An injury can cause a bruise, sprain, strain, and sometimes fracture or dislocation, which are a part of life. Discussed here are these acute blunt trauma injuries without surface wounds, cuts or bleeding. Wounds should be treated with appropriate first aid when present. While most such minor injuries like bruises, sprains and strains can be managed at home, major ones causing fracture or hematoma would need early and timely medical attention.
BRUISE AND HEMATOMA
BRUISE
A bruise (also called a contusion) is the result of an injury, causing leakage of blood from capillaries (small blood vessels supplying oxygen to various body tissues, and connecting arteries and veins). This leads to visible swelling and discoloration of the injured area. The discoloration is initially red due to fresh oxygen-rich blood but as the oxygen is lost and the pigments break down, the color can change to bluish-purple or blackish, and finally to a yellow-light brown in 2-3 days. A bruise is often painful, especially on touching or pressing (tenderness).
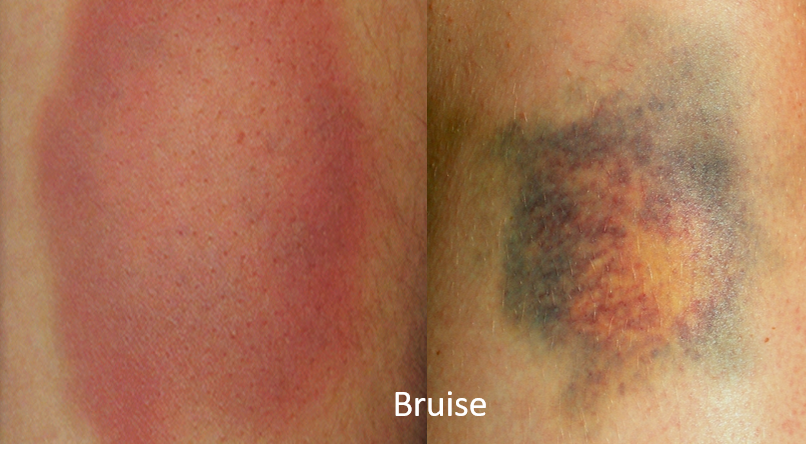
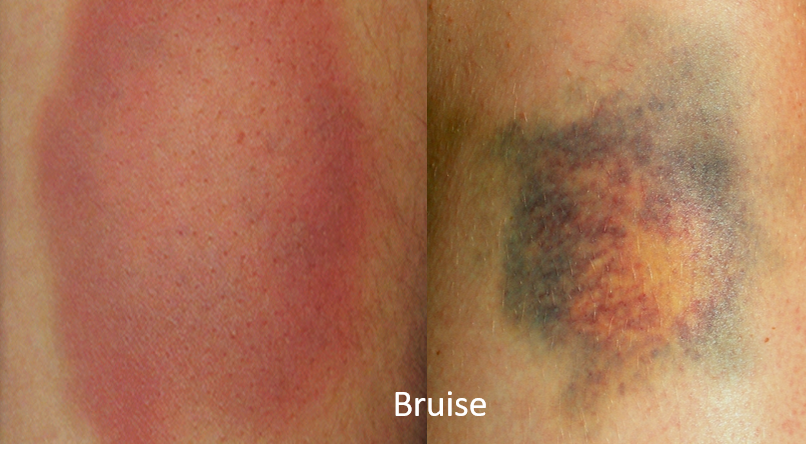
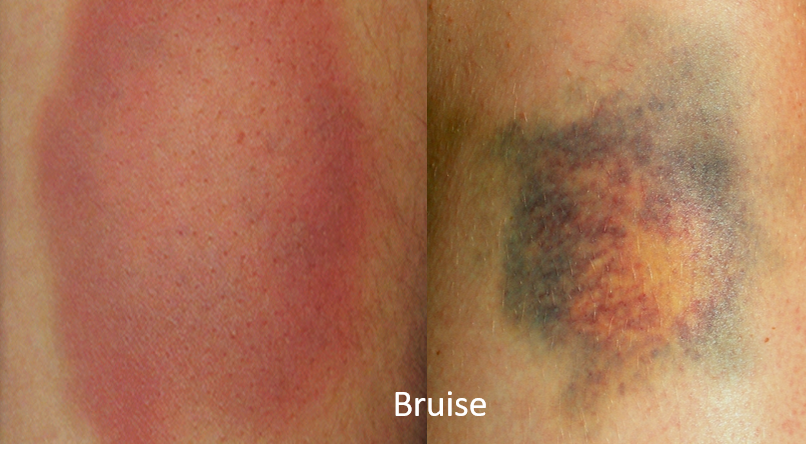
A bruise may be referred to by different medical terms depending on its size and appearance – petechiae (small pinpoint <3mm), purpura (3-5 mm, round purple in appearance), and ecchymosis (>1cm appears blackish-blue).
HEMATOMA
A hematoma refers to a larger and often deeper collection of blood due to injury and leakage of blood through the damaged blood vessel wall (can involve arteries and veins in addition to capillaries). So, a bruise can be regarded as a small hematoma visible under the surface of the skin. A hematoma is associated with more inflammation and activity and can progressively increase in size sometimes at a rapid pace.
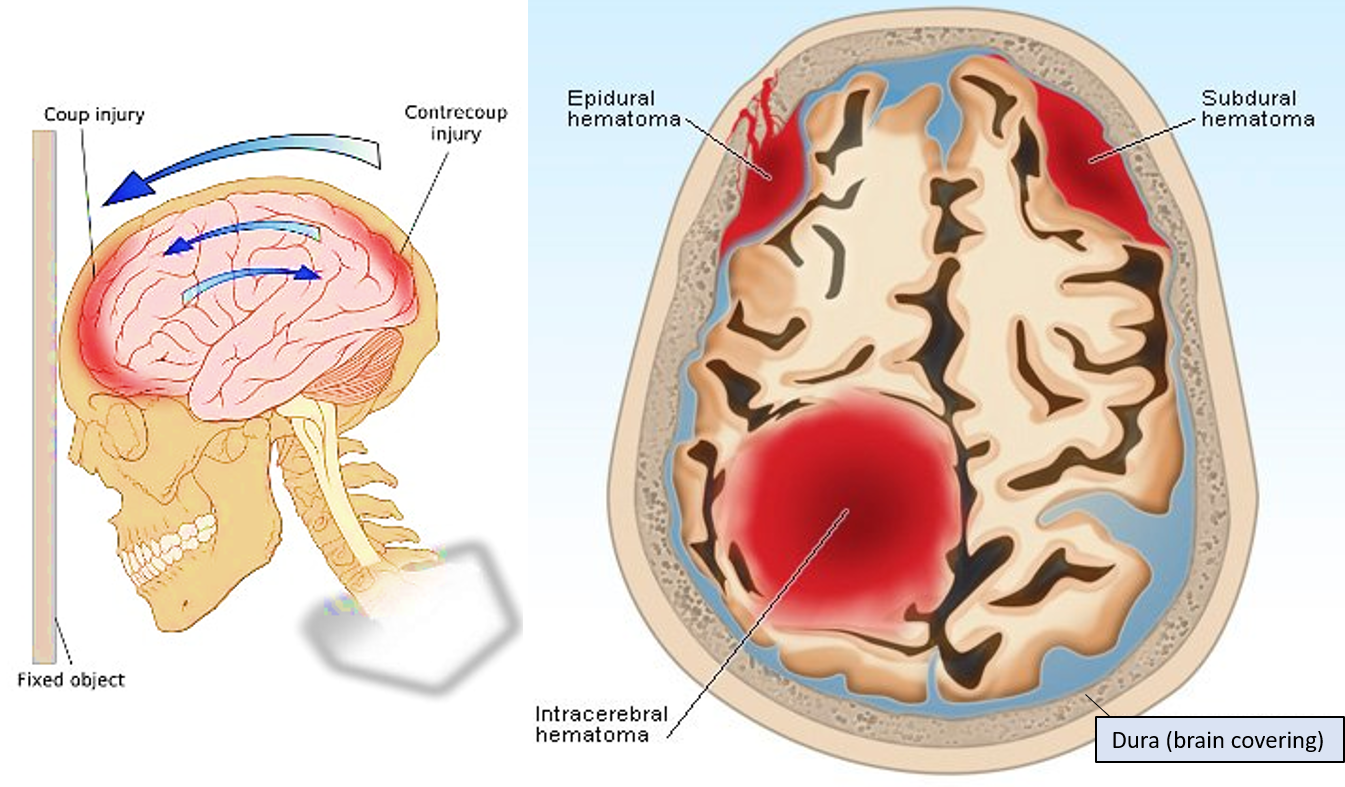
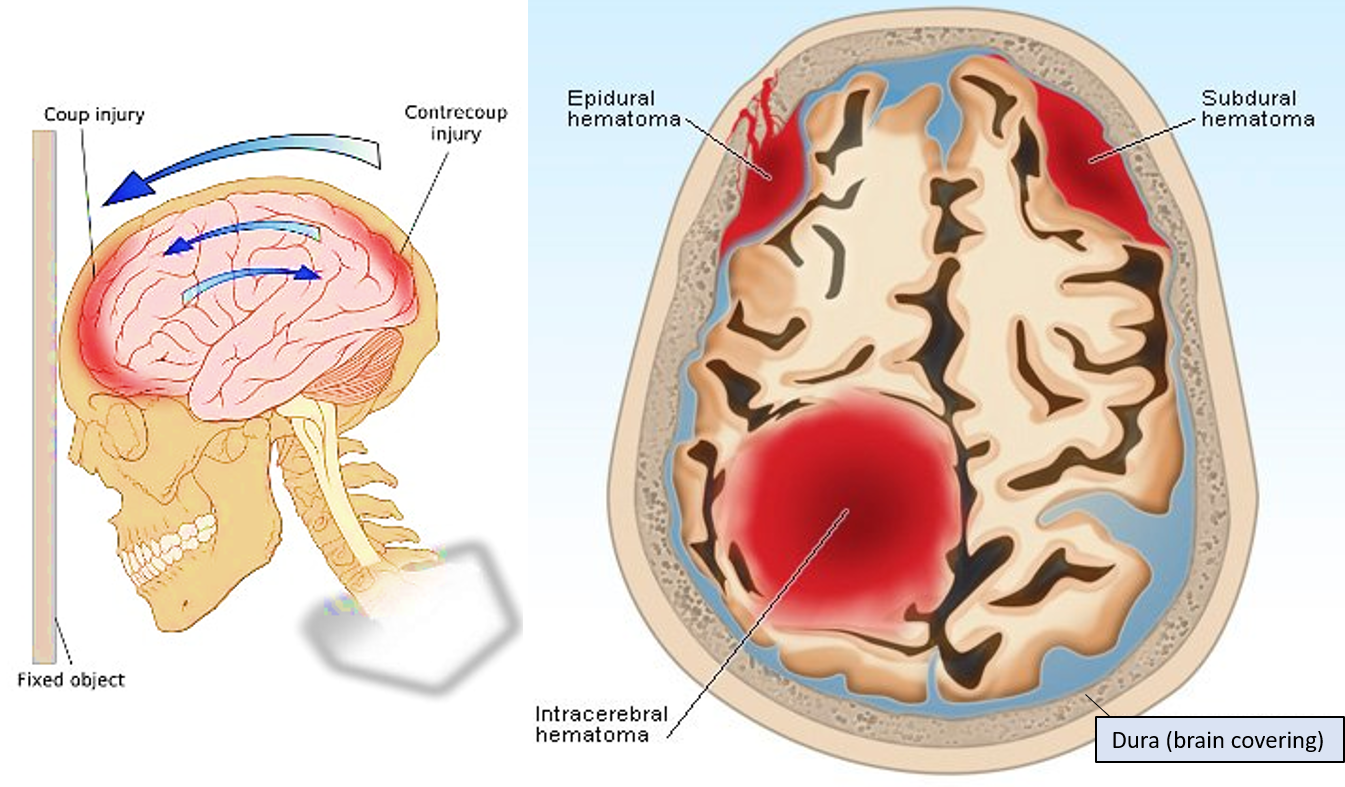
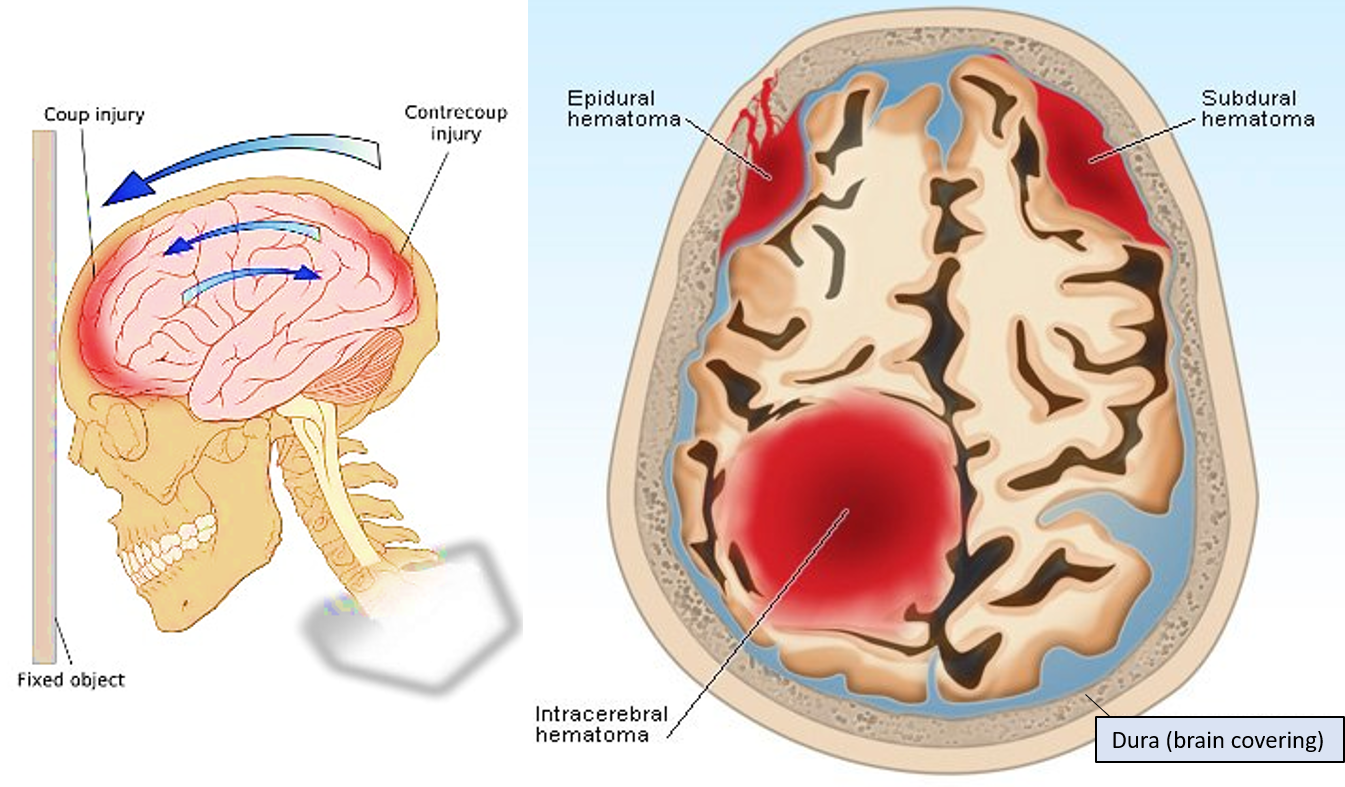
Hematomas may also form due to internal damage and bleed, and therefore escape diagnosis till suspicious symptoms appear. For example, after a concussion (blunt trauma to the skull/brain) there can be an intracranial hematoma formed in any of the layers between the skull and the