Congenital heart defects (CHD) are abnormalities in the structure and functioning of the heart that are present at birth due to genetic or developmental errors inside the womb. Congenital heart defects can manifest at birth, in infancy, childhood, or sometimes even in late teens or adulthood, based on the type and severity of the heart defect, and the lifestyle and physical activity of the person affected.
Congenital heart defects should be detected in time, and appropriate action should be taken, so as to give long-term quality of life to the child, and also reduce the risk of heart failure, recurrent hospitalization, and mortality.
The normal structure and functioning of the heart are shown below.
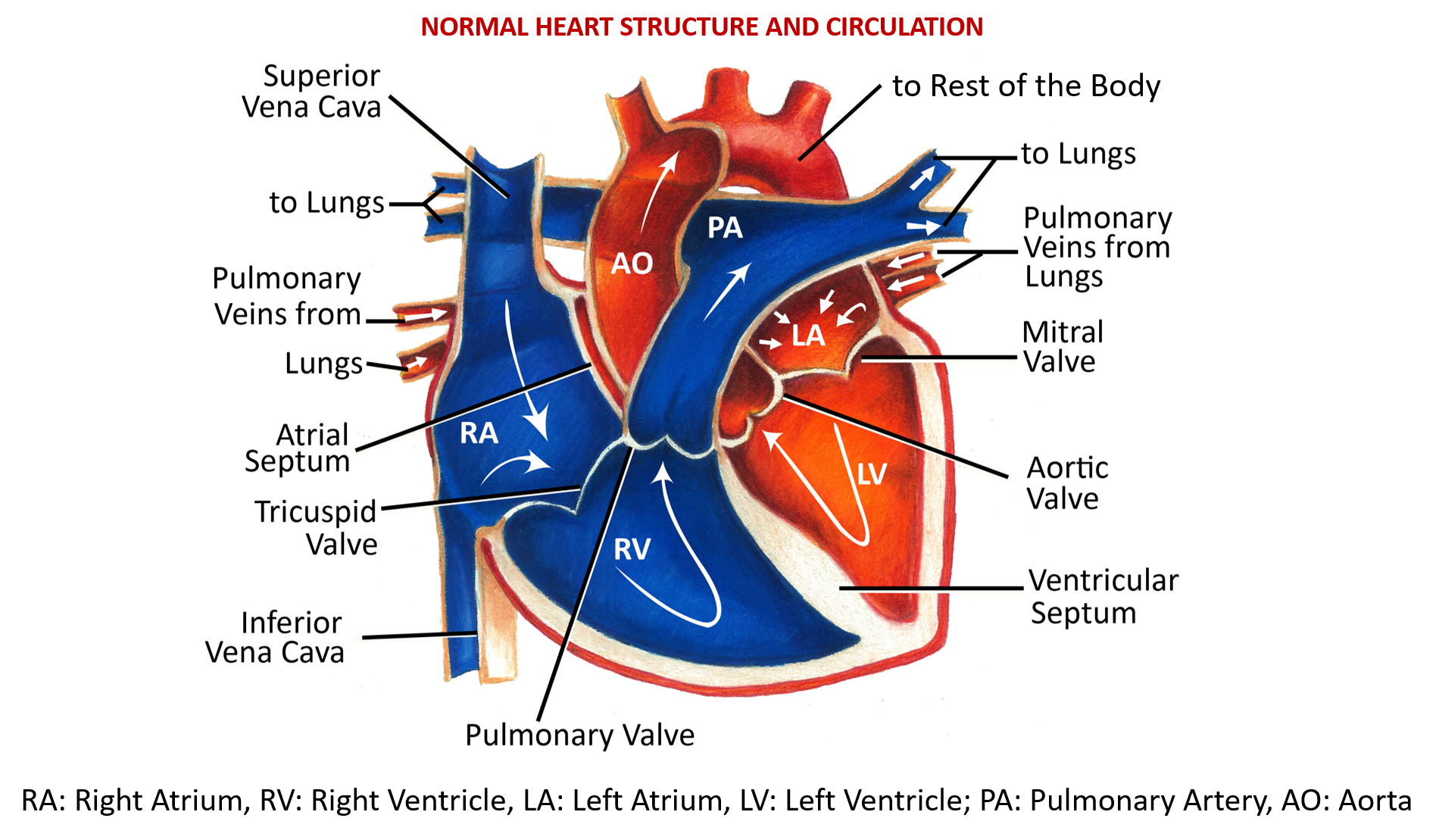
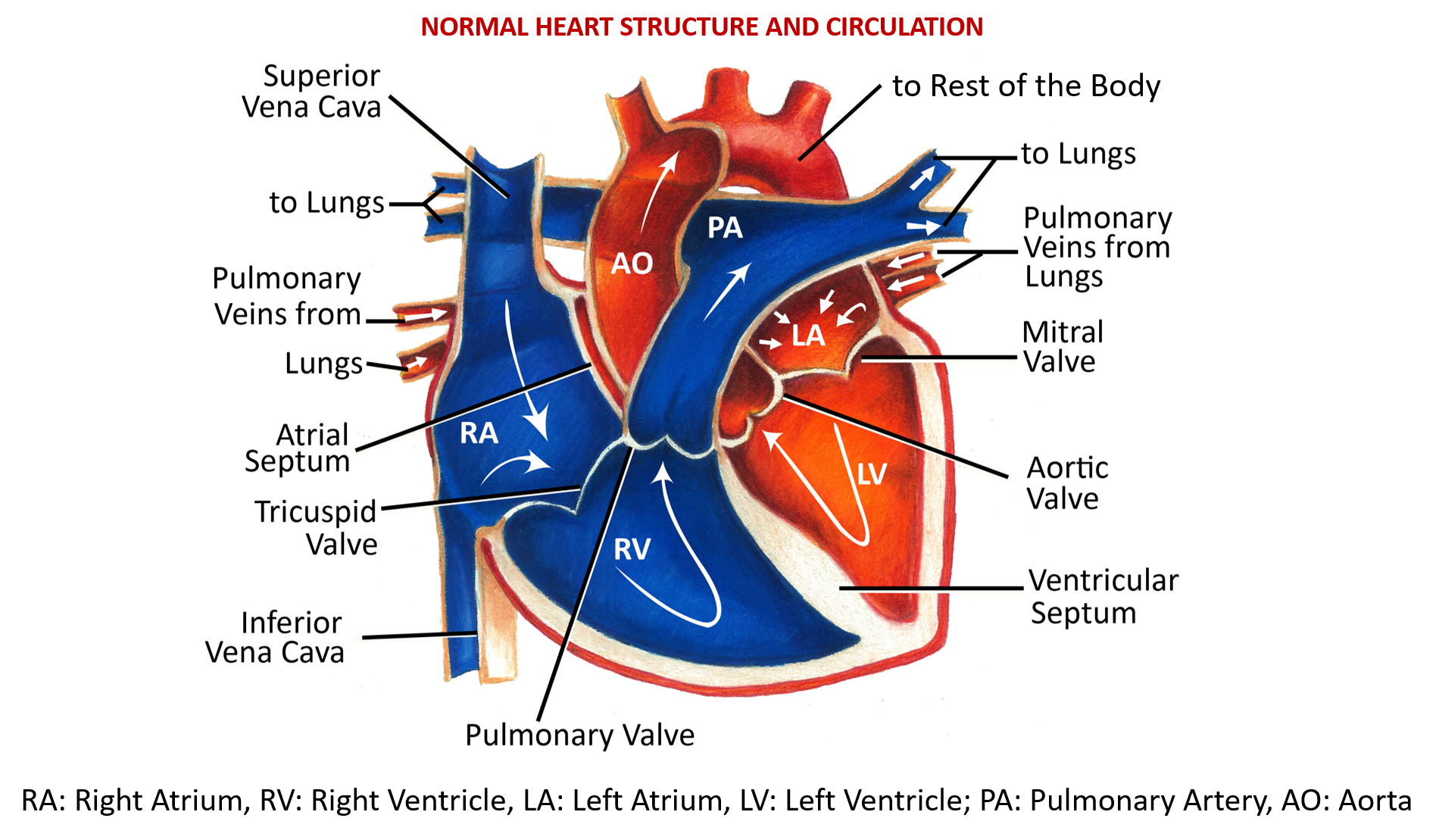
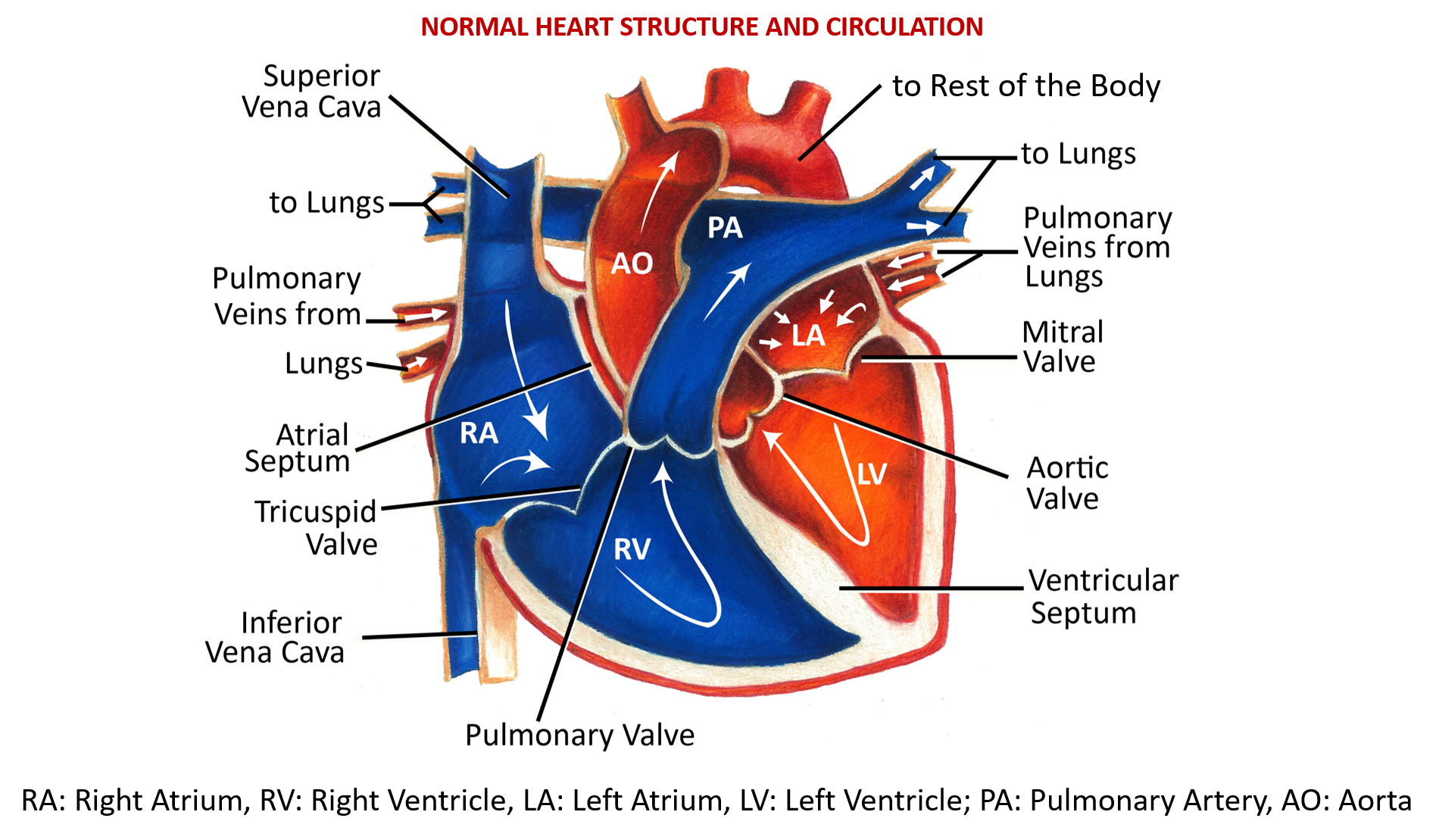
Oxygen-poor (deoxygenated) blood from all parts of the body enters through the superior and inferior vena cava into the right upper chamber of the heart (right atrium) and goes to the right lower chamber (right ventricle) through an opening controlled by the tricuspid valve. The right ventricle pumps this blood to the lungs through the pulmonary artery, the opening of which at the right ventricle is controlled by the pulmonary valve.
Oxygen-rich (oxygenated) blood from the lung reaches the left upper chamber (left atrium) of the heart, through the pulmonary veins. This blood then enters the left lower chamber (left ventricle) through an opening controlled by the bicuspid (mitral) valve. The left ventricle then pumps the oxygen-rich blood to all parts of the body through the aorta, the opening of which in the left ventricle is controlled by the aortic valve.
Therefore, oxygen-rich and oxygen-poor blood from the left and right side of the heart, or from the two main outgoing vessels (aorta and pulmonary artery) respectively, do not normally mix after birth. Such mixing may happen due to openings or connections when the baby is in the womb, but these close at or shortly after birth.
In congenital heart defects, such mixing continues to happen due to defects in the heart wall and septa (partitions between chambers), abnormal valves, and abnormal connections or positions of the main arteries leaving the heart. This leads to a reduced supply of oxygen to the body and causes various clinical symptoms. This also increases the pumping load on the heart which can eventually lead to heart failure if not surgically corrected in time.
Symptoms of Congenital Heart Defects
- Shortness of breath (prominent during exertion or physical activity)
- Fast or heavy breathing
- Tiredness (noticeable in infants while feeding)
- Dizziness, sweating or fainting spells
- Poor weight gain and development
- Frequent respiratory infections
- Sense of palpitations or skipped heartbeats
- Pale or bluish appearance
- Swelling of legs, feet, or abdomen
Diagnosis and Management
During a physical examination, the doctor may hear a distinct whooshing sound, called a heart murmur, that has distinct characteristics based on the type of heart defect.
The most common diagnostic test is an echocardiogram (ultrasound of the heart) that shows the type of abnormality, as well as the amount of blood flowing through or compromised due to the defect.
Treatment is always by corrective heart surgery. Long-term meticulous post-surgery follow-up is very important, and in many cases, multiple and multi-stage surgeries may be needed. Supportive nutrition and medicines to manage blood pressure and fluid overload are also given.
TYPES OF CONGENITAL HEART DEFECTS
SEPTAL DEFECTS
These are defects in the structure of the heart wall, especially the dividing walls (septa) between different chambers of the heart. They are commonly termed ‘hole in the heart’.
Ventricular Septal Defect (VSD) – This is the most common of septal defects. It is a hole in the wall (septum) that separates the two lower chambers (ventricles) of the heart.
Atrial septal defect (ASD) is a hole in the wall (septum) that divides the upper chambers (atria) of the heart.
Atrioventricular septal defect (AVSD) is a combined heart defect affecting the valves between the heart’s upper (atria) and lower (ventricle) chambers and the walls (septa) between these chambers.
Septal defects may be small or partial, and may even close on their own. Larger, complete, or persistent defects require surgery done by either cardiac catheterization or open-heart surgery to close the hole with a patch and restore normal blood flow. Septal defect surgeries usually ensure future healthy lives. However regular follow-up is important. Valvular repairs are needed in AVSD, and these cases need to be meticulously monitored long-term for future valve leakage and complications.
VALVULAR DEFECTS
Pulmonary Atresia
This is a birth defect of the pulmonary valve, that controls the entry of blood from the right ventricle into the pulmonary artery taking blood to the lungs for oxygenation.
The blood flow finds alternate routes out of the right ventricle through persistent openings and connections that were present when inside the womb, like the foramen ovale, an opening between the right and left atria that exists in the fetus and closes at birth. Another route is the ductus arteriosus (opening between the aorta and pulmonary artery, the two major outgoing blood vessels from the heart, which again is a normal part of a baby’s circulatory system in the womb but usually closes shortly after birth.
Medications (PGE1) are often given to keep the ductus arteriosus open after birth (patent ductus arteriosus), till the pulmonary valve can be made functional by surgery that involves stenting, valve expansion, or replacement. Regular long-term follow-up is essential, and possible later surgeries may also be needed.
Tricuspid Atresia
It is a birth defect of the tricuspid valve, which controls blood flow from the right atrium to the right ventricle, so the blood is unable to get to the right ventricle and out to the lungs. This defect may be accompanied by an underdeveloped right ventricle and pulmonary artery. