Urinary problems are often called as ‘bladder problems’ or ‘prostatism’. The appropriate term for these problems is ‘lower urinary tract symptoms (LUTS)’ since these can be caused by problems of any part of LUT, be it bladder, urethra, prostate, nerve supply, muscles and support system. LUTS are very common and the incidence is progressively higher as the age advances, particularly beyond 45-50 years of age.
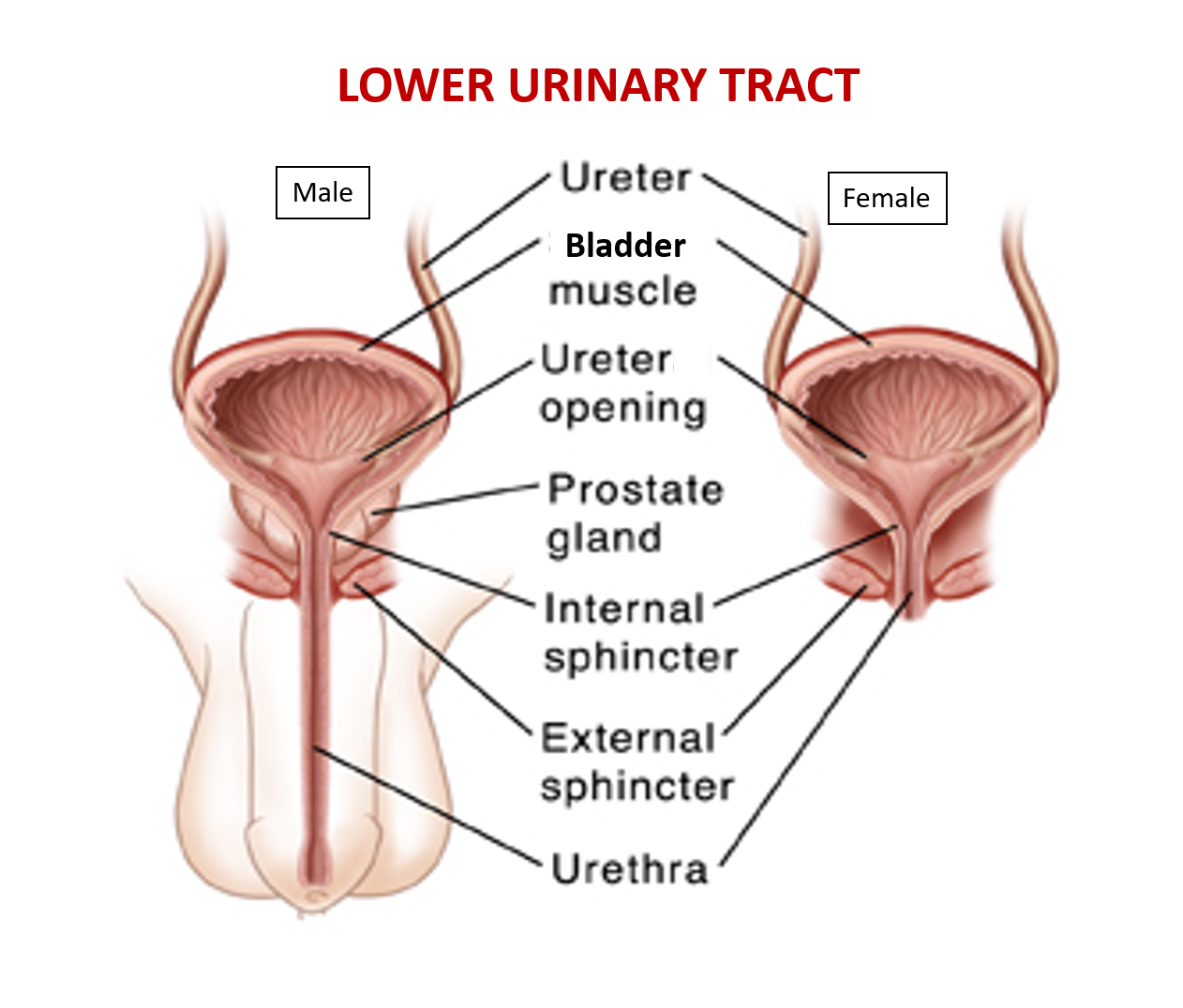
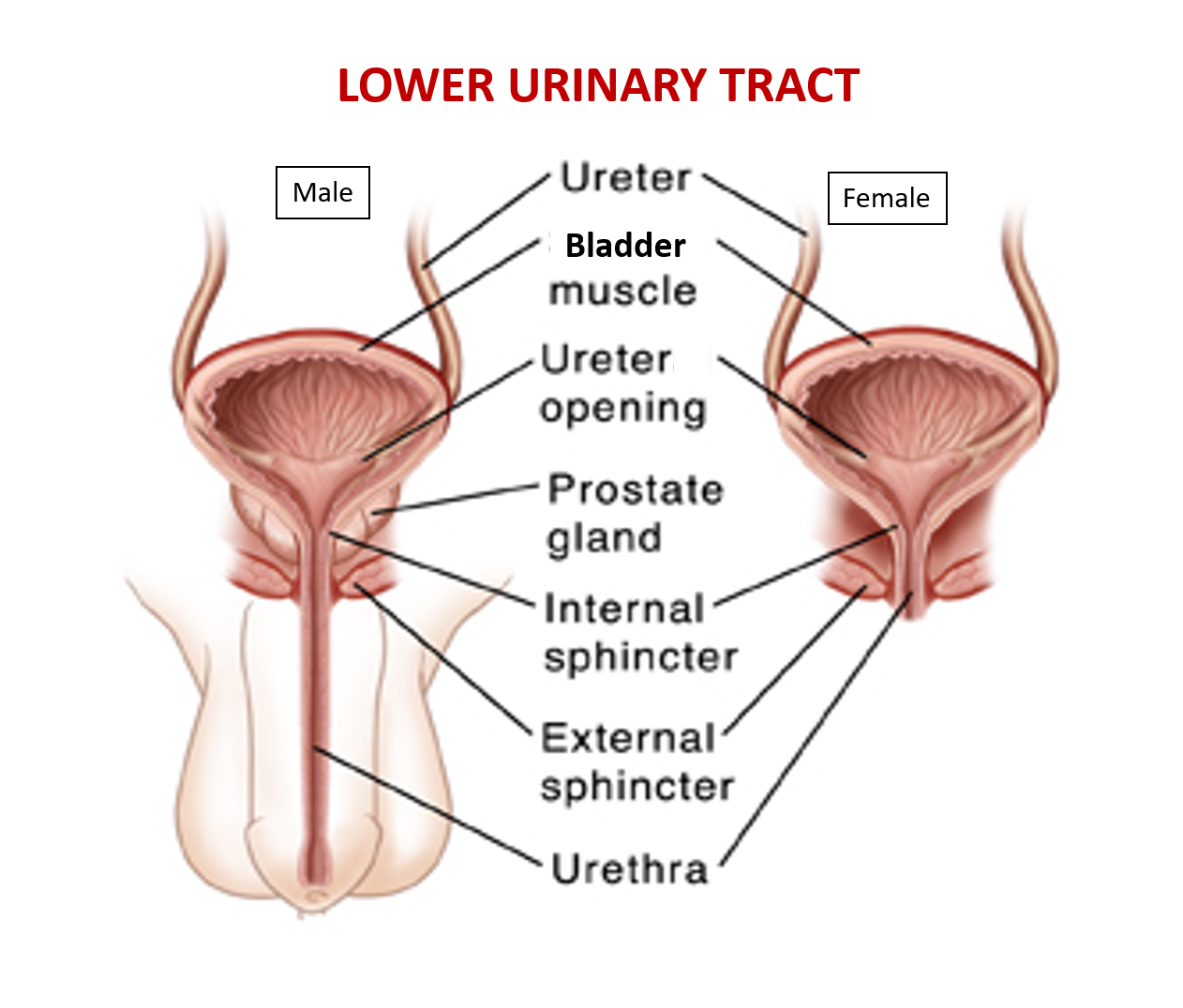
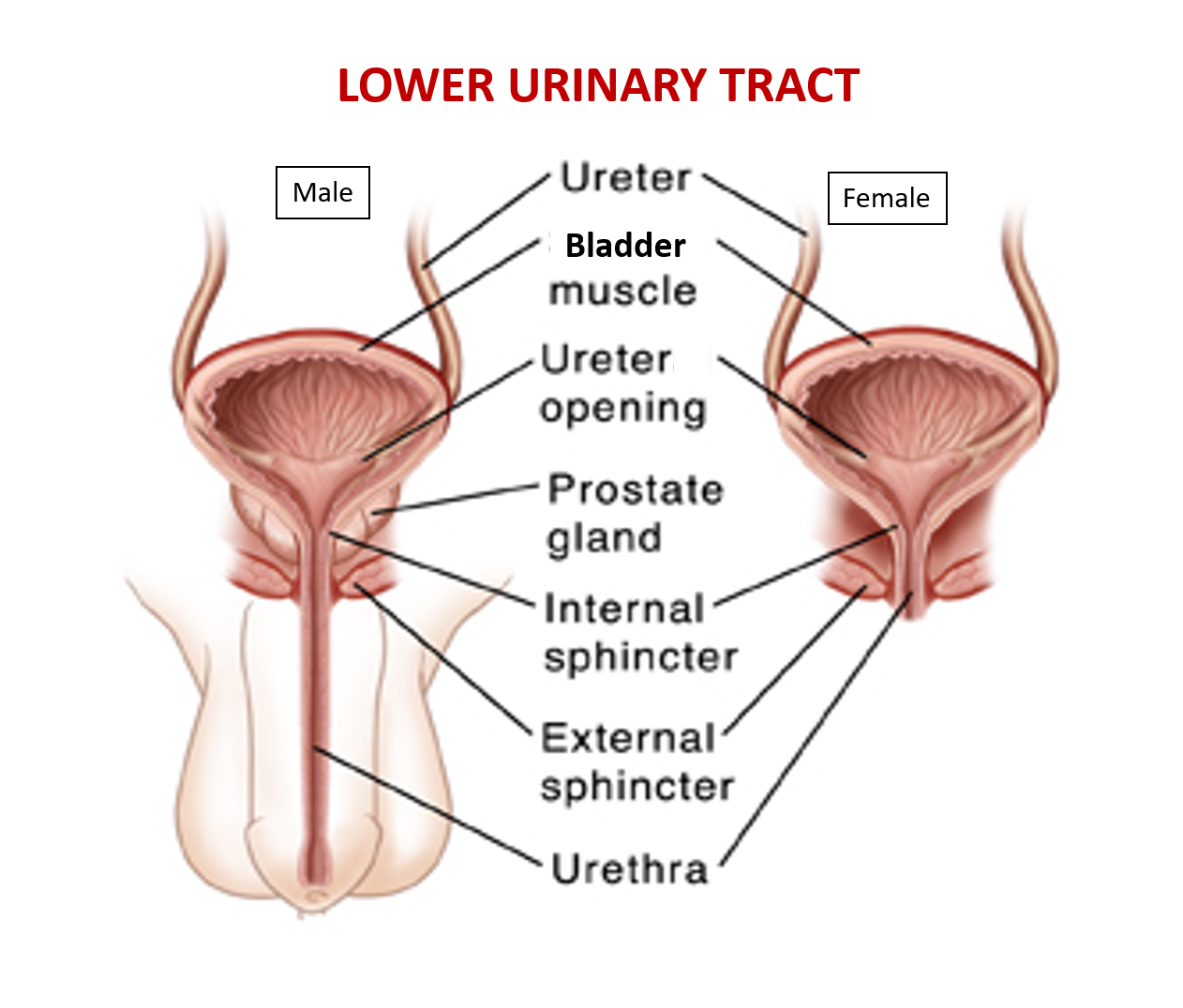
WHAT CONSTITUTES LOWER URINARY TRACT (LUT)?
