WHAT IS BRONCHIECTASIS?
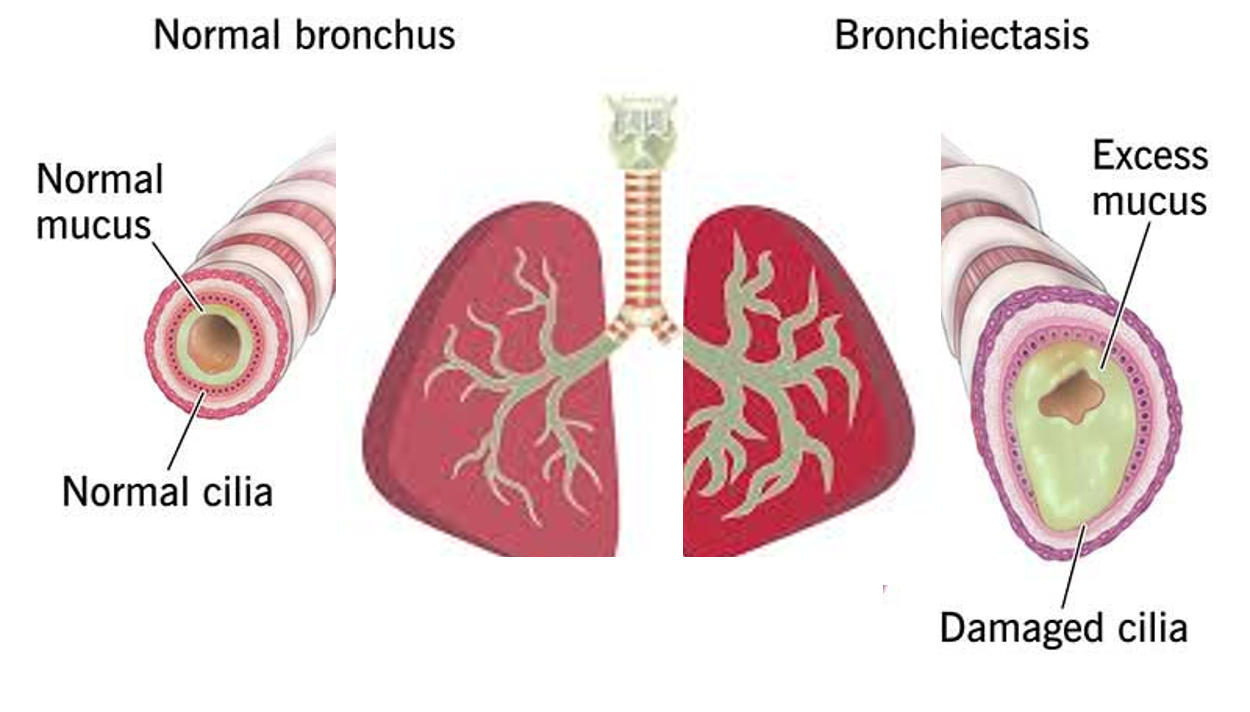
Bronchiectasis is a chronic lung condition where the lower airways (bronchi) become damaged, making it difficult to clear mucus, thereby leading to an increased risk of infections. The damaged lower airways become permanently widened. Reduced effectiveness at clearing mucus from the lungs creates an environment where micro-organisms, especially bacteria, can thrive and cause infections.
Bronchiectasis, based on the appearance of the airways, is sometimes classified as cylindrical (or tubular), varicose, or cystic. Cylindrical bronchiectasis is the most common and the least serious form, while cystic bronchiectasis is the most severe form. Bronchiectasis may be focal (in one area) or diffuse (in many areas throughout the lungs). When scarring in the lungs pulls the airways out of shape, it is called traction bronchiectasis.
Bronchiectasis can occur at any age, but is far more common in older adults >65 years who constitute half of all cases diagnosed. However, in the case of genetic conditions like CF and PCD mentioned below, diagnosis is in early childhood or infancy.
CAUSES AND ASSOCIATED CONDITIONS
Bronchiectasis is caused by two phases of airway damage. In the first phase, the initial damage (injury or “insult”) is caused by an infection, inflammatory disorder, or another condition that affects the lungs. This makes one more likely to suffer from airway inflammation and repeated infections that cause further damage, leading to the second phase of the vicious cycle of infection-damage-infection.
Some of the specific causes that cause the initial and continuing airway injury and inflammation are:
GENETIC DISORDERS
Individuals with the defective mutated genes who inherit two copies, one from each parent, are sufferers, while those who inherit only one copy of the mutated gene are carriers, do not typically experience symptoms, but can pass the gene on to their children.
- Cystic Fibrosis (CF), is a genetic disorder caused by mutations in the CFTR gene, which encodes a protein that regulates the movement of salt and water in and out of cells. So, a defective gene inhibits the ability to dilute mucus, which becomes thick, sticky, and very difficult to clear from the airways and gut. Symptoms are both respiratory (persistent cough, wheezing, shortness of breath, frequent lung infections, and inflamed nasal passages) and gastrointestinal (greasy, foul-smelling stools, constipation, poor weight gain, and delayed growth in children), with salty-tasting skin. CF is the most common cause of bronchiectasis in the developed world. Cystic fibrosis (CF) is typically diagnosed by 2 years of age, due to newborn screening and the presence of symptoms.
- Primary ciliary dyskinesia (PCD) is also a genetic disorder due to defects in cilia (tiny hair-like structures) that help clear mucus. PCD primarily affects the lungs, sinuses, and the ears, and presents with chronic cough and wheezing, respiratory distress at birth, excess mucus, chronic nasal congestion, and recurrent ear infections.
