WHAT IS PAIN AND WHY DOES IT OCCUR
Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue injury or damage. Therefore, pain is a sensation that intimates some ongoing injury or damage at or around the site where the pain is felt.
Pain may be acute (sudden onset, short-term; lasts under 2 weeks), or chronic (onset over a period of time, long-lasting with periods of exacerbation). Sometimes the pain may be felt at a site away from the actual site of tissue damage. This occurs due to the distribution of nerves and is called referred pain.
The injury or damage to a particular tissue or organ leading to pain may be due to:
- injury – physical injury, chemical/radiation injury
- lack of proper functioning leading to build up of metabolites, gases or toxins
- infection
- lack of proper blood supply
- mechanical obstruction, blockage, or compression
- wear and tear due to age, high physical activity, incorrect posture
- degeneration or lack of nutrition
Fibromyalgia is a disorder of altered processing and amplification of pain sensations and signals. It is characterized by chronic widespread and severe pain in muscles and joints along with fatigue, sleep disturbance, and effects on memory and mood.
MECHANISM OF PAIN
Understanding the mechanism of any medical problem helps in its effective coping, and management as well as reassurance on the rationale of the medicines and therapy prescribed. The mechanism of pain has two important components
- Inflammation
- Nerve transmission
INFLAMMATION
Any kind of tissue injury or damage due to the causes stated above leads to the development of inflammation. Damage to the membranes of cells releases substances called phospholipids that are converted to inflammatory mediators called prostaglandins (PGs) and leukotrienes with the help of enzymes called cyclooxygenase (COX) and lipoxygenase (LOX).
Other inflammatory mediators include cytokines (small messenger proteins) and free radicals (reactive oxygen species -ROS). These are released by the white blood cells (WBCs) that come to the site of injury due to the dilation of blood cells. This also leads to swelling and redness at the injured site.
NERVE TRANSMISSION
The first step involves the stimulation of nociceptive receptors (for example – the TRPV group of receptors) at the site of inflammation. The inflammatory mediators like prostaglandins, free radicals, etc., as well as damaged or infected tissue parts, cause activation of the nociceptive receptors leading to the formation of an electrical impulse or action potential.
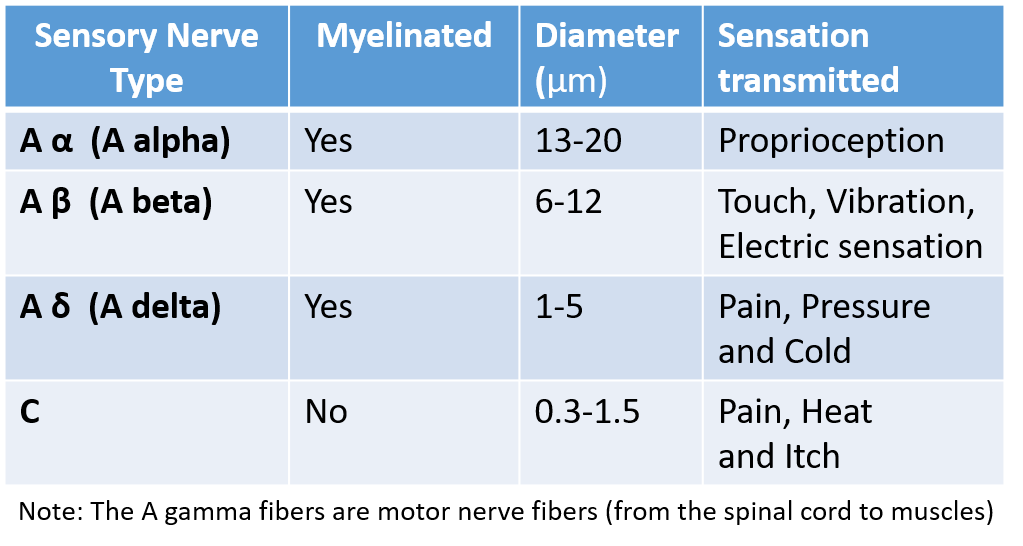
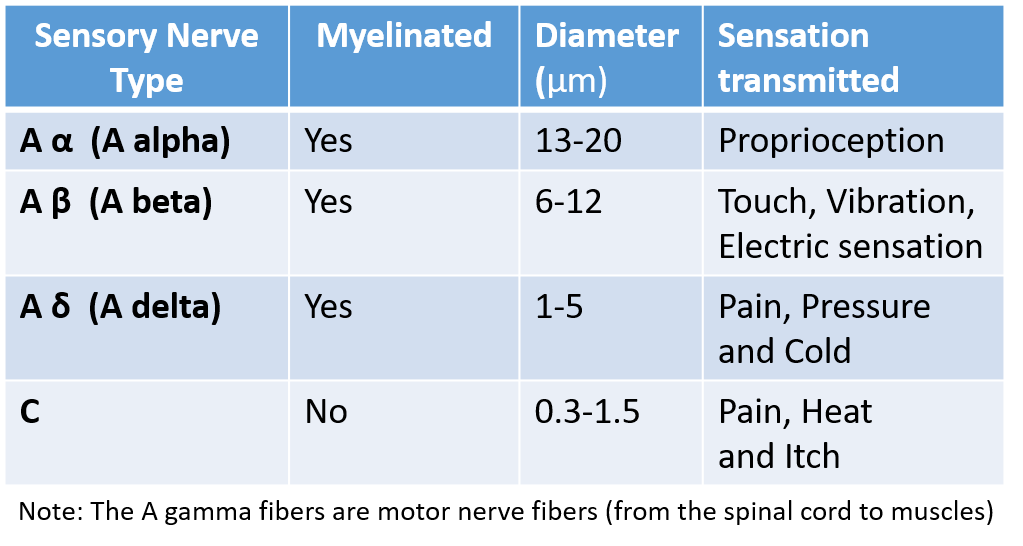
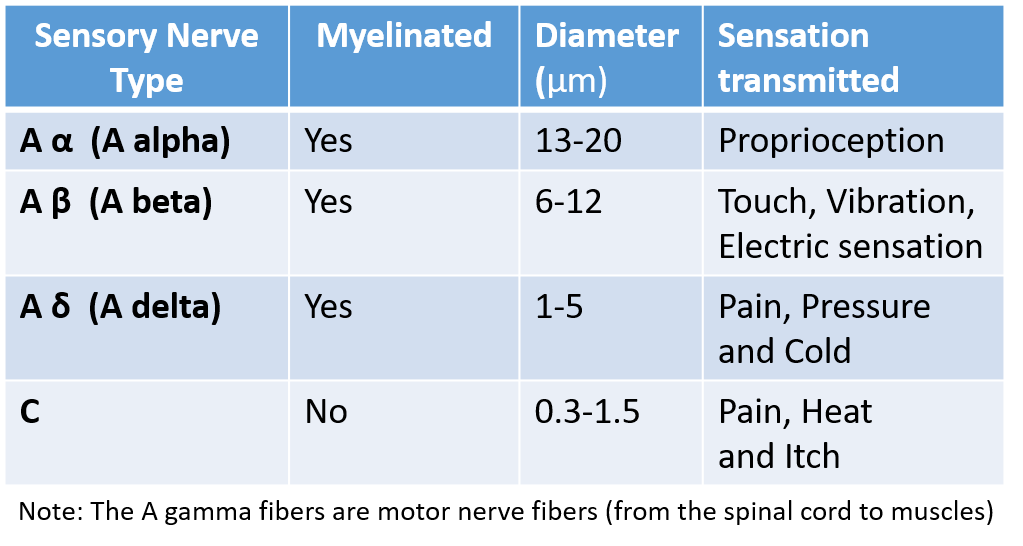
The next step is the transmission of this electric impulse (pain sensation) to the spinal cord through the peripheral sensory nerves. A nerve is a bundle of nerve cells called neurons. Peripheral sensory nerves are of different types as shown below.
The A fibers are larger and myelinated (covered by the myelin sheath) with regular interruptions for the electrical impulse to jump and travel much faster. The C fibers are not myelinated therefore transmission through them is slow. A delta and C fibers carry pain sensation from the nociceptive receptors at the site of injury to the appropriate level of the spinal cord.
From the spinal cord, ascending pathways carry the pain sensation to the brain, and also amplify and increase pain sensation.
The thalamus is the major junction and relay center in the brain. Here there are also projections from the limbic system (the emotional center of the brain). The sensations finally reach the cortex (the conscious and thinking brain), where the pain is perceived, interpreted, and analyzed to initiate action/response.
Therefore, the pain finally perceived is a combination of the sensation itself coupled with emotions like fear, anxiety, etc.
From the brain, there are descending pathways that project to various levels of the spinal cord and are inhibitory to pain thereby reducing pain perception. Therefore, pain perception can be modified and reduced by thoughts, emotional control, training, experience, and sleep.
Neurotransmitters are chemicals in the junction of neurons in the nerves that transmit the electric impulse from one neuron to the other in the nerve. These neurotransmitters can be excitatory (amplify the impulse) or inhibitory (suppress the impulse).
Glutamate is the most common excitatory neurotransmitter for pain sensation across peripheral sensory nerves and ascending pathways, while substance P is also an excitatory neurotransmitter at nociceptive receptors and C fibers. Both these amplify the electrical impulse as it reaches the spinal cord, and then to the brain. Descending pathways have inhibitory neurotransmitters like serotonin, noradrenaline, or GABA, that reduce pain transmission and perception.
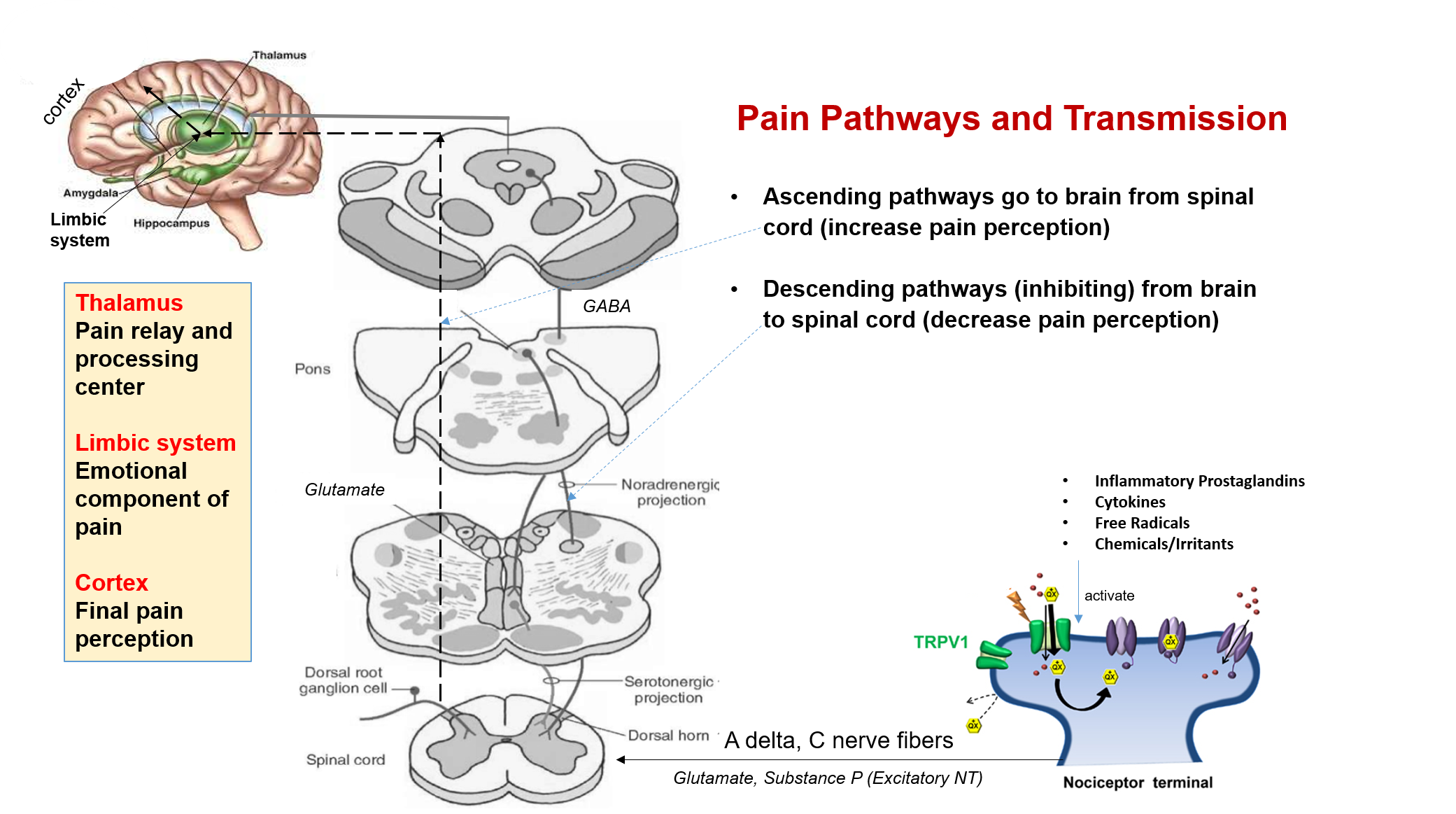
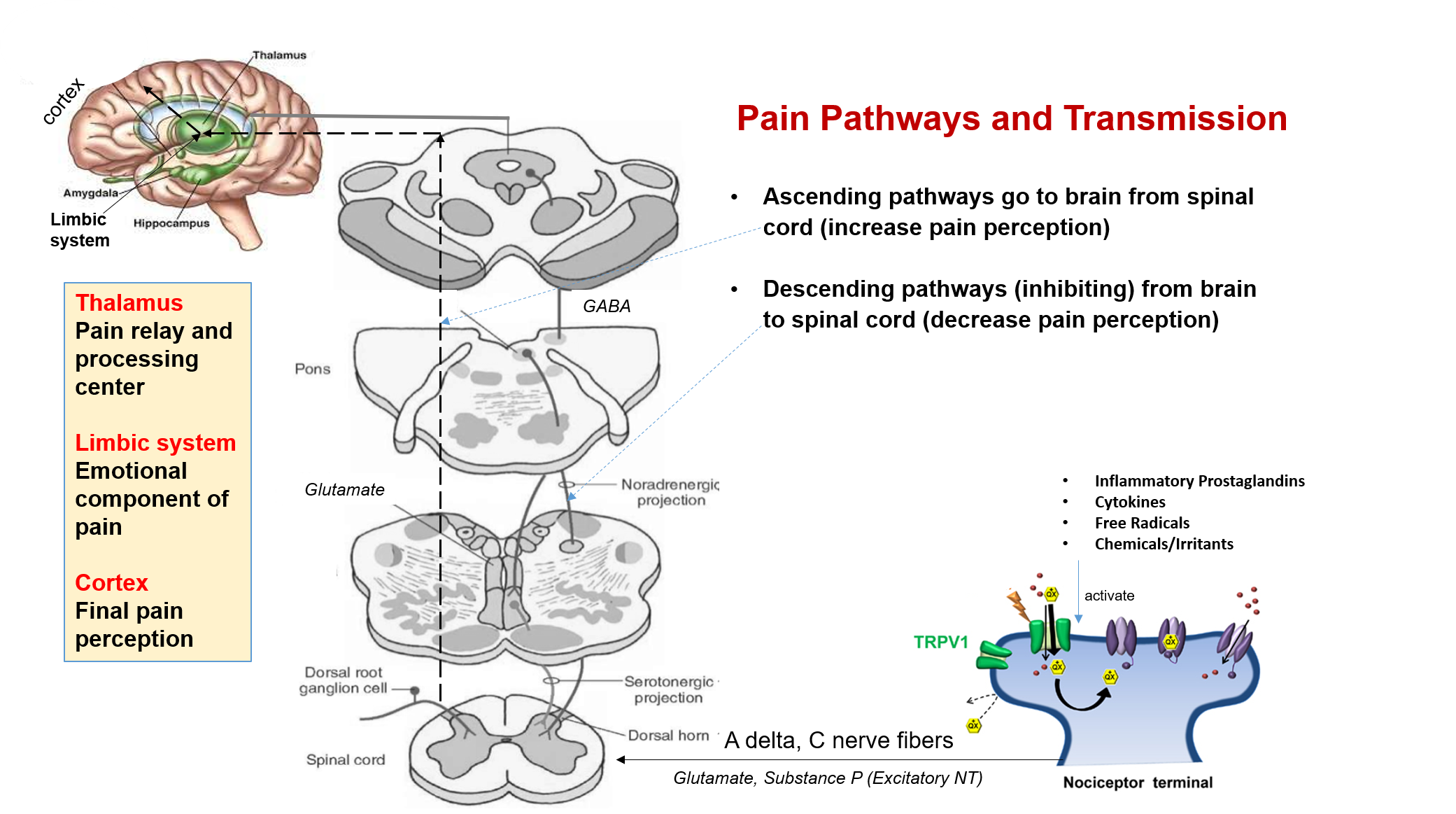
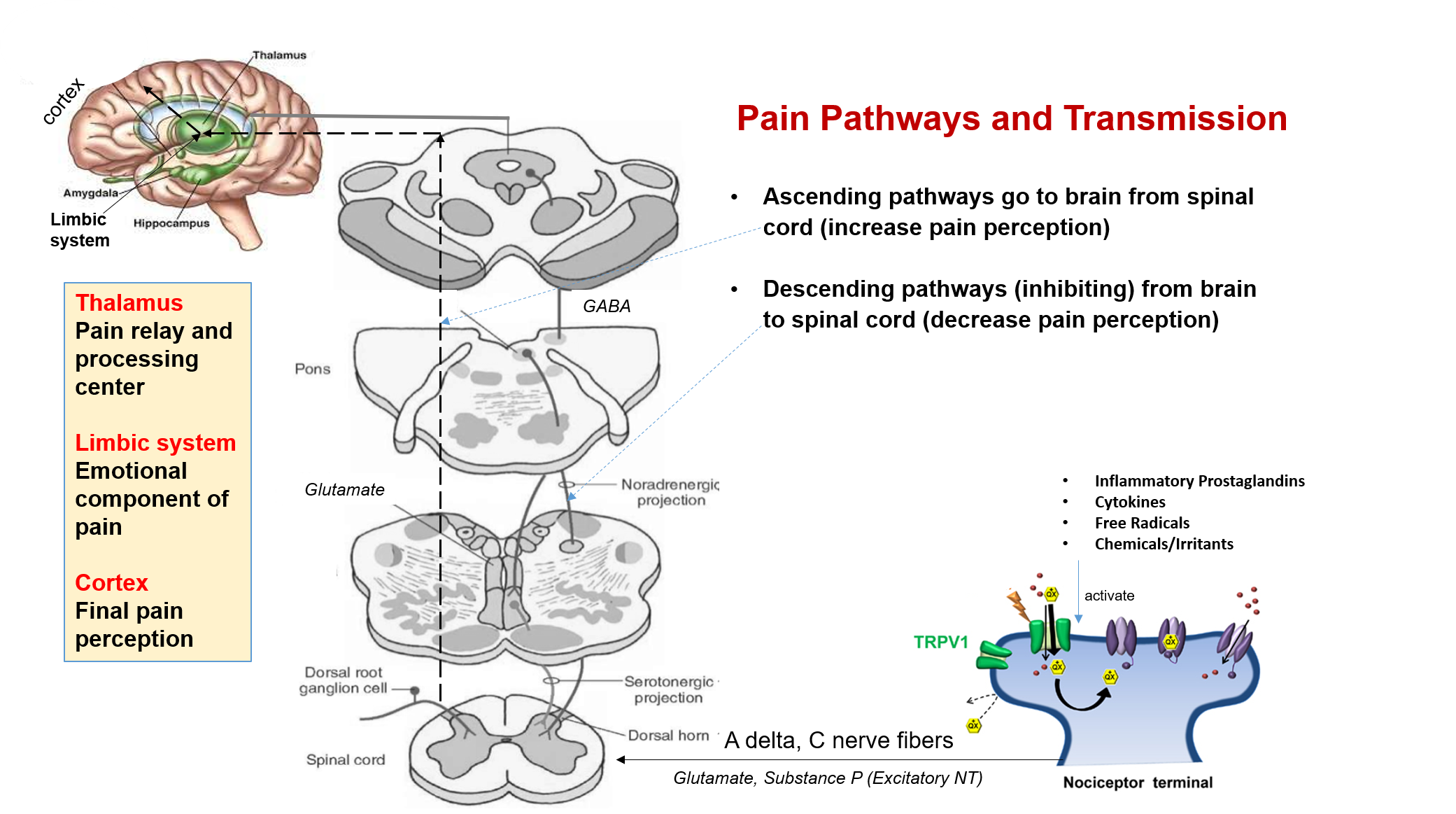
In all these nerve pathways of pain transmission and perception, multiple pain receptors (like TRPV nociceptors, opioid receptors, other G protein receptors, and cannabinoid receptors), along with neurotransmitters (excitatory/inhibitory) are involved. These are the targets of medicines used in pain management.
Medicines that reduce inflammation and inflammatory mediators at the site of injury, also reduce pain.
PAIN EVALUATION
It is difficult to evaluate pain objectively and quantify it. So, the pain is assessed and monitored qualitatively through pain rating scales, like the one shown below.
While there are many modalities for pain management, it is of prime importance that the underlying cause is diagnosed and treated. For fibromyalgia, the symptomatology and management are centered around pain relief, as no underlying cause is found.
MEDICINES FOR PAIN
Medicines that reduce pain are called analgesics, and sometimes painkillers in common terms. Most of them are available as oral tablets, and some are also available as injections.
Paracetamol
This is a medicine that acts at the level of the brain through multiple mechanisms. Some of these include inhibition of prostaglandins produced in the brain (centrally acting PGs) and activation of descending pathways, as well as possibly influencing some cannabinoid receptors. Paracetamol (also called acetaminophen) is the first-line medicine for all kinds of acute pain and fever. However, it does not have anti-inflammatory action, for which it is often combined with NSAIDs.
NSAIDs
Nonsteroidal anti-inflammatory drugs (NSAIDs) act by inhibiting the COX enzyme, thereby reducing the production of prostaglandins, which are one of the main inflammatory mediators, at the site of injury. Therefore, NSAIDs mainly act by reducing inflammation and thereby decreasing the stimulation of nociceptor receptors by inflammatory mediators.
The most commonly prescribed NSAIDs include ibuprofen, diclofenac, aceclofenac, naproxen, mefenamic acid, piroxicam, etoricoxib, nimesulide, and ketorolac. Gastrointestinal disturbance especially acidity is the most common side effect for which acid-suppressant drugs, are often co-prescribed.
Opioids
This is a class of strong analgesics and is reserved only for severe pain non-responsive to NSAIDs, and for palliative care. These are to be taken only under medical prescription, supervision, and dose monitoring, as these can produce physical and psychological dependence, as well as tolerance, and so have the potential for addiction and abuse. These can also produce significant side effects like sedation, constipation, visual and psychological disturbance, and in high doses respiratory depression.
Opioids act through different kinds of receptors. The main opioid receptors identified are δ (delta-opioid receptor DOR, DOP or OP1), κ (kappa-opioid receptor KOR, KOP or OP2), and µ (mu-opioid receptor MOR, MOP or OP3).
The body has its own natural endogenous opioids that act through these receptors. Most well-known are the endorphins, enkephalins, and dynorphins that act through mu, delta, and kappa receptors respectively. Endorphins help relieve pain, reduce stress, and improve the sense of well-being, acting like the body’s ‘feel-good’ chemicals. Opioid medicines (exogenous opioids) also potentiate the action of these endogenous opioids.
The most commonly used opioid drugs are tramadol and tapentadol which act mainly through the mu receptors. In addition, they also increase levels of neurotransmitters like serotonin and noradrenaline which further adds to their pain inhibition properties. These drugs are often combined with NSAIDs. They are first-line opioid medicines with lower dependence and side effects.
Opioids like morphine, pethidine, codeine, meperidine, oxymorphone, oxycodone, fentanyl, and methadone, act mainly via MOP and to some extent through the other opioid receptors also. Pentazocine acts mainly through KOP, while buprenorphine has a partial action on MOP. These drugs all have significant side effects, dependence, and abuse potential therefore appropriate medical usage is of prime importance.
