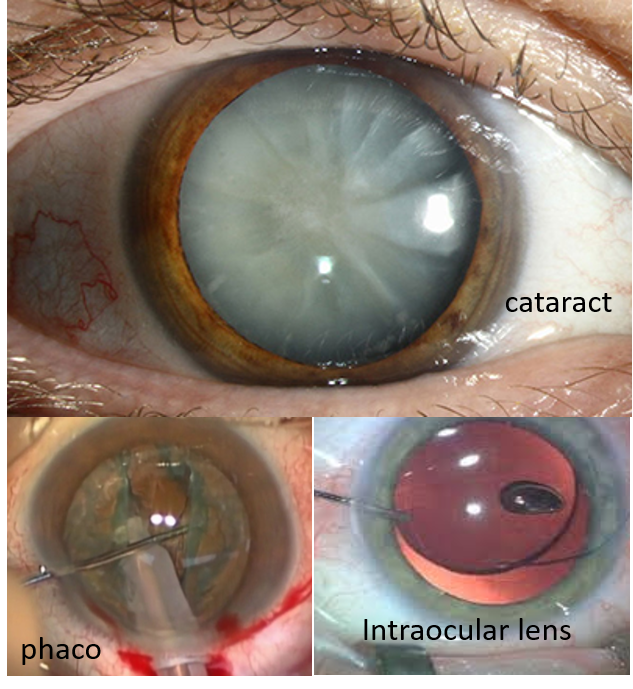
Cataract is the clouding of the lens due to aging and is the most common cause of a gradual decrease in vision in the elderly age group.
UNDERSTANDING LENS STRUCTURE AND CATARACT
The lens of the eye has 3 parts – a lens covering or capsule (the front part is called the anterior capsule, and the back part is called the posterior capsule), the cortex the peripheral softer part of the lens under the capsule, containing newer lens fibers, and the central nucleus, the hardest part, containing older denser lens fibers.
The lens is held in place with the help of ‘zonules’ that connect it to the ciliary body (that extends behind from the iris). The contraction of the zonules during viewing near objects helps the lens become more convex, increasing the converging power of the eye for better near focus. With increasing age, the zonules become rigid making viewing near objects difficult, and a need to wear reading glasses. This is called presbyopia.
In elderly people, the lens proteins and fibers degenerate and clump together, reducing lens transparency and making the lens appear cloudy. This is called cataract, and makes the vision blurred and hazy. Rarely, cataract can occur at a younger age due to the use of steroid medicines, diabetes, excessive smoking, radiation exposure, or sometimes after lens trauma.
CATARACT SURGERY TECHNIQUE
Cataract is treated only by surgical removal of the lens and placing a synthetic intraocular lens (IOL) in its place. Before the surgery, the power (number) of the IOL is calculated in diopters (D) via a corneal assessment (by a test called keratometry), and measuring the length of the eyeball by Ultrasound A-scan biometry. The IOL power is according to the postoperative distance vision correction.
In current practice, this is done by phacoemulsification where a small incision is made on the eye surface near or at the upper cornea, followed by a circular opening created on the anterior capsule through which the cataractous lens is broken down by an ultrasound probe, and removed through the small cut.
The intraocular lenses are flexible and sometimes even foldable, and have a central round part called the optic and two protrusions on either side called haptics. The IOLs used most commonly are posterior chamber IOLs (PCIOLs). These are inserted through the small cut and then the circular opening on the anterior capsule and placed on the posterior capsule of the lens by dialing in the haptics. Sometimes if the integrity of the posterior capsule is questionable, then the PCIOL may be placed on the remaining rim of the anterior capsule. Rarely the lens zonules are ruptured and both the anterior and posterior capsule may not be intact. Then an anterior chamber IOL (ACIOL) is used and placed on the iris.
Cataract surgery is a daycare procedure, and the person can go home after some observation period post-surgery. Usually, one eye is operated at a time. The use of a small incision and flexible foldable IOLs makes healing much faster. Antibiotic and anti-inflammatory eyedrops are given postoperatively for a few days.
Even though modern-day cataract surgery is fast and safe with great results, rarely complications can happen due to inadvertent surgical injury or patient predisposing factors. These can include bleeding in the eye, rupture of the posterior capsule, postoperative swelling of the cornea or retina, surgical incision leakage, rise in intraocular pressure (glaucoma), and eye infection or inflammation (uveitis). All these should be identified and treated timely by proper post-operative examination, recommended use of eye drops, and regular follow-up.