The LUT comprises of the urinary bladder (muscular sac for urine storage) and urethra (tubing for the passing of urine). In males, a walnut-size organ called the prostate surrounds the urethra just beneath the bladder. In both genders, the deepest 3-4 cm of the urethra is surrounded by muscles (called sphincters) that regulate the passage of urine. The internal sphincter is present at the bladder neck and the external sphincter is beneath the prostate in men, and lower 2-3cm of the urethra in women. A complex network of nerves supplies the whole urinary tract and helps the brain control function of LUT.
HOW DOES THE LUT FUNCTION?
Simplistically function of the LUT can be understood in terms of that of a water tank and tap. It is divided into the following two phases –
- Storage phase – when the urine is collecting in the bladder, the bladder muscles remain relaxed enabling urine to collect with ease and the urethral muscles (sphincters) remain contracted (in a squeezed state) maintaining a closed outlet for preventing leakage of urine.
- Voiding phase – when it’s time to pass urine, the urethral muscles become relaxed to let the urine pass with ease while bladder muscles contract to squeeze the urine out to completion.
WHAT ARE THE LUT PROBLEMS/SYMPTOMS?
LUTS are broadly categorized into two –
A. Storage problems occur when the storage capacity of the bladder is reduced either due to a problem in the bladder (e.g. infection, bladder muscle irritation) or due to damage /malfunction of sphincters. Various symptoms of bladder storage problems include
- Frequency or urinating much more often
- Urgency or a sudden urge to urinate which is difficult to control
- Bladder /Urethral pain on trying to hold urine
- Nocturia which is having to wake up at night to pass urine several times
- Incontinence (uncontrollable leakage of urine). It is of the following types:
- Urge incontinence – This occurs due to ‘urgency’ because of involuntary bladder muscle contraction often associated with overactive bladder (OAB). This may happen due to abdominal trauma, infection, nerve damage, some medications, and certain fluids like alcohol/caffeine, etc.
- Stress incontinence – This occurs due to increased abdominal pressure during lifting heavy-weight, sneezing, coughing, laughing or straining, along with a weak sphincter and pelvic floor muscles. This is seen post childbirth trauma, menopause, and surgery. (It is not due to ‘mental stress’),
- Overflow incontinence – This occurs due to overfilled bladder and the inability to empty it completely while urinating (imagine if you continue to pour water in a pot after filling to brim!). This may happen with an increase in urine volume in conditions like diabetes or the use of diuretic medicines, due to an obstruction in the bladder or of the urethra (bladder outflow obstruction BOO), or because of weak bladder muscles or nerve damage.
B. Voiding problems occur when the passage of urine becomes difficult either due to weak bladder muscle (for example due to neve-related problems, diabetes) or due to spasm in sphincter muscles, or other causes of blockage of the urethra like prostate enlargement, urethral narrowing (stricture). Various symptoms of voiding problems include
- Hesitancy or difficulty in initiating urine stream
- Poor stream or slow flow speed of urine
- Intermittency which is a stop-start type of stream of urine
- Straining for urination
- Sensation of incomplete voiding
Causes of LUTS
- Structural problems
- Prostate enlargement: men over 45 years of age frequently suffer from urinary blockade from enlargement of the prostate gland, as due to age-related and hormonal changes, the prostate gland tends to swell in size. Men, whose father or uncles have had prostate enlargement, have a higher tendency to develop it.
- Urethral stricture: Structural narrowing of the urethra due to fibrosis (scarring) is a frequent occurrence in men of all ages. Strictures can form out of urethral infection (sexually transmitted diseases-STD), injury to the urethra (accidents/injuries/fractures), urethral instrumentation (catheter placement for urinary retention, urethral surgery for enlarged prostate, etc.), cancer, or sometimes for unknown reasons. Strictures also occur in women, though infrequently.