GABAergic drugs
Gabapentinoids are derivatives of GABA and therefore mimic its inhibitory neurotransmitter action. The drugs in this class include pregabalin and gabapentin. They are useful in pain management especially in pain due to nerve inflammation (neuropathies and neuralgia), as well as to treat conditions like anxiety disorders, bipolar disorder, epilepsy, fibromyalgia, and sometimes even migraine, and insomnia. Some of the common side effects include drowsiness, dizziness, fatigue, blurring, confusion, euphoria, vivid dreams, tremors, dry mouth, and indigestion.
Benzodiazepines act by increasing the action of GABA and therefore are sometimes used as adjuncts in pain management, especially if associated with significant anxiety and lack of sleep. This class includes medicines like diazepam, alprazolam, and clonazepam. However, the risk of tolerance and dependence should be evaluated and these medicines prescribed judiciously and appropriately for a short duration.
Cannabinoids
This is a class that has acquired a lot of interest recently. Cannabinoids are derived from the plant Cannabis sativa, and consist of substances that act on the body’s cannabinoid receptors (like CBD1 and CBD2) as well as other G protein receptors and TRPV nociceptive receptors that modulate pain. Our body also has endogenous cannabinoids that act through these receptors.
Cannabinoids from Cannabis sativa (also called phytocannabinoids or exocannabinoids) include CBD (cannabidiol – most studied), CBN (cannabinol), CBG (cannabigerol), THC (tetrahydrocannabinol) and terpenes. These act by desensitizing nociceptive receptors, decreasing pain transmission, increasing descending pathways, decreasing anxiety and stress associated with pain, and also potentiating the action of endogenous cannabinoids.
There are a number of legalities and regulations regarding the medical use of Cannabis that vary from country to country, therefore the same should be checked for one’s own country. In some countries like India, Cannabis is used in folklore (Vijaya leaf – bhang), and cannabinoids derived from Cannabis leaf extract and its use in seed oil are approved as herbal medicine. However, using the flower or buds is not permitted under the Narcotics Act. In the USA, medical cannabis use has been legalized in some states, however, it should be derived from the Hemp plant where the amount of THC (responsible for psychotropic effects) is much lower.
CBD oil is available in many countries and is prescribed for moderate to severe pain. Its oral dose should be gradually increased with close monitoring and titration by a physician. Cannabis leaf extract in preparations in seed oil are also commercially available. There is still ongoing research, while more evidence and regulatory clarity are awaited on using cannabis medically in pain management.
Antidepressants
These drugs may sometimes be added to enhance response to pain therapy. These drugs act by blocking the reuptake and potentiating the action of serotonin and noradrenaline (SSRI and SNRI). Therefore, they help reduce pain perception as well as improve mood. Medicines in this class of antidepressants include fluoxetine, duloxetine, escitalopram, desvenlafaxine, etc.
Muscle Relaxants
Injury and inflammation can often produce spasms and stiffness of associated muscles. This can increase the discomfort associated with the pain. Muscle relaxants are therefore sometimes combined with NSAIDs.
Skeletal (voluntary) muscle relaxants include methocarbamol, thiocolchicoside, and tizanidine. Muscle relaxants, such as carisoprodol and cyclobenzaprine, are prescribed for severe pain and discomfort caused by muscle spasms and stiffness. Tolperisone is a centrally acting skeletal muscle relaxant used for the treatment of increased muscle tone and pain associated with neurological diseases.
Smooth (involuntary) muscle relaxants include dicyclomine, mebeverine, and drotaverine.
Proteolytic enzymes
These are mainly used in physical injuries like bruises, wounds, or infections. Enzymes like trypsin, chymotrypsin, bromelain, and serratiopeptidase break down barrier proteins, reduce inflammation and swelling, and improve healing, which helps in reducing pain. They are often combined with NSAIDs. Sometimes antioxidants especially of the flavonoid group like rutin (rutoside) may also be added to such combinations.