- Alpha-1 antitrypsin deficiency (AATD) is a genetic disorder where the body produces inadequate or defective alpha-1 antitrypsin protein, which normally protects the lungs and liver from damage. AATD increases the risk of developing chronic obstructive pulmonary disease (COPD) and bronchiectasis. Symptoms of lung disease in AATD can include shortness of breath, wheezing, and a chronic cough, which may appear between the ages of 20 and 50 years, and smoking and exposure to environmental toxins can accelerate the progression of lung disease in individuals with AATD.
INFECTIONS AND INFLAMMATION
- Tuberculosis (TB) or other Mycobacterial infections (MAC – Mycobacterium Avium Complex, seen in those with compromised immunity) are the most common cause of bronchiectasis worldwide.
- Autoimmune or inflammatory disorders, like rheumatoid arthritis (RA), inflammatory bowel disease (IBD), lupus (SLE), Sjögren’s syndrome, etc.
- Airway obstruction due to foreign bodies, tumors, or enlarged lymph nodes.
- Compromised Immunity due to conditions (like HIV), or immunosuppressive drugs (for cancer or post-organ transplant).
- Allergic broncho-pulmonary aspergillosis (ABPA), an allergy to a type of fungus.
- COVID cases who had pneumonia, underwent hospitalization, and have lung scarring and reduced lung capacity.
- Lung fibrosis (scarring) from radiation, or a severe pneumonia, or chemical injury.
SYMPTOMS
Bronchiectasis can significantly impact a person’s quality of life due to chronic symptoms, frequent infections, and potential for lung damage and respiratory failure. The main symptoms are:
- Cough, which is persistent, with lots of mucus and pus (mucus often foul-smelling)
- Sometimes coughing up blood (hemoptysis).
- Recurrent respiratory tract infections – like colds, ear infection, bronchitis, etc.
- Shortness of breath (dyspnea) and wheezing.
- Swollen fingertips with nail clubbing.
- Fever, chills, and night sweats, especially during flare-ups.
- Fatigue and decreased quality of life
- Impacted growth and development in children
Damage caused by severe bronchiectasis can lead to life-threatening complications, including:
- Respiratory failure due to the lack of oxygen in the blood and tissues.
- Haemorrhage/bleeding due to blood vessels in the lungs getting damaged and rupturing.
DIAGNOSIS
A thorough work-up is required to diagnose the above conditions if present.
Genetic testing for CF and PCD, sweat test (for chloride levels for CF), and nasal or bronchial ciliary biopsy and microscopy (for PCD) is advised in symptomatic infants and children. Blood tests to measure AAT levels and genetic testing to identify specific gene mutations for AATD may be ordered if needed. Early diagnosis is important to manage the condition and prevent or delay lung and liver damage.
Pulmonary function tests (PFTs), Sputum test (microscopy and culture), Chest X-ray or CT Chest, and Bronchoscopy are performed for diagnosis, and assessing airway and lung function, as well as the type of infection. In addition, complete blood cell counts (CBC), HIV test, and inflammatory markers for autoimmune diseases may be done.
TREATMENT
Bronchiectasis can’t be fully cured. Treatment focuses on managing symptoms, preventing infections, maintaining nutrition and general health, and improving lung function through antibiotics, mucus clearance techniques, and other therapies. Avoiding smoking, vaping, and exposure to environmental toxins as much as possible is important. The underlying condition should always be investigated, diagnosed, and treated. Rarely, surgery may be recommended.
- Antibiotics – To treat recurrent respiratory bacterial infections. One may have to change drug classes frequently or work with combinations to avoid antibiotic resistance and reduced treatment effectiveness. Macrolide antibiotics like azithromycin, roxithromycin, erythromycin, and clarithromycin can reduce inflammation in the airways in addition to helping fight certain bacteria, and may be prescribed for long-term use to reduce the frequency of exacerbations and improve quality of life.
- Expectorant and mucolytics- To break down, dilute, or thin mucus and help cough it out. Examples include N-acetylcysteine, bromhexine, ambroxol, guaiphenesin, acebrophylline).
- Bronchodilators – To help dilate airways to ease mucus expulsion. Examples include salbutamol, levosalbutamol, and terbutaline.
- Saline- As nasal sprays for nasal symptoms, and hypertonic saline to restore healthy salt balance in the lungs and help the productive cough.
- Specific medicines – Special drugs have been approved for certain conditions like CFTR modulators for CF (combination of correctors – elexacaftor/tezacaftor/lumecaftor and potentiator –ivacaftor, and triple combination – vanzacaftor, tezacaftor and deutivacaftor), and augmentation therapy for AATD, where purified AAT protein is infused to boost levels in the blood and lungs.
- New drug: A promising new drug for bronchiectasis, brensocatib, has recently received FDA approval. Brensocatib is an oral inhibitor of dipeptidyl peptidase 1 (DPP1) to reduce chronic lung inflammation and exacerbations, and is the first drug specifically approved for non-cystic fibrosis bronchiectasis.
- Physical therapy – Involves postural draining and chest percussion therapy to help loosen and remove mucus, and breathing exercises to help open up airways.
- Medical devices – Include oscillating positive expiratory pressure (PEP) devices and percussive vests to break up and pull mucus out from the lungs.
- Vaccination – Pediatric vaccination schedule should be up to date, and important adult vaccines include annual flu vaccine, pneumococcal vaccination, Tdap, and MMR, as these diseases can worsen bronchiectasis.
The overall outlook will depend on how severe the condition is, how well the response to treatment is, and what other health conditions are present. With proper treatment, most people with bronchiectasis can expect to live as long as someone without it (history of smoking and low lung function are known to lower your life expectancy).
Also read: