Chronic venous insufficiency refers to the suboptimal functioning of veins and its consequences.
BLOOD CIRCULATION BASICS
Blood Vessels
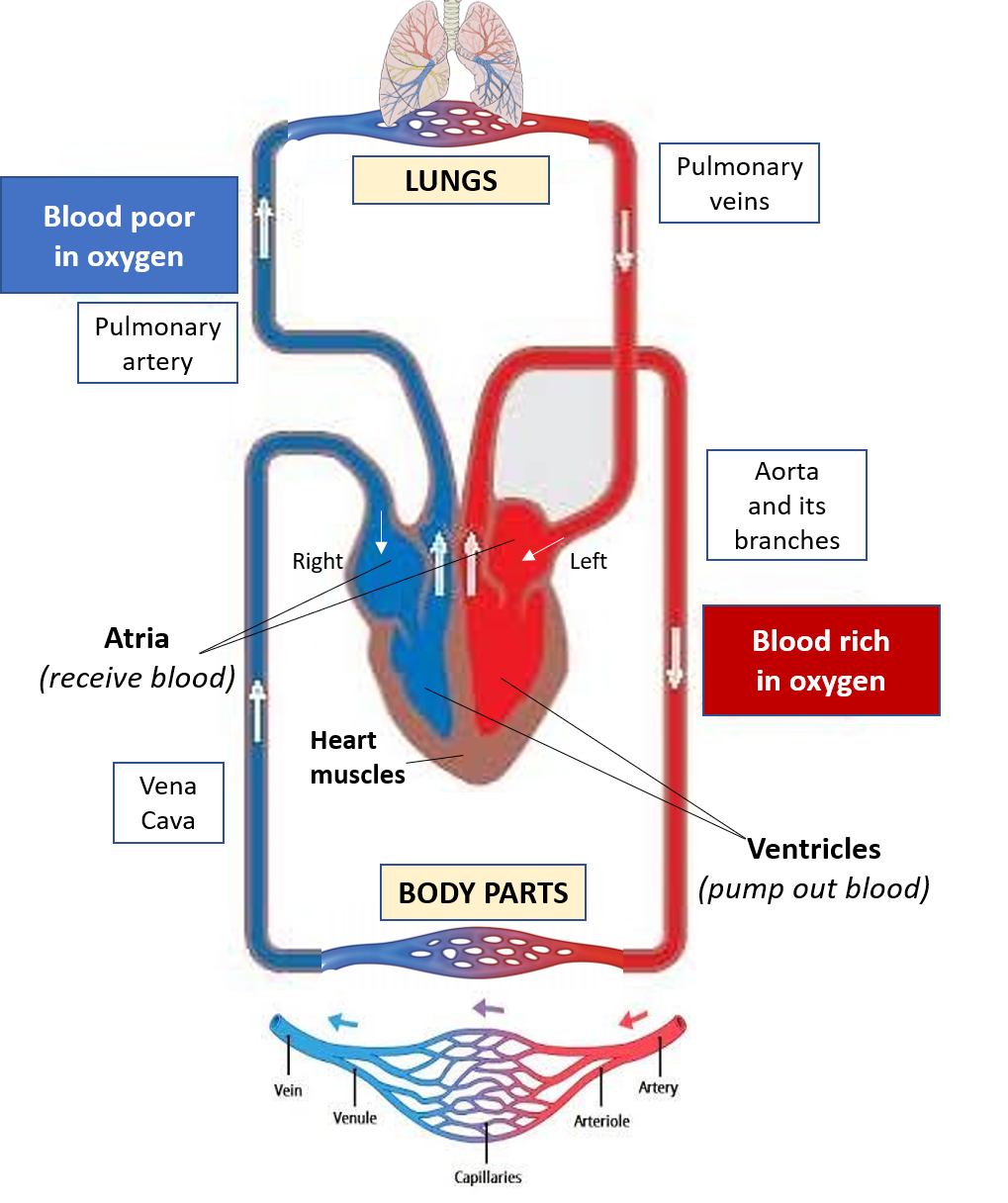
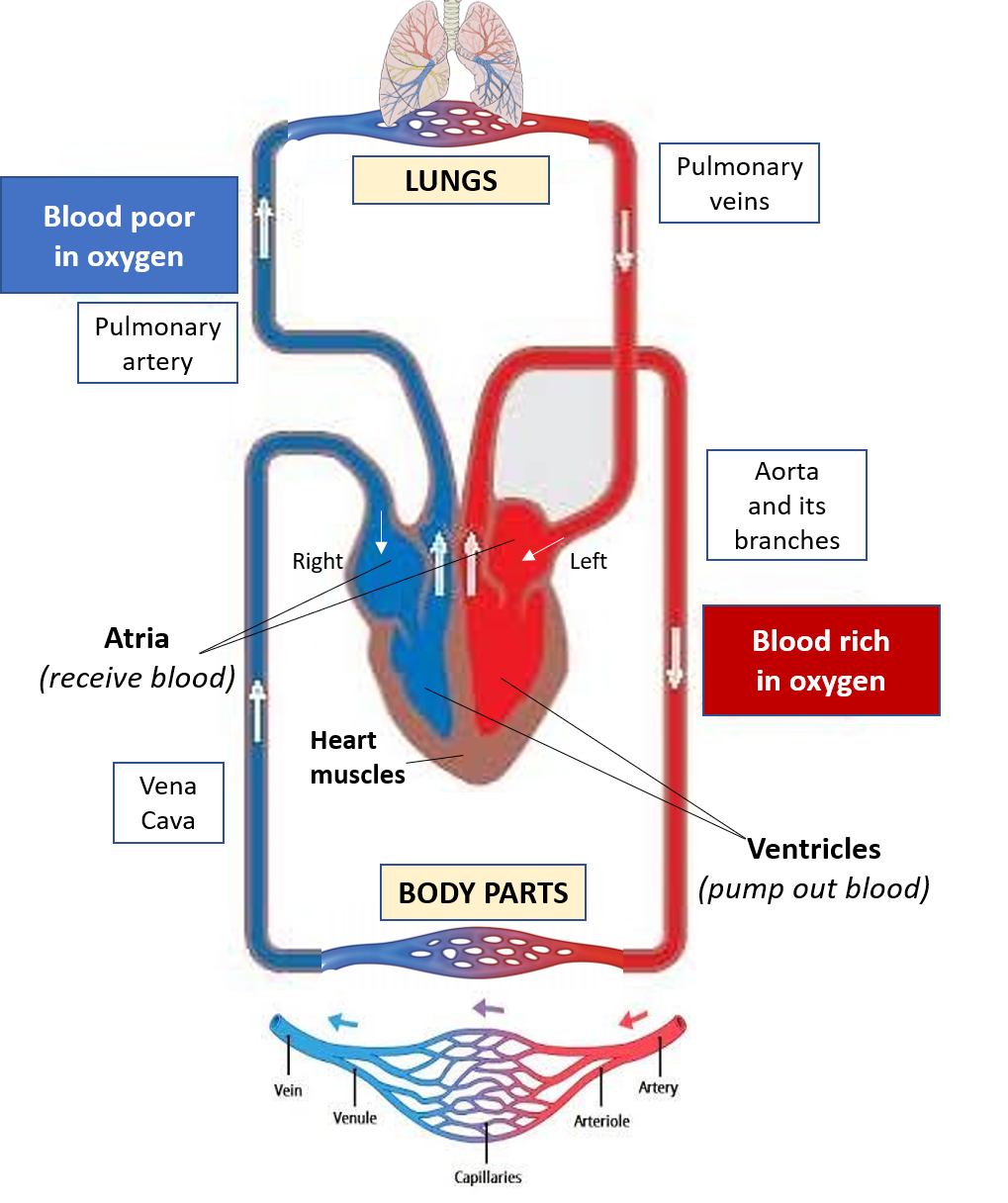
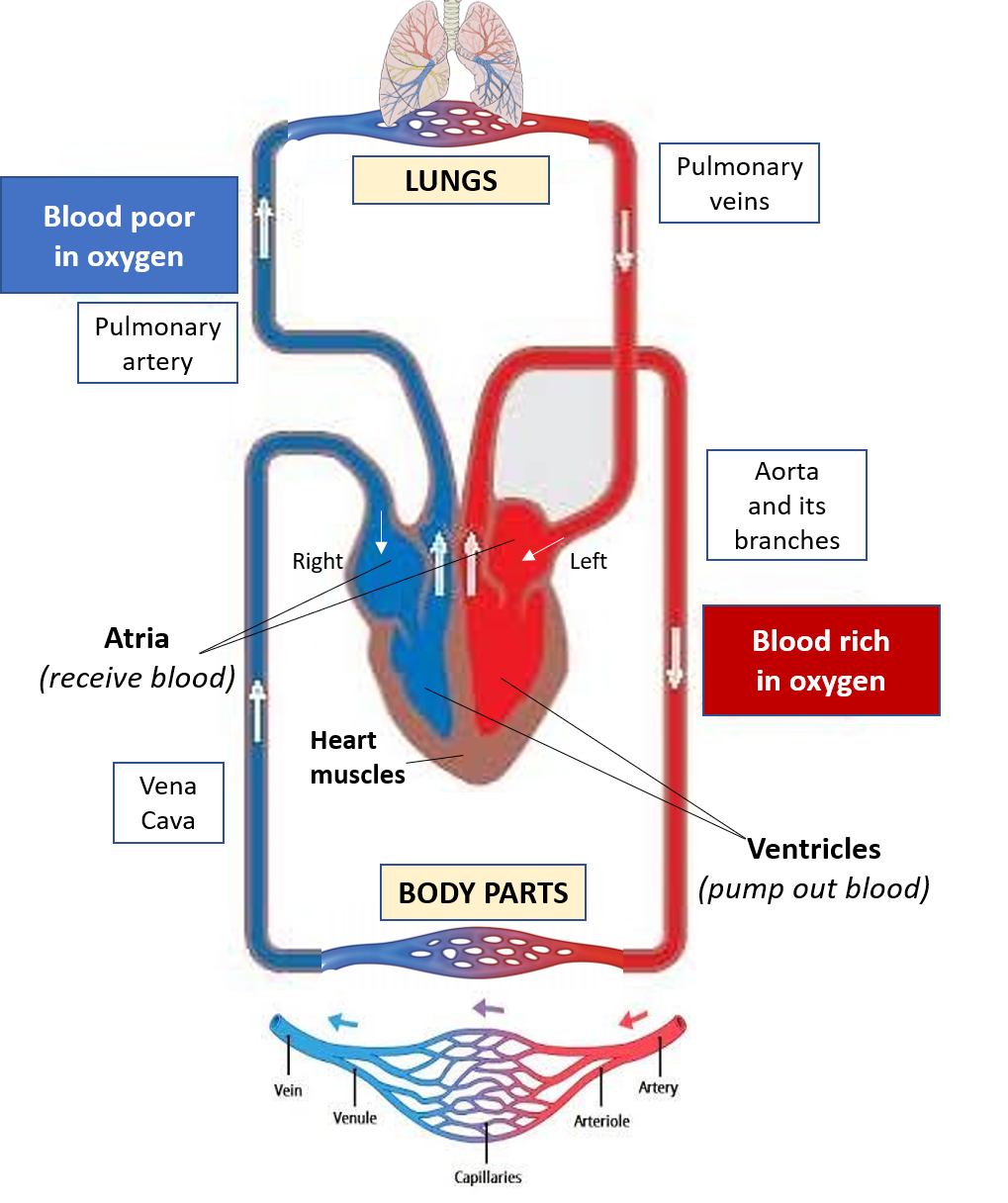
The blood vessels of our body are the arteries, that carry oxygen-rich blood from the heart to all body parts, and the veins that carry oxygen-deficient (deoxygenated) blood from all body parts back to the heart. The main artery is the aorta which leaves the left side of the heart and then branches out as many other arteries, that further divide into smaller arterioles finally breaking down to form very narrow thin vessels called capillaries. It is at the level of the capillaries that oxygen is delivered and exchanged for carbon dioxide. Thereafter the capillaries join together to form venules which further join together to form the veins that all come together to form the 2 main veins (superior and inferior vena cava) that bring blood back into the right side of the heart.