- Prolapse of internal organs: In women, with advancing age, multiple pregnancies and childbirth, pelvic floor support (muscles, ligaments, nerve supply supporting the uterus/bladder/bowel) progressively weakens. Moreover, with obesity the pressure in the abdomen is higher due to fat deposition. This strain and weakening leads to problems of urinary leakage and prolapse of pelvic organs (e.g. bladder and uterus drop).
- Functional problems
- Neurological (problems of nerve supply): The function of the urinary tract is completely under the control of the brain via the spinal cord through nerves. Therefore, problems with neurological structure, function and blood supply like seen in cases of Parkinson’s disease, Alzheimer’s disease, dementia, multiple sclerosis, tumors, compression, trauma, surgeries, diabetes and stroke, can cause a variety of LUT problems.
- Non-neurological – LUTS can also be due to weakness or spasms of the sphincter that can occur without damage/blockade of nerve supply in both men and women. These include:
- Weakness of sphincters, leading to leakage of urine while coughing, sneezing, squatting, or in severe cases, even walking (called stress incontinence), is common in women who have had vaginal deliveries, particularly those who are overweight. In men, sphincter weakness happens predominantly after prostate surgery for cancer (called post-prostatectomy incontinence).
- Bladder neck obstruction is the result of a persistent spasm of the internal sphincter muscle
- Dysfunctional voiding is due to external sphincter spasm.
- Prostate-related LUTS may be due to both gland enlargement as well as spasms of prostatic muscles.
- Bladder sensitivity may be altered as the bladder can become hyposensitive (not feeling the presence of urine) or overactive during filling of urine giving rise to urgency and leakage (urge incontinence), or underactive during voiding (causing difficulty in passing urine).
HOW ARE LUT PROBLEMS DIAGNOSED?
Your doctor would take a careful history of your urinary symptoms and medical problems, do a detailed examination of your lower abdomen, as well as decide to check neurological reflexes. The investigations recommended and performed include commonly an Ultrasound of urinary tract, routine urine and blood tests and a test for checking the speed of flow of your urine (Uroflowmetry). At times you may be asked to keep a record of your liquid intake and urination for 2 – 7 days.
Uroflometer is a small machine that is used to record the flow of urine. It is kept beneath a container into which one passes urine. The result is given in the form of a graph of flow rate against the volume of urine passed, and some numerical parameters, to help decipher the basic problem and initiate the treatment.
If the diagnosis is still uncertain or, more commonly, the patient has not optimally responded to initial treatment, further evaluation with invasive investigations like urodynamic study or certain x-ray studies (urethrography, cystography) may be advised to pinpoint the problem area.
Urodynamic study is a computerized invasive study done with small tubes placed into the urethra and rectum and patches placed to measuring pressures, electrical activity of muscles and urine flow rates which are depicted graphically and numerically.
HOW ARE LUT PROBLEMS TREATED?
Fortunately, a large majority of LUT problems can be managed by conservative methods, like pelvic floor exercises, diet modification and medications.
- Pelvic floor exercises (“Kegel’s exercises”) – the patient is trained to squeeze and relax his / her pelvic floor muscles (the muscles used to “stop urine” or “stop flatus” from coming out) multiple times a day. These exercises strengthen the muscles as well as improve neuronal connections between brain and LUT. It is helpful in urinary leakage, urinary urgency and difficulty in passing urine due to external sphincter spasm.
- Diet and lifestyle modification – since LUT and rectum are supported by the same group of pelvic floor muscles and supplied by the same group of nerves, problems of the rectum (e.g. constipation) may worsen LUT problems and vice versa. Therefore, it is advised to increase fiber intake in diet (water, fruits, salads). Patients with leakage of urine, urgency and bladder pain may feel better by decreasing/avoiding caffeinated beverages (e.g. coffee, tea, and cola) and spices in food. Patient is asked to reduce weight by diet and exercises.
- Medications – there are several groups of medications available in the market each designed to address a different set of problems like medicines to decrease irritability of bladder by improving urgency, medicines to relax the sphincter and prostate to improve the flow of urine, etc. Needless to say, one must not do self-medication for LUT problems and must always consult a qualified specialist.
A minority of patients need invasive management, the type of procedure depending on the diagnosis –
- Prostate surgery – with technical advancements (e.g. HD/4K visualization systems, plasma-kinetic and laser systems for cutting the prostate) most of the time prostate removal surgery can be performed endoscopically obviating the need for cutting open the abdomen. Name of two popular procedures are bipolar TURP, HOLEP laser surgery
- Surgery for incontinence – for women with stress incontinence, pelvic floor support procedures known as mid-urethral sling, are performed. Currently, these procedures are minimally invasive, requiring only a small cut inside the vagina (half inch or less) with/without tiny stabs (2-3mm) in the groin area. These can be typically performed as day-care or short admission procedures. For men and women with urge incontinence, a day-care procedure is done with Botox® (also used to get rid of wrinkles) injected into bladder wall endoscopically through the urinary passage to relax the irritated bladder muscle. Rarely, a pacemaker may have to be implanted into the nerve supply of LUT (called sacral neuromodulation) for resistant cases of urge incontinence, or other procedures like artificial urinary sphincter placement, or augmentation cystoplasty in which a segment of intestine is fashioned into a cup and stitched to the bladder in patients with very small bladders, performed in resistant cases.
HOW DOES ONE KEEP THE LOWER URINARY TRACT HEALTHY?
- Drink plenty of liquids, so that the color of your urine is almost like water. Dark-colored urine is not healthy and is a sign of dehydration. For an average person mostly working indoors, approximately 2 – 2.5 liters of liquids is sufficient. (caution – consult your doctor if there are fluid restrictions due to medical conditions)
- Avoid drinking excessive caffeinated beverages such as cola, coffee, tea, etc. Caffeine tends to irritate bladder lining and muscle, and therefore one may feel urgency for urination.
- Do Kegel’s exercises (sequentially squeezing and relaxing the pelvic floor muscles) to maintain good muscle tone and responsiveness
- Keep genitalia clean. Women should wash their genital area well while taking bath at least once daily, and wipe the area with clean tissue/towel from front to back after urinating. Men should wash the penis from outside as well as inside (i.e. retract the foreskin fully) at least once daily and wipe the front part with clean tissue/towel after urinating.
- Sexual hygiene should be maintained. Both men and women should clean genitals before having intercourse to decrease the number of bacteria. Urinating after intercourse to flush out the bacteria which may have entered, is also recommended.
- Avoid constipation by increasing fiber in diet (salads, fruits), taking enough fluids and exercising regularly.
- Take time to empty your bladder as completely as possible. Relax your muscle and do not strain while passing urine.
In case you have any Urinary problems or symptoms, consult a qualified medical practitioner.
Dr. Mayank Mohan Agarwal, is a urological surgeon working as Associate Director in the Department of Urology & Kidney transplant surgery at Medanta Hospital, Lucknow. He has special interest in treatment of incontinence and prolapse in women (female urology), urological cancer surgery (uro-oncology) and laser and minimally invasive surgery (laser and laparoscopy). After his superspecialty training (MCh) from prestigious PGIMER, Chandigarh, he received, through awarded fellowships, training in uro-oncology and uro-gynecology from Memorial Sloan Kettering Cancer Center, New York and University of California, Los Angeles, respectively. He worked as Associate Professor at his alma mater PGIMER, Chandigarh before moving to private sector. He is also an avid academician and researcher with several research publications, book chapters and a book to his credit. He is Associate Editor of the international research journal – BMC Urology.
Also read –
Urinary Tract Infection (UTI) – urethritis, cystitis, ureteritis, pyelonephritis