What is Fatty Liver
When the amount of fat deposition in the liver exceeds 5% it is classified as fatty liver. It is also called steatotic liver disease or hepatic steatosis. Usually, 5-10% fat deposit in the liver does not cause inflammation or damage, and therefore is classified as grade 0 steatosis.
What are the Types of Fatty Liver
There are two main types:
NONALCOHOLIC FATTY LIVER DISEASE (NAFLD)
NAFLD, now called Metabolic associated fatty liver disease (MAFLD) or Metabolic dysfunction- associated steatotic liver disease (MASLD), is seen in people who have daily alcohol consumption below 10g but have other metabolic risk factors. When fat deposition in the liver exceeds 10%, and more and more fats accumulate, it can cause inflammation of the liver cells (hepatocytes), and the condition is called steatohepatitis (NASH/MASH). Inflammation and liver cell damage can cause fibrosis, or scarring, of the liver, and NASH can lead to the development of cirrhosis, which can further increase the risk of liver failure as well as liver cancer.
ALCOHOLIC LIVER DISEASE (ALD)
Alcoholic liver disease is due to heavy alcohol use. Too much drinking causes a load on the liver cells to metabolize alcohol inhibits the breakdown of fats (fatty acid oxidation) and also releases substances that are harmful to the liver. Therefore, fat deposition occurs in the liver which progresses to liver inflammation (alcoholic steatohepatitis) over time ultimately resulting in cirrhosis and liver failure, as well as increased chances of liver cancer.
Who is at Risk for Fatty Liver Disease
Too much drinking and alcohol abuse is the cause of alcoholic liver disease (ALD).
The cause of nonalcoholic fatty liver disease (NAFLD) is unknown, however, certain risk factors have been identified:
• Type 2 diabetes
• Obesity and high BMI, especially excess fat around the waist
• High cholesterol or triglycerides
• High blood pressure
• Metabolic or thyroid disorders
• Overuse of certain drugs, medications containing metals and toxins, or unregulated herbs
• Family history or genetic predisposition
How is Fatty Liver Disease Diagnosed
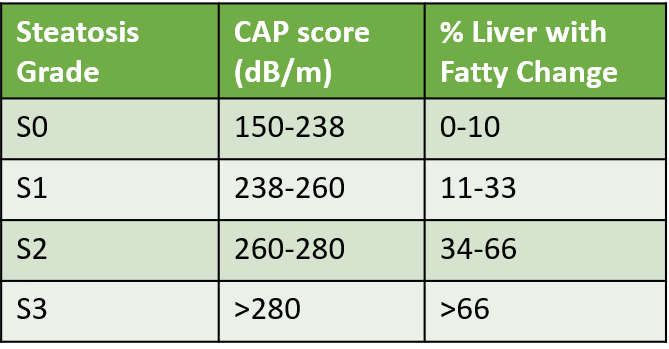
There are usually no symptoms of Fatty Liver Disease till the stage of inflammation is reached (hepatitis) or cirrhosis develops. It may be picked up if one is screened by an ultrasound test called FibroScan (CAP score) due to the presence of mentioned risk factors. Usually S1 grade onwards, some amount of inflammation and damage may begin in the liver.
Other tests include blood lipid profile for cholesterol and triglycerides, and liver function tests for liver enzymes alanine aminotransferase (ALT), aspartate aminotransferase (AST) and gamma-glutamyl transferase (GGT), along with blood sugar, and thyroid profile.
Fatty Liver Index (FLI) is an algorithm combining body mass index (BMI), waist circumference (WC), gamma-glutamyl transferase (GGT), and triglyceride (TG) levels, and has been demonstrated to be a useful tool to predict the presence of NAFLD, since it shows high correlation with imaging as well as biopsy criteria for NAFLD.
How to Treat Fatty Liver and Prevent Progression
Management includes:
• Quitting alcohol use and smoking
• Healthy diet
• Weight loss: Even a 3-5% weight loss can significantly cut the risk of progression to hepatitis stage.
• Managing and effectively controlling risk factors with appropriate lifestyle and medicines: like diabetes, hypertension, cholesterol-triglycerides, and thyroid disorders.
• Regular Exercise: For at least 30-45 minutes regularly like brisk walking, cycling, swimming, yoga or aerobics.
• Stress management
• Stopping drugs and unregulated supplements under medical guidance that can be a possible cause.
• Vaccinations for Hepatitis A, and B.
• Regular follow-up and FibroScan ultrasound to check for progression
Medicines mainly include supplements that increase the oxidation of fatty acids, reduce inflammation of the liver and have anti-oxidant action. There are many supplements available, however, none are curative or can completely prevent progression. Some of these supplements include carnitine, inositol, vitamin E, silymarin, curcumin, omega 3 fatty acids, resveratrol, coenzyme Q10, and pre-probiotics. ALD and MAFLD currently have no specific medicines, though supportive therapy with tonics, nutritional supplements, and antioxidants is often prescribed. Research on specific drugs is in progress. Saroglitazar has recently been approved in India as a specific drug for NASH. Resmetirom a drug that helps to reduce fat production, increase the breakdown of fatty acids, and decrease liver fat content, was approved by FDA in March 2024 for MASH and liver scarring due to steatosis. Antidiabetic drugs and vitamin E are also used in managing various stages of MAFLD. Treatment and management of underlying risk factors is the cornerstone.
Also read:

