Glomerulonephritis
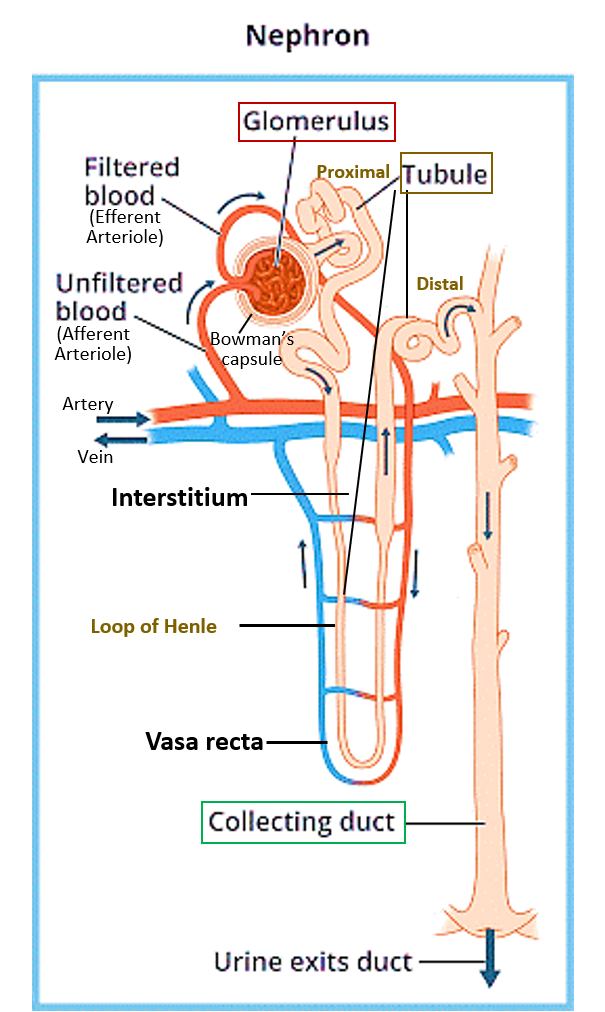
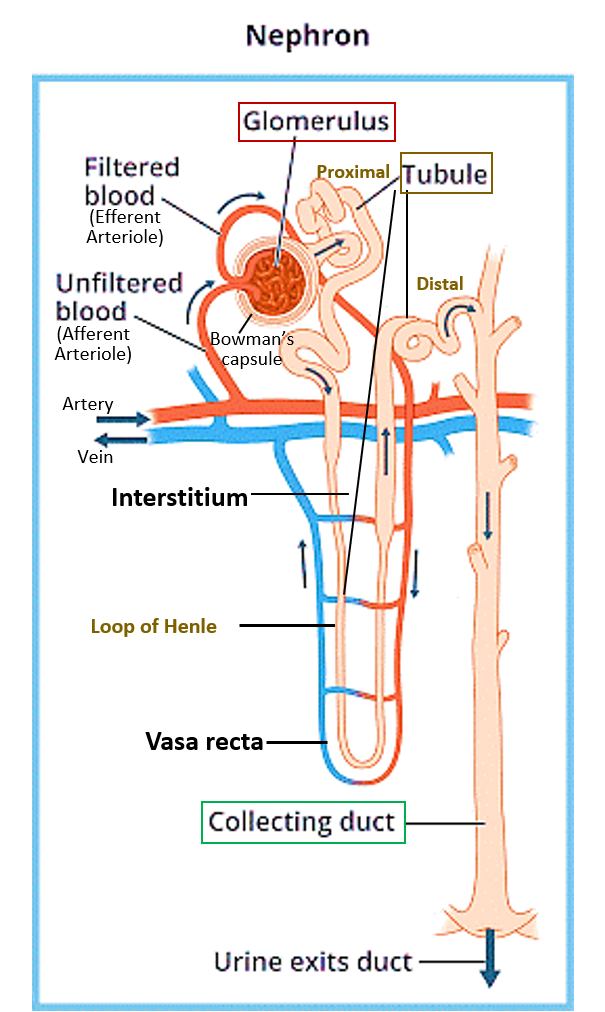
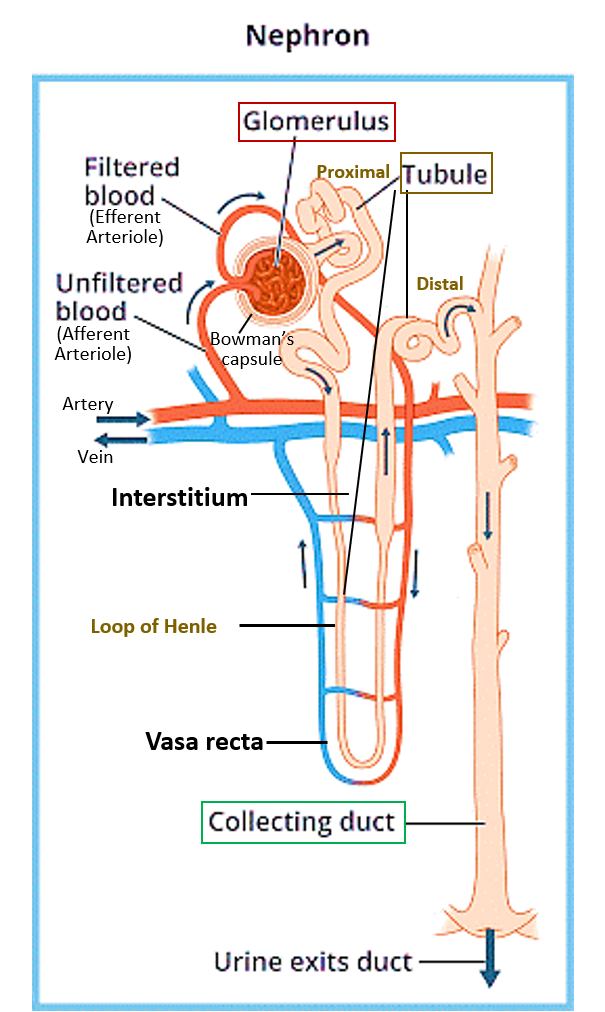
Glomerulonephritis is the inflammation of the glomerulus which is the network of capillaries inside the cup (Bowman’s capsule) of the kidney cells called nephrons. The glomerulus is responsible for filtering wastes from the blood, to form urine. Therefore, when it gets inflamed, the capillary vessel walls become more leaky.
Glomerulonephritis can occur suddenly (acute) or over a period of time (chronic).
Read – Structure, and Function of Kidneys
SIGNS AND SYMPTOMS
Sometimes initially there may be no symptoms, especially in the chronic form. Since the glomerulus becomes more leaky due to the inflammation, initially substances normally not filtered by the kidney, are found in urine.
In cases of early initial stage (the non-proliferative stage), proteins leak through and are found in urine making the urine foamy. This may initially go undetected unless a urine test is done routinely. Swelling on the face in the mornings is an early sign, especially in children. Significant protein loss in urine can lead to a fall in blood proteins leading to swelling of hands, legs, face, and abdomen. This is called nephrotic syndrome. Sometimes fats may also be passed in urine giving it a milky look (lipiduria).
Ongoing damage to the glomerulus can lead to the proliferative stage, where there is blood (red blood cells -RBCs) in the urine, called hematuria. Due to uncontrolled filtration, as a reflex, the RAAS system (a hormonal regulatory system for blood pressure and fluid-electrolyte balance) gets activated and causes increased blood pressure, and reduced blood flow to the kidney. This leads to fluid retention and a further increase in swelling, along with a reduction in urine volume (less urination). High blood pressure and hematuria characterize the nephritic syndrome. Other symptoms may include nausea-vomiting, cramps, and fatigue.
Over a period of time fluid-electrolyte balance gets disturbed and wastes accumulate in the blood (raised blood urea nitrogen, and creatinine). This can ultimately lead to kidney failure that may be acute (rapid and transient especially seen in infections, and often shows recovery) or chronic (decreased kidney function for 3 months or more). Chronic kidney disease (CKD) may advance to end-stage kidney disease, which requires either dialysis or a kidney transplant.
CAUSES
There are many causes, that include infections, autoimmune conditions and other diseases.
Infections
The most well-known is associated with the Streptococcal bacterial infection and happens a week or two after a throat infection, especially in children or rarely a skin infection. It is actually the antibodies formed by the body against the Streptococcal bacteria that cause the glomerular inflammation. A condition called bacterial endocarditis is an infection of the inner lining of the heart’s chambers and valves, that can also cause inflammation of the glomerulus. Viral infections of the kidney by hepatitis virus B/C and HIV, and others like malaria can also cause glomerulonephritis.
Autoimmune diseases
Autoimmune diseases are conditions caused by the immune system attacking one of our body’s own proteins, considering it as foreign due to an immune recognition error. Lupus (systemic lupus erythematosus) is one such condition that can affect the skin, joints, kidneys, blood cells, heart and lungs. A specific and rare condition called Goodpasture’s syndrome creates antibodies against the basement membrane of the capillaries of the lung and glomerulus in the kidneys. Another condition causing glomerulonephritis is IgA antibodies that are produced against some infections but end up damaging the glomeruli (IgA nephropathy).