Nutritional Supplements
These may be added to improve general health. These contain Vitamin D, E or those of the B group, and minerals like zinc and magnesium. However, there is no direct role in pain management. Some herbs also claim pain-relieving properties, most of which act by their calming and anti-inflammatory effects. Evidence from clinical studies or wide clinical experience should be present if prescribing such herbal supplements.
LOCAL APPLICATION (TOPICAL THERAPY)
Many of the medicines mentioned above especially NSAIDs, are available for local application also. Topical formulations include creams, balms, ointments, gels, patches, and sprays applied on the site of pain. Topical therapy is useful in giving local pain relief, as well as preventing side effects seen with oral tablets.
Rubefacients are substances that cause redness and dilation of superficial blood vessels and induce a sensation of warmth when applied. Counter-irritants are substances that induce a burning or heat sensation when applied. Since both hot temperature and pain sensation are carried by the same nerve fibers, the sensation of heat temporarily prevents the sensation of pain from being transmitted, thus providing pain relief. Many substances used in topical analgesic formulations are rubefacients and counter-irritants like methyl salicylate (oil of wintergreen), capsaicin, cinnamon, and camphor.
Herbal oils like eucalyptus, lavender, clove, turmeric, chamomile, rosemary, sandalwood, etc. have anti-inflammatory properties, and when massaged also have rubefacient properties, both of which help in pain relief. In addition, inhaling the aroma of these oils on application also induces a sense of well-being and allays pain-associated anxiety (aromatherapy).
Local anesthetics are sometimes added to topical preparation to give pain relief and soothing effects. Lidocaine is an anesthetic agent commonly added to gels and patches. Menthol (or peppermint) gives a cooling and soothing effect and is also commonly a part of gels, creams, and balms. Lidocaine and menthol are also part of mouth gels, sprays, and lozenges for relief from pain due to mouth ulcers or pharyngitis.
Topical therapy is useful in headaches, backache, muscle pain, joint pains or arthritis, and other injuries like sprain and strain. However, if the pain is deep-seated, absorption of the ingredients through the skin may not be enough to reach such deep sites.
OTHER PAIN THERAPIES
These therapies are based on the principle that larger (in diameter) sensory nerve fibers carry sensations more effectively, and these sensations are gated preferentially and perceived better by the brain and spinal cord. It is interesting that nature itself has equipped the human body to give the least preference to pain sensation perception among all sensations!
Physical therapy or physiotherapy in the form of regular and appropriate physical activity stretches, and exercise is important. A physical therapist can teach exercises that will improve strength, flexibility, and stamina. Water-based exercises and yoga can be particularly helpful.
Occupational therapy can help with workplace adjustments to reduce stress and strain on the body.
Massage therapy relies on increasing the touch and pressure sensations that are carried in preference to pain. Massage also helps relax muscles. In addition, massage gives a sensation of warmth with the help of oils and also a feeling of wellness through aromatherapy.
Acupressure is a type of massage therapy in which manual pressure is applied to specific points on the body. It is based on concepts in traditional medicine of energy flow along meridians in the body.
Heat therapy relies on the preferential transmission of heat sensation to relieve pain. Superficial heat can be given with the help of hot water bags or electric heating pads.
Shortwave diathermy (SWD) uses high-frequency pulsed or continuous electromagnetic energy to generate deep heat.
Ultrasound therapy uses sound waves, or ultrasound rays that penetrate within the body generating heat, increasing blood flow, and relaxing muscles, thereby reducing pain and muscle spasms.
Transcutaneous electrical nerve stimulation (TENS) is a therapy that uses low-voltage electrical current to provide pain relief.
Biofeedback is a type of mind-body technique one uses to control some of the body’s functions, such as heart rate, breathing patterns, and muscle responses. It helps to gain awareness of many physiological functions of one’s own body by using electronic or other instruments, with the goal of being able to manipulate the body’s systems at will.
Psychological therapies include cognitive and behavioral therapies (CBT), mindfulness, positive imagery, music therapy, counseling, acceptance and commitment therapy (ACT), and hypnosis.
Lifestyle therapy includes stress management, engaging in group activities, developing hobbies, having good family and social support, and maintaining a healthy diet.
Also read:
Arthritis – Awareness of the Causes, Types and Health Impact
Fibromyalgia – 5 Important Points of Awareness and Understanding