brain (epidural -outside the brain covering, subdural – under the brain covering and intracerebral – in the brain). In a concussion, damage can occur at the site of impact (coup) or opposite side (contrecoup).
Hematomas may also form in the anus, breast, muscles, nail, ear (after improper traumatic piercing), etc.
TREATMENT
Bruises and visible hematomas are treated with the RICE technique – resting the injured site, ice (or cold pack) application, compression, and elevation of the injured part (in lower limb injuries). Ice should not be applied directly but wrapped in a thin towel and for not more than 10-15 minutes at a time. Compression can be done by a crepe bandage. Medicines to reduce pain and swelling (non-steroidal anti-inflammatory drugs -NSAIDs like ibuprofen, diclofenac, aceclofenac, etc.) may be prescribed with monitoring for a visible bruise or hematoma. A bruise typically resolves within 3-7 days. Visible hematomas may take up to 1-2 weeks.
In the case of internal hematomas, it is important to be alert for signs and symptoms after any trauma but especially head injury. These symptoms include persistent headache, confusion, nausea-vomiting, drowsiness, dizziness, or behavioral/personality change. A CT scan or MRI will reveal the hematoma, and a drainage procedure by making an opening in the skull (by drilling a burr hole or removing a part of the skull – craniotomy/craniectomy) is performed by a neurological expert.
While bruises and hematomas are usually caused by an injury, they can also occur in people with bleeding disorders or those on anticoagulant blood thinner medicines, sometimes without or after minor trauma.