While arteries carry oxygen-rich blood and veins carry deoxygenated blood, the only exception to this rule are the pulmonary (lung) artery and veins. The pulmonary artery carries blood from the right side of the heart to the lung for oxygenation, while the pulmonary veins carry the oxygenated blood from the lungs to the left side of the heart.
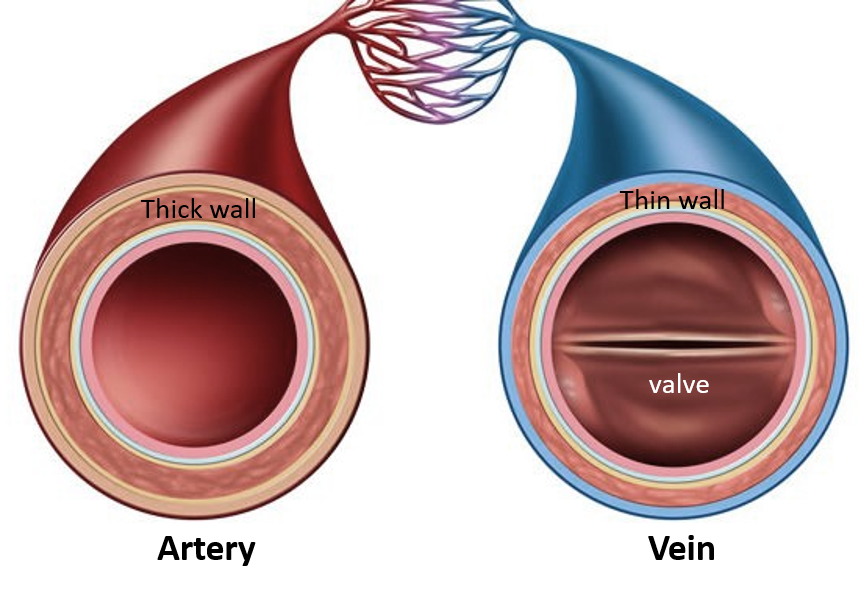
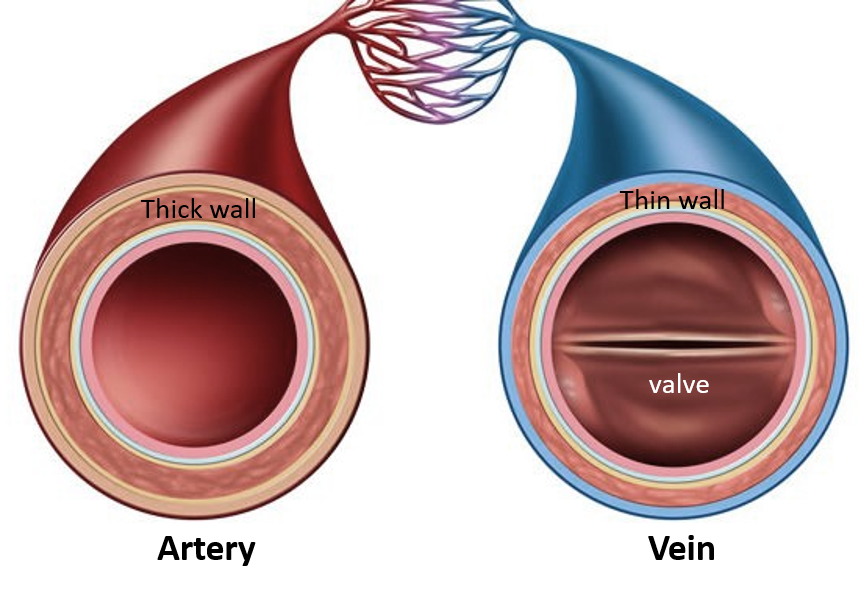
Arteries versus Veins
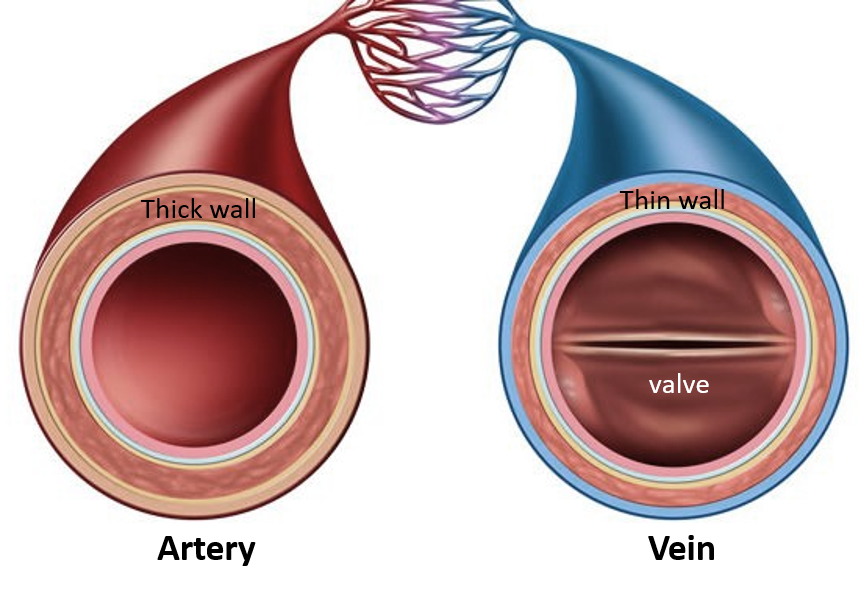
The arteries have thick and elastic walls, and the blood flow is pulsatile exerting a maximum and minimum pressure on the artery walls (blood pressure -BP 120/80 mm Hg). Whereas the veins have thin, flexible walls with blood flowing at low pressure (5-8mm Hg) in a more constant, non-pulsatile manner. Therefore, veins rely on the action of muscles to help in blood flow against gravity and have valves to prevent the backflow of blood. While arteries are always deep, veins can be both superficial (easily visible under the skin) or deep.
Due to the high pressure of blood flow in arteries, their inner walls are more prone to damage leading to the formation of plaques and clots (atherosclerosis/arteriosclerosis) that can obstruct flow. There are many risk factors contributing to this leading to cardiovascular disease. Veins can suffer from problems of deficiencies in the competence of their walls, valves, and surrounding muscle action, or veins can also get blocked and inflamed due to clots.
CHRONIC VENOUS INSUFFICIENCY
CAUSES
