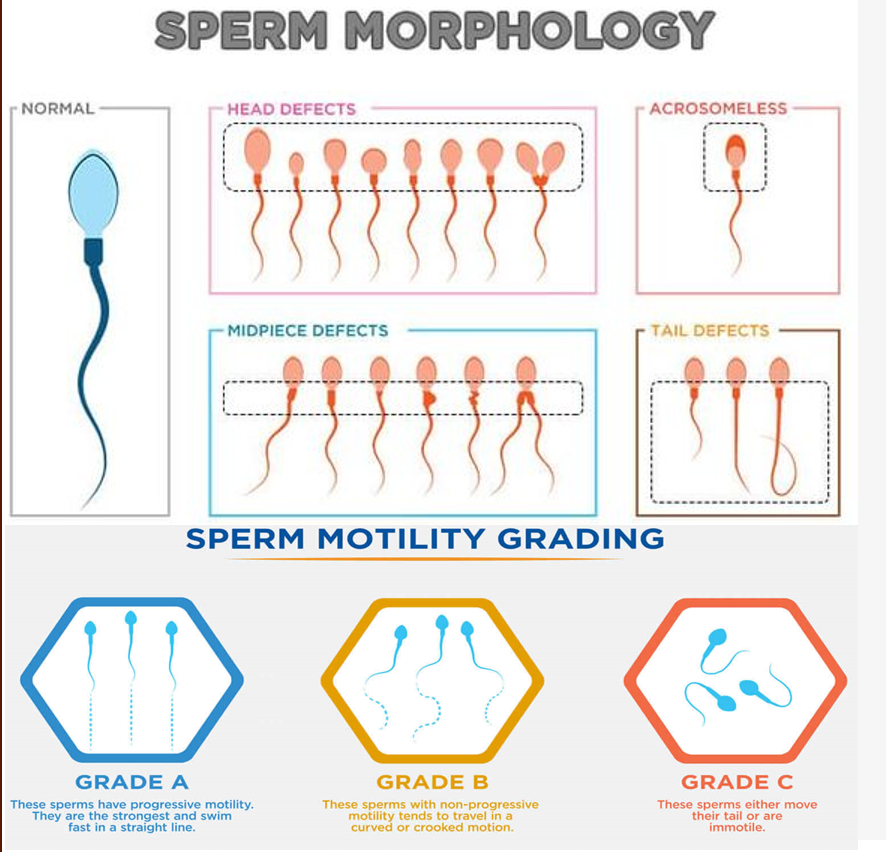
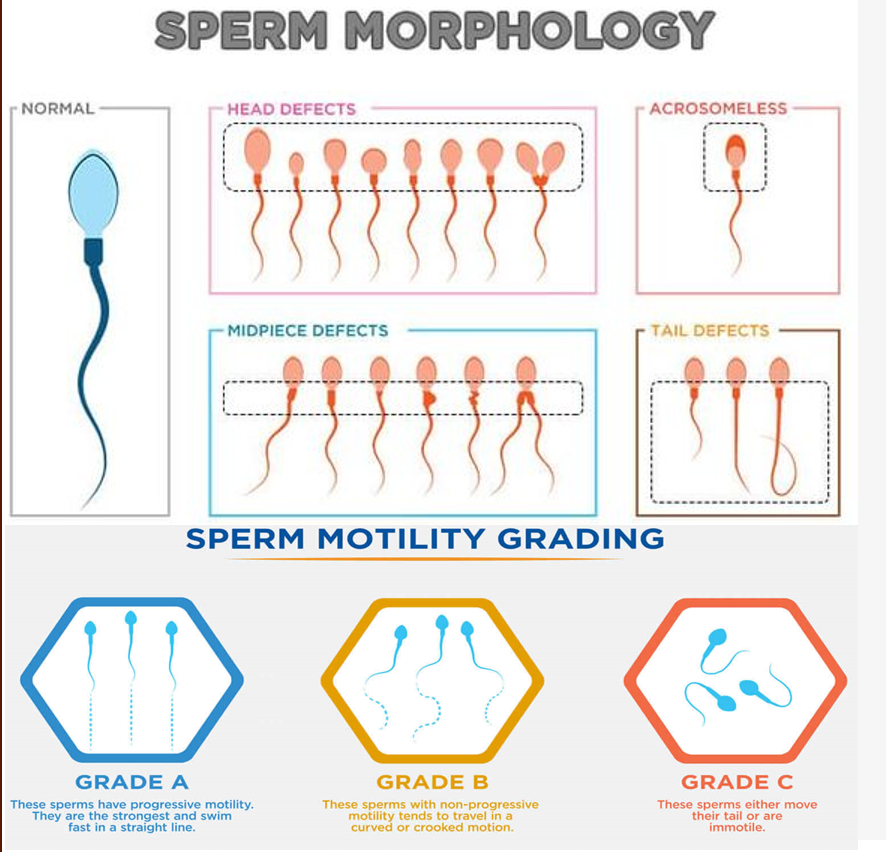
The analysis is done of sperm morphology (shape, size, structure) and motility (movement, swimming ability and characteristics).