TYPES OF PCIOLs
A regular simple PCIOL made of polymethyl methacrylate (PMMA) has largely now been replaced with more flexible and foldable materials like acrylics (hydrophilic-water attracting or hydrophobic-water repelling). Hydrophilic acrylic lenses are made up of poly-HEMA (Hydroxy Ethyl Methacrylate) with water content in the range of 18-36%. These lenses need to be kept hydrated in the operation theatre till they are implanted and fold-unfold fast. The hydrophobic acrylic lenses are made up of PEMA, or PEA (Poly Ethyl Methacrylate or Phenyl Ethyl acrylate) and have a water content of 5% or less. They have a higher refractive index and lower edge thickness compared to hydrophilic lenses, fold-unfold slowly, are easier to handle when wet, with a temperature-dependent viscoelasticity.
Hydrophilic acrylic lenses are more flexible and easier to insert through very small incisions, while hydrophobic ones have more controlled and predictable unfolding as compared to hydrophilic lenses. Surgeons make their choice based on their skill-technique and experience.
Monofocal foldable IOLs correct only distance vision (reading glasses needed post-surgery). These include:
- Hydrophobic acrylic IOLs: Tecnis 1, Acrysof IQ, Seelens HP and Bunnylens HP, Vivinex and iSert, Optifelx Genesis and Eyecryl plus, Acriol, Aurovue and Supraphob. Tecnis Eyhance is a modified (next generation) hydrophobic acrylic monofocal IOL with higher order anterior aspheric design, which can extend the range of vision to intermediate in addition to distance vision.
- Hydrophilic Acrylic IOLs: Akreos AO, CT Asphina, RayOne-RAO600C/ C flex, Seelens AF and Bunnylens AF, Eyecryl plus clear and Acryfold and NAspro
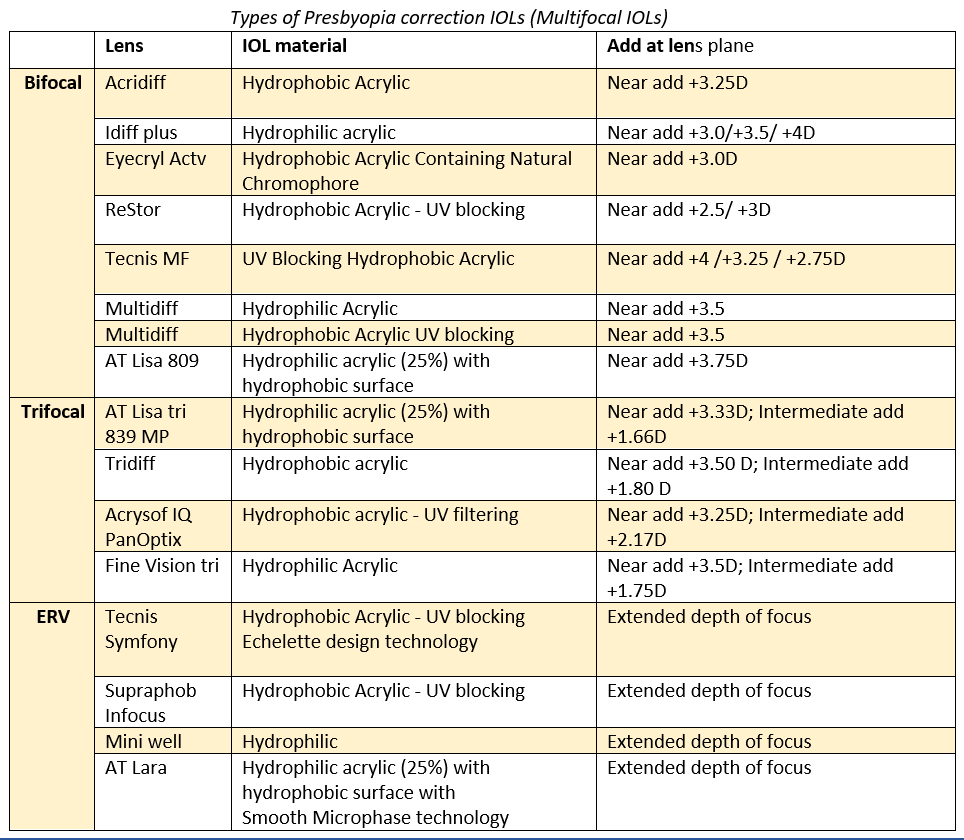
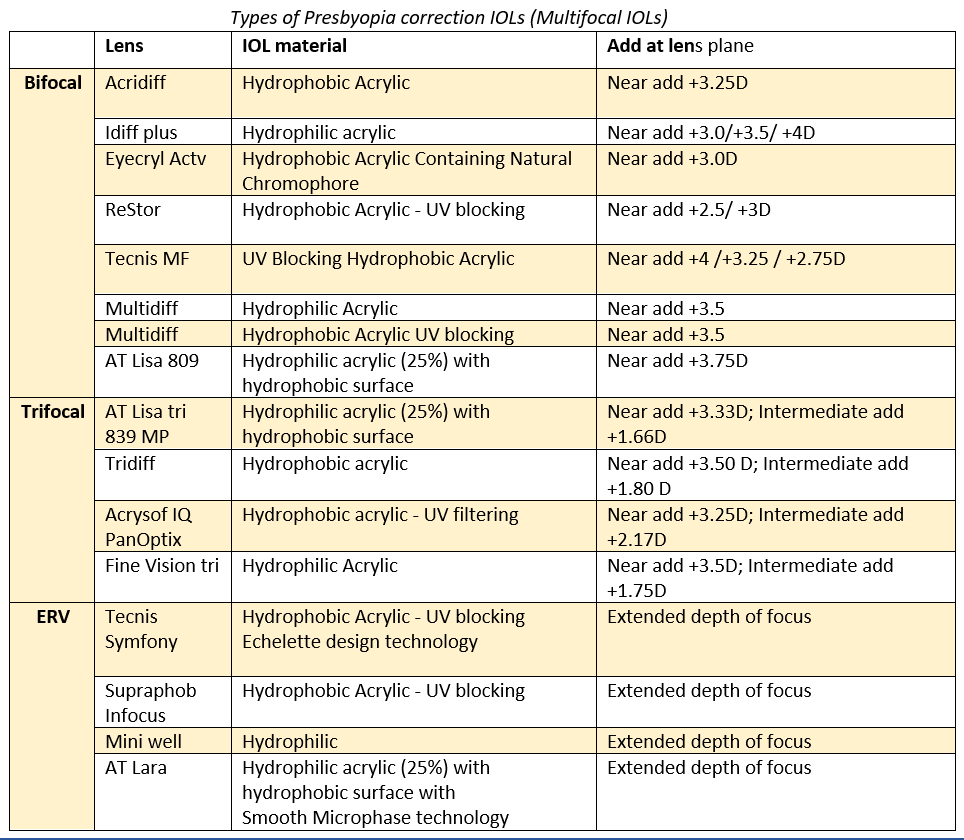
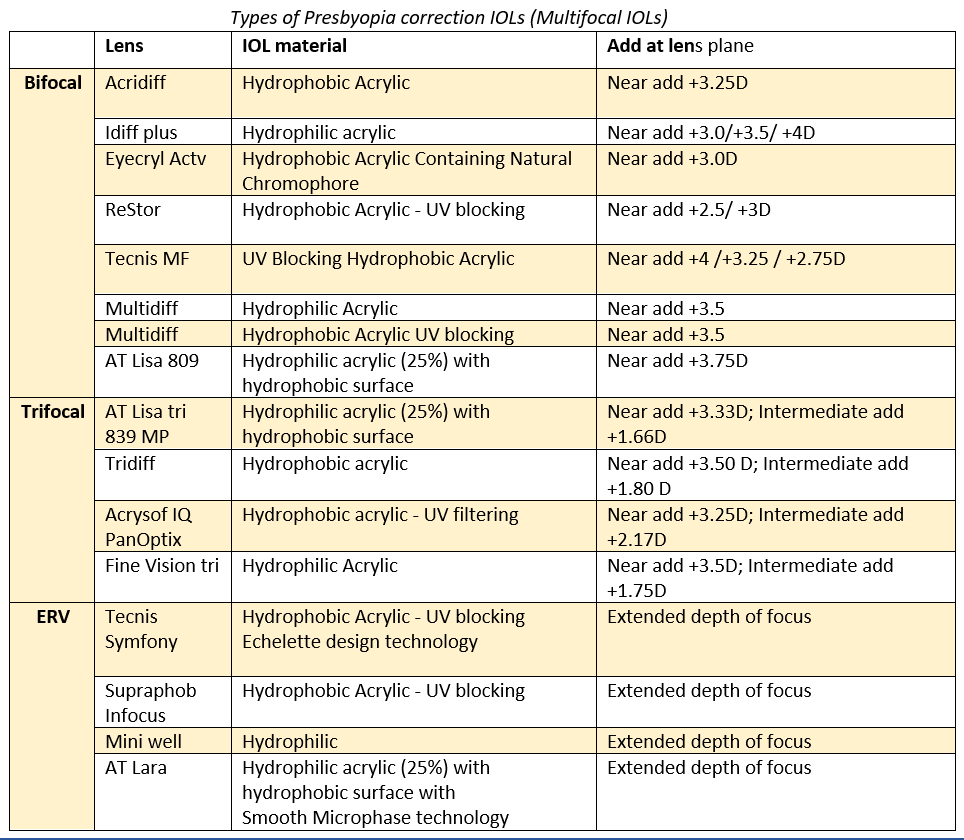
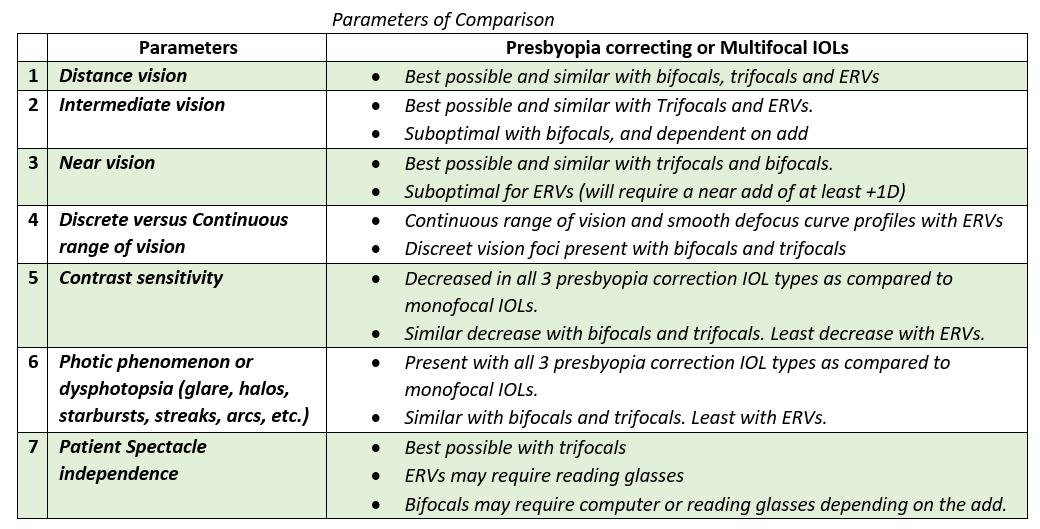
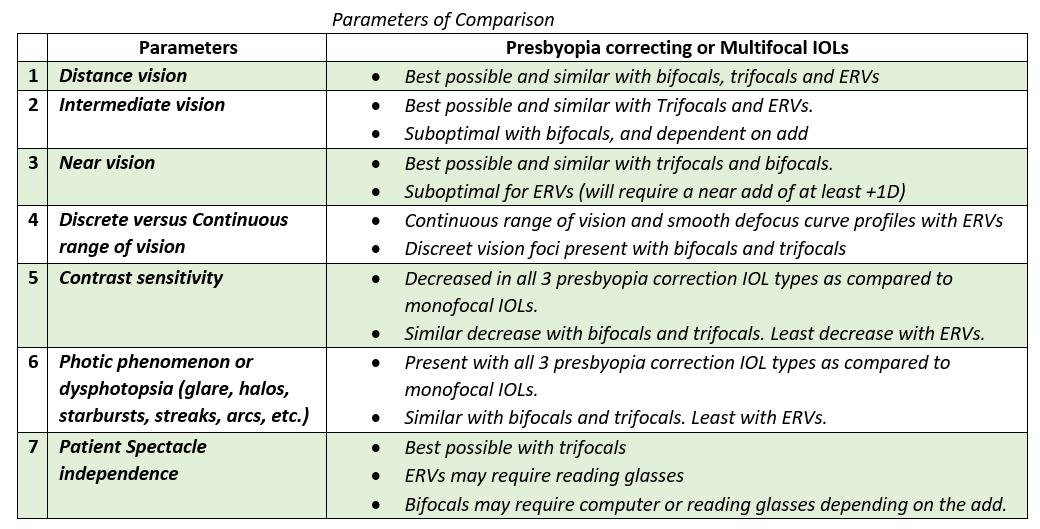
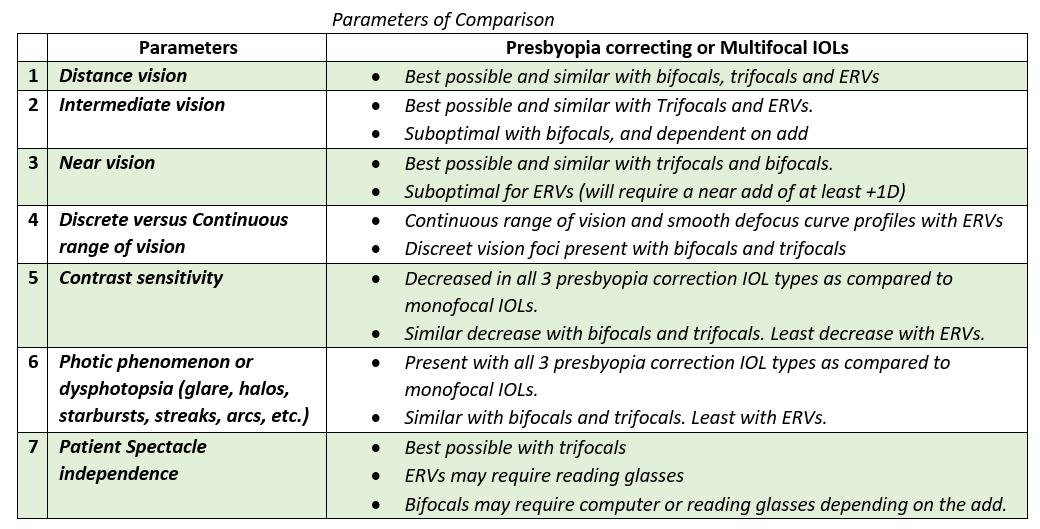
Multifocal IOLs (Presbyopia correction IOLs)