This occurs due to weakened or damaged vein walls, and incompetent valves, which results in backflow, stasis (stagnation), and pooling of blood. This is seen in the leg veins as blood has to flow to the heart against gravity. Normally the calf and foot muscle action during walking helps to push up the blood in the leg veins, and the valves prevent backflow.
Due to aging, the vein walls and valves become weak. During prolonged standing or sitting, muscle action is not present to aid blood flow in the leg veins. Therefore commonly, a combination of aging and low mobility results in chronic venous insufficiency (CVI). CVI is more common in the elderly (>50 years) and in women. Risk factors include obesity, smoking, family history, and during pregnancy.
CVI can also occur as a result of clot formation (thrombosis) and inflammation (phlebitis) in the veins causing damage to the vein valves and wall when it is called post-thrombotic syndrome. 30% of cases of deep vein thrombosis (DVT) develop CVI in the course of 10 years.
Other causes of chronic venous insufficiency include direct injury, and rarely pelvic tumors or anomalies in the blood vessels (vascular malformations).
SIGNS AND SYMPTOMS
When the superficial veins are affected, they are prominent and visible along the leg appearing tortuous and twisted called varicose veins.
Deep veins with insufficiency are not visible but present with swelling (edema) of the leg and ankle which is more prominent after prolonged standing or sitting. The swelling is typically pitting’ (a depression or dimple remains after pressing on the swelling for a few seconds). Sometimes a collection of small dilated tortuous veins called ‘spider veins’ may be present on the surface as a telltale sign.