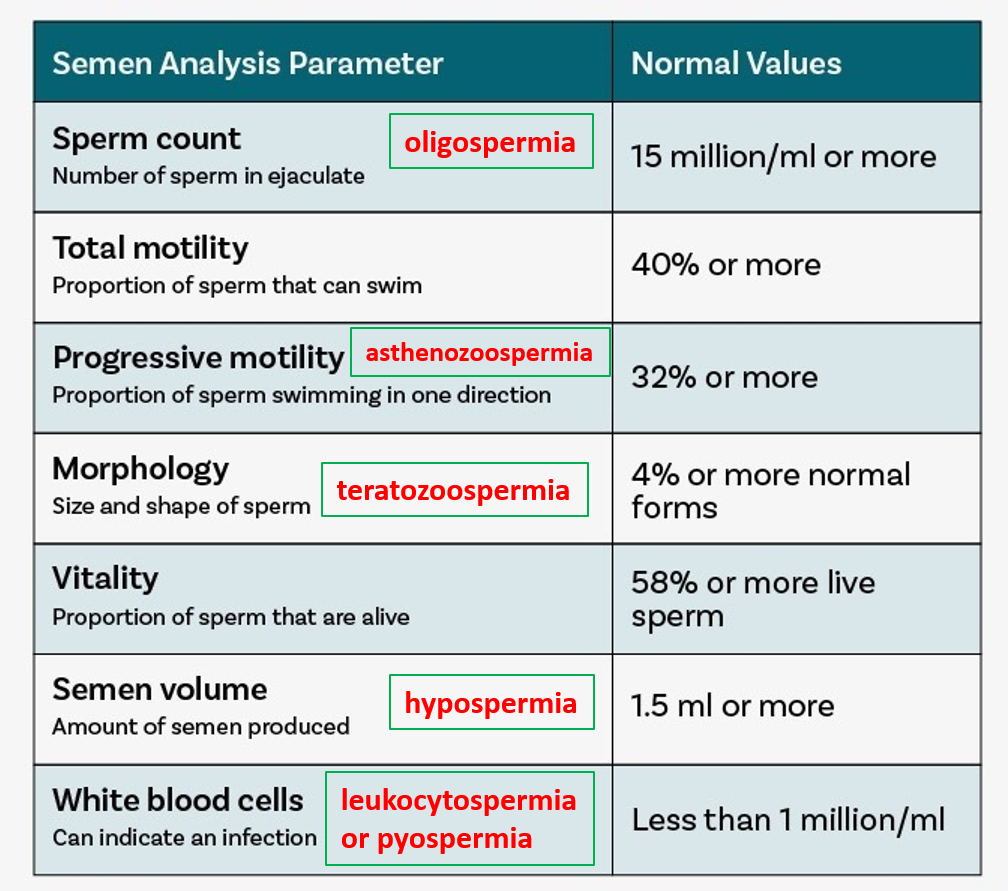
Oligospermia refers to low sperm count. Azoospermia is the medical term used when there are no sperm in the ejaculate. It can be “obstructive,” where there is a blockage preventing sperm from entering the ejaculate, or it can be “nonobstructive” when it is due to non-production of sperm by the testis.
Teratozoospermia is a condition in which a man has a high amount of abnormally shaped sperm. Every sperm count has a large percentage of abnormally shaped sperm present, but when this percentage is over 96% of the sample, it is known as teratozoospermia.
Asthenozoospermia is an infertility condition in men wherein a man produces sperms with low motility. Motility is the ability of the sperm to move forward swiftly and in a straight line. It is an essential requirement for natural conception.
Oligoasthenoteratozoospermia (OAT) is the term used when all the parameters like movement, sperm count and shape are abnormal. It can further be classified as mild, moderate and severe. The treatment and the prognosis are heavily dependent on the severity of the condition.
Necrozoospermia implies that the sperm in the sample are all dead. This condition is rare, and if it has sperms that are viable but are immotile. IVF and ICSI may help men with this condition to have a genetic baby. If the sperms are not viable, the fertility expert may attempt to remove immature and viable sperms through testicular biopsy to perform IVF or ICSI.
Aspermia is a condition where a man experiences dry orgasms or orgasms without releasing any semen. This may be the result of retrograde ejaculation, genetic disorders like cystic fibrosis or Klinefelter syndrome, hormonal imbalances or congenital abnormalities. This condition may affect male fertility.
Hypospermia implies that the total ejaculate is less than 1.5 ml. Retrograde ejaculation is the most common cause of this condition. However, it may also be caused by genetic disorders, hormonal imbalances or congenital abnormalities.
Leukocytospermia is when there are many white blood cells in the semen, and the condition is also called pyospermia. The white blood cells can cause damage to the sperm, decreasing fertility. The high amount of white blood cells can also mean that the man is dealing with some infection. It can also be the result of an autoimmune disease.
OTHER TESTS
Blood hormone levels: To check levels of testosterone, other androgens, and thyroid hormones (hyperthyroidism can reduce sperm count and function).
Urine test: Sperm in a urine sample taken after ejaculation can indicate if sperms are traveling backward into the bladder instead of out the penis during ejaculation (retrograde ejaculation).
Imaging tests: Scrotal or transrectal ultrasound
Genetic tests: To diagnose various congenital or inherited syndromes.
Testicular biopsy. This test involves removing samples from the testicle with a needle.
TREATMENT
One always begins with lifestyle solutions, and natural therapies and then moves on to hormones, drugs, and procedures as required.
Improving sexual productivity through more frequent intercourse, especially around the period of ovulation (like daily or alternate day), from 5 days before to after predicted ovulation in the middle of the cycle) will be advised. The avoidance of lubricants by the female may also help preserve the sperms better.
Diet should be rich in green vegetables, fruits, curd, PUFA, and whole grains, with adequate amounts of water. Avoidance of high-sugar items, and too much trans/saturated fat, alcohol, and refined carbs is beneficial. Adequate sleep, stress management, adequate physical exercise, quitting smoking, and intake of recreational drugs is important.
Natural or dietary supplements that have some scientific evidence of benefit, may be prescribed by many doctors to improve general health, improve sperm production and function, and reduce oxidative stress in the body. These include L-carnitine, coenzyme Q10, antioxidants like astaxanthin, lycopene, vitamin C, vitamin E, and minerals like selenium and zinc. Herbal supplements include maca root, shilajit, ginseng, ashwagandha, fenugreek, and saw palmetto, which may also be available as combinations, but still need more robust clinical evidence.
Psychological treatment may be needed if the evaluation reveals underlying stress, anxiety, or depression. In such cases, some relaxation techniques like breathing exercises, mindfulness, meditation, counseling, and psychotherapy (cognitive and behavioral therapy) may be advised and beneficial. Medicines for anxiety-depression may be given for some time.
Hormonal treatment with testosterone or other androgens is given if hormonal levels are abnormal on testing.
Treating any infection when seen or suspected, requires a course of appropriate antibiotics to be given to both partners.
Ejaculation problems like erectile dysfunction or premature ejaculation are treated with medicines like sildenafil or tadalafil.
Surgery is reserved for structural problems or specific conditions like hydrocoele, varicocele, hernia, torsion, obstructed vas deferens, reversing a prior vasectomy, etc., In cases where no sperm are present in the ejaculate, sperm can often be retrieved directly from the testicles or epididymis using sperm retrieval techniques.
Assisted reproductive technology (ART) involves obtaining the sperms (semen) from the male through normal ejaculation, sperm retrieval techniques, surgical extraction, or from donor individuals. The sperms are then inserted into the female genital tract, or used to perform in-vitro fertilization (IVF). IVF involves an egg being combined with sperm in vitro. The process involves monitoring and stimulating a woman’s ovulatory process, egg retrieval or removal from the ovarian follicles using a thin needle guided by ultrasound, and letting a man’s sperm fertilize the egg in a culture medium in a laboratory (test-tube baby) and then reimplanting the fertilized egg in the woman’s womb.
Alternate options include considering a sperm donor or adoption, if all other treatments do not work out.
Also read:
Urinary Tract Infection (UTI) – urethritis, cystitis, ureteritis, pyelonephritis