Now IOLs are available that can cover both distance and intermediate/near distances to enable a spectacle-free existence. These are called Multifocal IOLs (MFIOLs -include Bifocal, Trifocal, and Extended Range of Vision ERV IOLs) or Presbyopia correcting IOLs, as they omit the need for reading glasses due to presbyopia.
Presbyopia Correction lenses as an option should be offered to and discussed with all patients undergoing cataract surgery, as they give both good visual acuity (visual quality) and convenience.
- Bifocal IOLs refract or diffract (or both) light from an object simultaneously to the far and near foci of vision, and part of this light disperses. They may be pupil-independent with a fixed distribution of light between the near and distance zones (Tecnis MF) or pupil-dependent with light distribution based on pupil size with more light distribution to the near zone during pupillary constriction (Acrysof ReStor). Pupil-dependent Bifocal IOLs can make reading in dim light harder but help to reduce glare and halos at night, while Pupil-independent Bifocal IOLs can make it more difficult to read in bright light when the pupil is more constricted.
- Trifocal IOLs have three focal points with additional intermediate focus providing superior quality of vision for intermediate activities.
- The extended range of vision (ERV) IOL, also called EDOF (Extended Depth of Focus IOL), is based on a new optical technology where elongation of the focus is due to the constructive interference of light, and enhanced phase and interaction of light emerging from each and all zones occurring over a range of distances. This is achieved by the echelette design (spacing of rings, and height differential within each ring). The proprietary achromatic diffractive technology corrects the corneal chromatic aberration and decreases loss in contrast sensitivity.
Also read:
Vision Reduction and Loss – Understanding Causes and Points for Timely Action