CVI can cause leg ache and cramps, skin irritation/itchiness, and discoloration. In severe cases, capillaries can rupture due to the pressure from the backflow, causing bleeding, inflammation, and breakdown of the overlying skin to form a venous ulcer.
CVI of the veins around the anus is called piles (hemorrhoids) similar to varicose veins. The veins become swollen and inflamed, cause pain, irritation, and discomfort especially while passing stool, and also sometimes rupture and bleed.



MANAGEMENT
Preventive measures for CVI include regular exercise (especially walking, or others like cycling, swimming, and yoga) and avoidance of prolonged standing or sitting. In long flights or at office, try to walk around every 1-2 hours, and if that is not possible then while in your seat itself bend and raise your legs a few times every half-one hour. Weight loss if obese, stopping smoking and eating a healthy and balanced diet are other important measures.
Diagnosis of CVI is made based on history, signs and symptoms, and clinical examination. Sometimes tests to rule out venous obstruction due to clot formation (deep vein thrombosis – DVT) may be ordered which include a blood test called D-dimer or an imaging procedure to evaluate blood flow called vascular duplex ultrasound.
Management and treatment of CVI when it has developed requires the following –
- Prolonged standing should be avoided.
- Legs should be kept elevated with pillows just above heart level, while sitting.
- Exercises like walking, leg raising and stretches while sitting, cycling, water aerobics/swimming, yoga, etc. under guidance can help strengthen leg muscle action and tone, without unduly straining the muscles.
- Diet should be nutritious and healthy. Refined carbohydrates like flour (maida) and sugar should be reduced while whole-grain and multigrain wheat/oat preparations and brown rice should be increased. Avoid high salt and fried foods, and include more fresh fruits, green vegetables, pulses, nuts, soy, and fish in the diet. Substances called flavonoids found in vegetables and fruits like spinach, broccoli, capsicum, onions, grapes, apples, berries, citrus fruits, and garlic can be increased in the diet.
- Smoking should be avoided. Alcohol consumption should be reduced.
- Tight clothes and belts should be avoided.
- Compression stockings can be worn which apply pressure to help blood flow. Most ready purchase compression stockings in pharmacies exert a pressure of 5-10 mm Hg, however, for higher pressure stockings >20mm Hg, a doctor’s prescription and monitoring is needed. Stockings should be of the correct fit and size (not too loose or tight, and not bunching up). Depending on the position and extent of varicose veins, the stockings can be below the knee, above the knee, or full leg till the waist. The stocking should be removed while going to bed, and be cleaned and washed regularly.
- Skin hygiene should be well maintained. Apply moisturizers to prevent skin cracking, and avoid scratching or picking at the overlying skin. In case of itching and irritation, herbal oils like horse chestnut or lavender can be applied. In severe cases, an anti-inflammatory cream containing a corticosteroid, and/or zinc oxide may be prescribed with an antibiotic/antifungal where needed. Medicated compression bandages are available to provide both skincare and aid blood flow. Venous ulcers if present should be treated with appropriate dressing.
- Medicines may also be recommended in some cases. These include calcium dobesilate and flavonoids (troxerutin/oxerutin, diosmin, and hesperidin) which improve blood flow and reduce vessel wall damage, leakage, swelling, inflammation, clotting, and tortuosity.
- Procedures and surgeries may be needed in certain severe and non-responsive cases. Sclerotherapy and thermal ablation (using a laser of high-frequency radio waves) are outpatient procedures that can help to collapse and close varicose veins and prevent bleeding and ulcers. Surgical treatments include ligation (cutting and tying off) and stripping the affected vein, microincision ambulatory phlebectomy (removing the affected vein through small openings), and vein bypass surgery. These procedures and surgeries are generally performed by experienced general surgeons or vascular surgeons
Also read:
For any query, additional information or to discuss any case, leave a comment or write to info@drvarsha.com and be assured of a response soon.
Reference: CVI-Society for Vascular Surgery