STRAIN AND SPRAIN
Strain and sprain refer to injuries of the tendon (joins bone to bone) and ligament (joins muscle to bone), respectively. These also present with pain and swelling, however unlike a bruise no discoloration is seen. While bruise is caused by direct blunt trauma, sprains and strains happen more due to indirect trauma like sudden and abnormal movements (twisting-turning, slipping, lifting, sports, exercise pull-pushups, etc.).
In a sprain, the ligament may tear sometimes partially or fully (complete tear where one end detaches from bone). This may make the joint unstable and susceptible to repeated sprains as commonly seen with knee or ankle.



TREATMENT
The treatment remains RICE. The part should be rested. Ice (or cold pack) application helps in first 24-48 hours, 2-3 times a day in 10–15-minute sessions to reduce swelling. A compression crepe bandage should be applied. In case of common knee and ankle sprains and strains, elevating that limb with a pillow is recommended. NSAIDs may be prescribed for symptomatic relief. Sprains and strains resolve in 5-10 days.
Severe sprains due to torn ligaments often need complete immobilization for a few weeks and may also require physiotherapy.
Recurrent sprains or joint instability especially with complete ligament tears may need surgery to repair and reconstruct the ligament followed by immobilization and physiotherapy.
FRACTURE
Sometimes due to injury, an underlying fracture (break in the bone) may occur, that would need medical intervention. Fracture also presents with swelling and pain, especially on touching and pressing, just like a bruise, and it may be difficult to say whether it is just a bruise, sprain/strain or a fracture. The following 5 clinical signs help suspect a fracture –
- Pain – A fracture leads to intense, sharp and stabbing pain. The pain can be severe on the slightest movement or touching of the injured area. The pain of the fracture is much more than that of a bruise or sprain/strain. Ice and compression do not reduce, and in fact, may worsen the pain.
- Swelling – In a fracture, the swelling does not go down significantly with ice therapy. Ice constricts the capillaries and reduces leakage of blood. However, the injury causing a fracture is more extensive involving bone inflammation, which will not be effectively relieved with ice. Also, sometimes the swelling may be due to a protruding or displaced bony fragment.
- Movement – The slightest movement can produce pain in a fracture. It may not be possible to put any weight on the affected limb or part, and mobility is usually lost far more in a fracture, than in a bruise or a sprain/strain.
- Deformity – Any change or abnormal appearance of the contour, shape, position or stability of the affected part, is very suggestive of a fracture. If the swelling feels hard or like a bony protrusion, it is almost definitely a fracture.
- Crepitus – If at the time of injury there was a grinding or snapping sound, it can indicate a broken bone. Crepitus is a crunchy feeling one gets below the swelling on feeling, which also suggests a fracture.
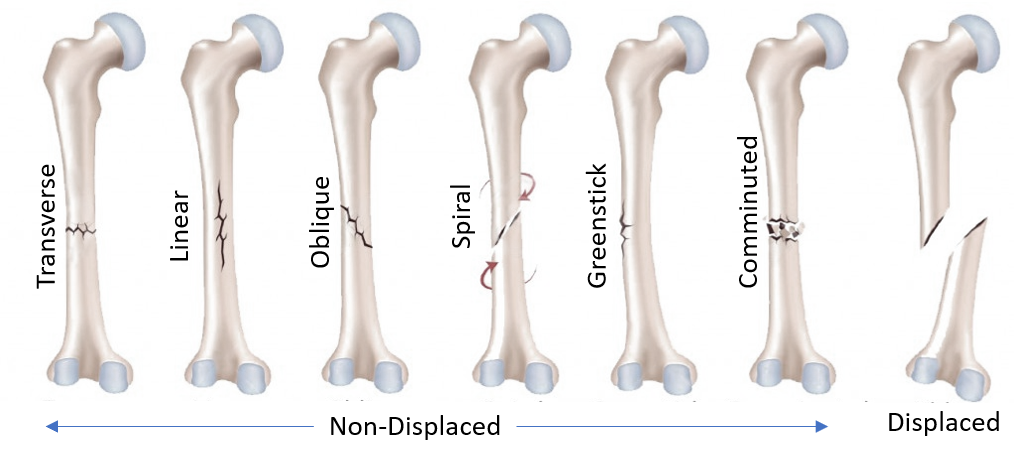
TYPES
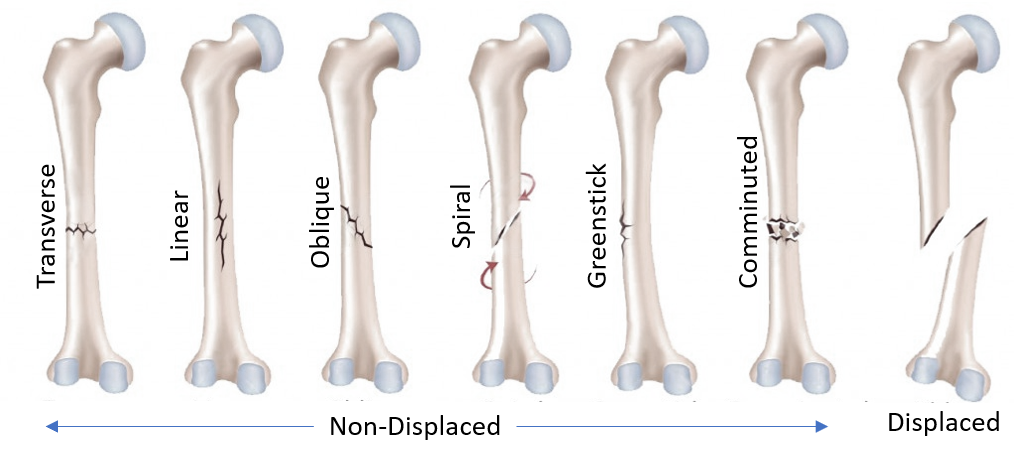
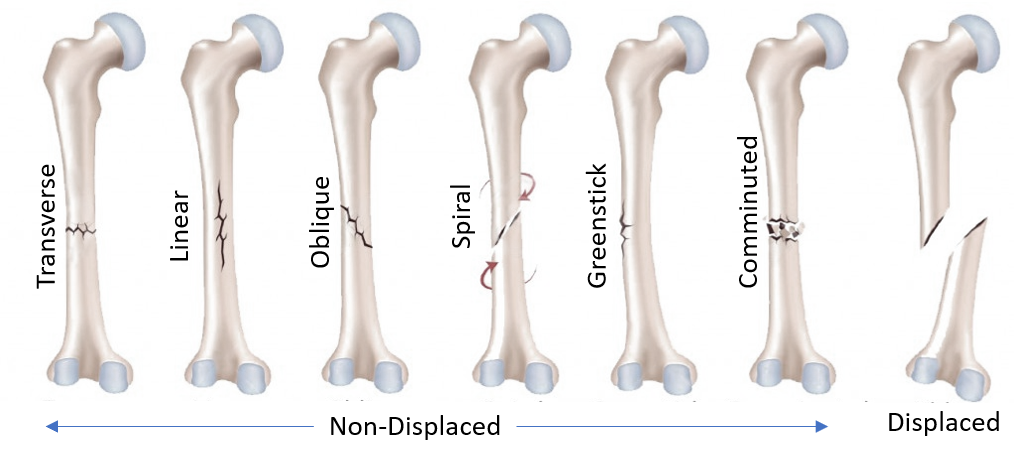
Fractures associated with open wounds are called open or compound fractures. Most fractures after blunt trauma do not have surface cuts or wounds and are called closed fractures. A fracture in which the alignment or position of any of the fractured bone fragment shifts, it is called a displaced fracture. Types of fractures are shown below.
While most fractures are caused by significant injuries, people who have weak or thinning bones (osteoporosis) can suffer fractures more easily with relatively less or insignificant trauma. Stress fractures are cracks in the bone caused by repetitive force, overuse, or trauma like jumping up and down, running or walking long distances in inappropriate footwear, or without proper muscle training and graded step up.
TREATMENT
Sometimes there may be a hairline crack in the bone, or patients with a high pain threshold may continue to move or use the affected part, and treat the pain and swelling like a bruise or sprain/strain. Even if one does not suspect a fracture, resting the part for at least 24-48 hours is important, and one should seek medical consultation if swelling and pain do not come down in 24 hours. X-ray of the affected part is the most definitive way of ruling out a fracture.
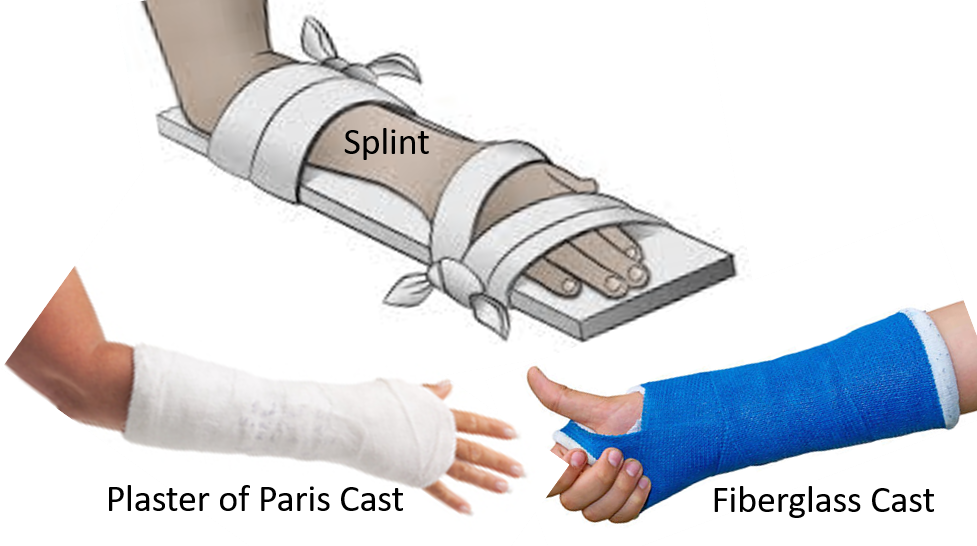
If suspecting a fracture, the most important action point is to immobilize the part with the help of a splint, so that the broken bone does not change its position or alignment. Thereafter X-ray of the affected part followed by a cast application for immobilization and healing should be done in a medical set-up preferably under orthopedic supervision. The cast is usually kept in place for 3-6 weeks or longer, depending on the type of fracture and part affected. Conventionally casts were made of plaster of Paris, but now new age flexible synthetic fiberglass casts are available which are lighter, more porous so comfortable, and feasible for taking X-rays.
Displaced fractures with shifting of the bone from its position or loss of alignment between the bone segments require a procedure called ‘reduction’, which may be done in the clinic (closed reduction) or by surgery (open reduction). This makes the bony fragments align and prevents abnormal healing/joining (malunion) which can lead to deformity and movement restriction (may need physiotherapy) that can sometimes be permanent. Fractured fragments may also be fixed by nails, rods/plate, and screws (fixation) which may be visible outside (external fixation) or put internally after open reduction (internal fixation).
DISLOCATION
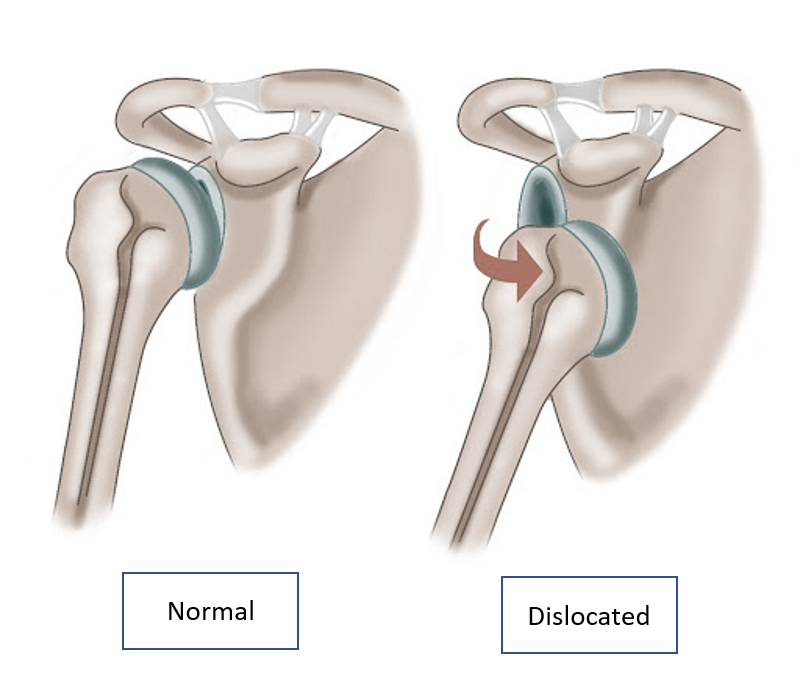
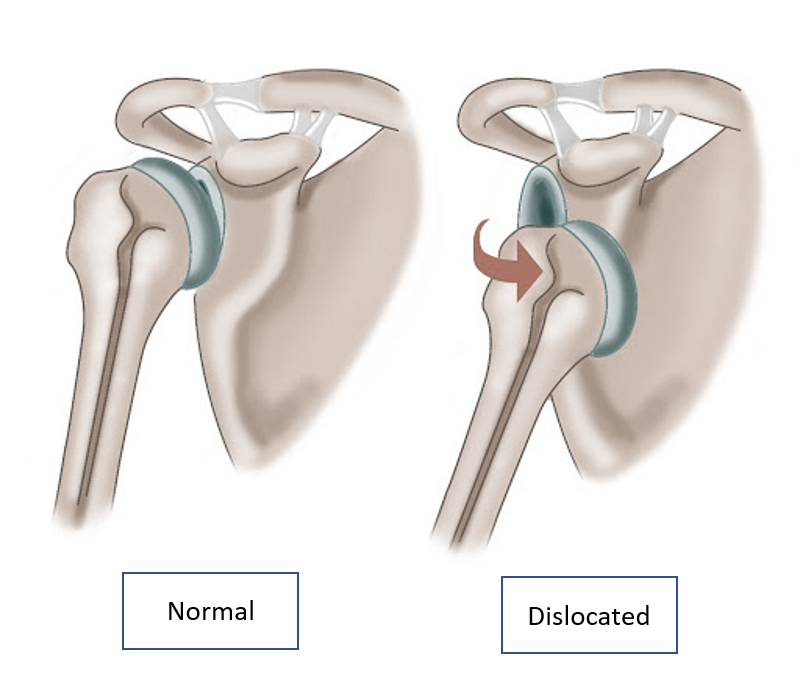
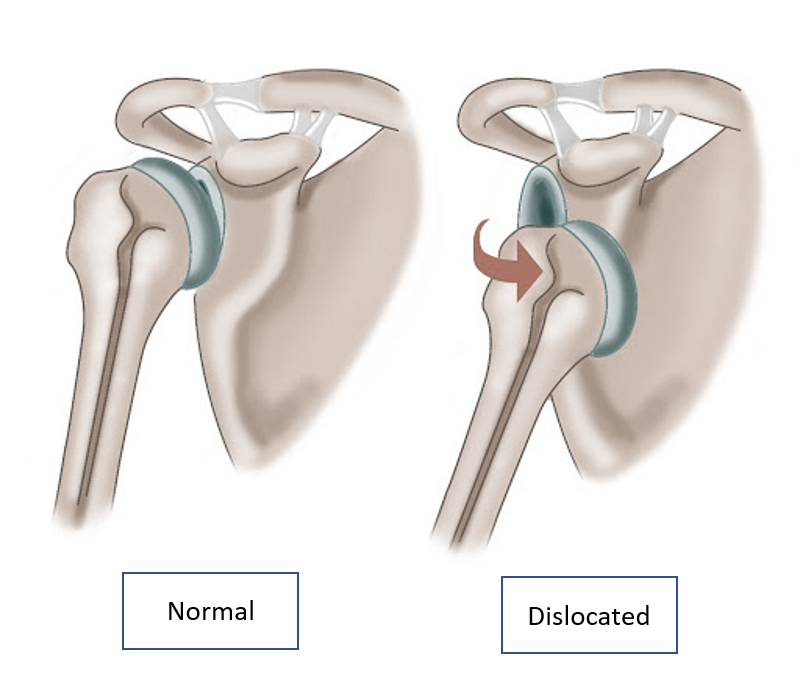
An injury that leads to a displacement of the end of the bone from its normal position in the joint, is called dislocation. The bone is not broken or cracked but has just moved out of its normal position and alignment. Dislocation is seen after a fall, accident, collision, and during sports. The most common joints affected are the shoulder in adults and the elbow in children. Thumb/finger joints are also dislocated with force bending. The joint appears temporarily deformed and loses mobility, and there is often sudden and severe pain and swelling. The term subluxation is used when the dislocation is incomplete and some part of the bone ends of the joint are still in contact.
TREATMENT
Rest and immobilization (preferably with a splint) of that joint, along with ice to reduce swelling and an analgesic for pain are first aid measures. It is very important not to move the joint or manipulate it as it can cause injury to nerves, blood vessels, and other structures.
Dislocation has to be corrected by an orthopedist by external manipulation under anesthesia to bring the bone end back to its correct aligned position in the joint. In some cases, surgery may be needed. Physiotherapy is sometimes recommended after treatment to improve mobility and recovery.
Also read:
Weak, Thinning Bones: Osteoporosis Risks and How to get Screened
For any query, additional information or to discuss any case, write to info@drvarsha.com, and be assured of a response soon.
References
Intracranial hematoma – Mayo clinic