Other Diseases
High blood pressure and diabetes are two chronic conditions that cause gradual damage to the walls of blood vessels and can also therefore cause chronic glomerulonephritis. Glomerulonephritis further can cause high blood pressure and set up a vicious cycle in people with hypertension. Damage to the kidneys due to diabetes is called diabetic nephropathy.
Vasculitis refers to conditions that cause inflammation of small and medium blood vessels across the body, including the glomerulus. These include polyarteritis (affects vessels of kidneys, skin, muscles, joints, and gut), and granulomatosis with polyangiitis (formerly known as Wegener’s granulomatosis that affects vessels of the lungs, upper airways and kidneys).
Amyloidosis is a disorder in which abnormal proteins build up in tissues and organs, and these can deposit in the glomeruli and damage them over a period of time. Cancers like leukemia, stomach and lung cancers can also cause glomerulonephritis.
Drugs like NSAIDs and some antibiotics can sometimes trigger transient glomerulonephritis. Sometimes the cause may not be determined despite investigating thoroughly. Rarely it may be genetic and run in families.
DIAGNOSIS
A routine single sample urine test will show red blood cells, increased white blood cells and proteins in urine. A 24-hour urine collection and testing may show a lowered urine volume and also help estimate creatinine clearance and total protein loss.
Blood tests are done to estimate if creatinine, as well as urea and nitrogen (BUN) levels are raised in blood suggesting reduced kidney function. Blood tests also check for blood counts for evidence of anemia or infection, total proteins with albumin and globulin ratios, electrolyte levels, as well as blood sugar levels. Specific antibody marker tests may be done for suspected conditions.
From the creatinine values based on age, gender, weight and race, an estimated glomerular filtration rate (eGFR) can be calculated, which gives an idea of the filtering function of the glomerulus. The values are given as % of what is normal for that age, gender, weight and race.
Based on clinical examination and blood-urine tests, additionally an imaging of the kidney by ultrasound or CT/MRI may be advised, and in some cases a kidney biopsy may also be needed to make a specific diagnosis.
TREATMENT
Treatment of glomerulonephritis consists of 3 parts –
- general care
- treating the underlying cause
- managing loss of kidney function.
In most cases 1 and 2 take care of the 3rd and the kidney function improves spontaneously, however in some cases the kidney function may deteriorate progressively.
General care
This includes dietary changes like reducing the amount of salt, fat, protein and potassium in diet, restricting fluid intake, and stopping smoking. One should have regular health check-up for blood pressure. In such patients often immunity is compromised, so they should receive the flu and pneumococcal vaccines.
Treating underlying cause
Infections should be treated, with appropriate antibiotics for bacterial infections like streptococci, and antiviral drugs for hepatitis and HIV. Blood pressure and diabetes should be meticulously controlled. Blood cholesterol and triglycerides if raised should also be treated. Certain drugs called diuretics may be given to reduce fluid build-up and swelling.
Vasculitis or autoimmune conditions should be treated with a course of oral or injectable corticosteroids or other immune-suppressive drugs. Plasma exchange (plasmapheresis) is an intervention sometimes used where the patient’s plasma is exchanged with a similar fluid in an external machine and that fluid put back in the patient’s body. It temporarily removes certain immune factors that are causing damage. The fluid put back may be donor plasma, albumin, or a combination of albumin and saline
Managing loss of kidney function
Kidney failure is the loss of 85% or more of kidney function determined by eGFR of 15% or less. This requires a procedure called dialysis where an external machine filters out the wastes from the body.
Acute kidney failure due to infection usually recovers and patient can be off dialysis after recovery. However chronic kidney disease (CKD) or failure requires dialysis on long-term basis till a kidney transplant can be done.
Nephrotic Syndrome due to Minimal Change Disease
Minimal change disease is the most common cause of nephrotic syndrome in children. It causes foamy urine with swelling of the face most noticeable in the mornings, followed by swelling in the abdomen and other parts. In minimal change disease, examination of kidney tissue on biopsy under a microscope appears normal or nearly normal, and no obvious glomerular inflammation is evident. The cause is not known and the condition shows prompt response to a course of corticosteroids like prednisolone. There is usually complete resolution without any loss of kidney function, and recurrences are rare.
Also read:
Tubulointerstitial nephritis – Causes, Diagnosis and Treatment
Chronic Kidney Disease (CKD) – 5 Key Points of Understanding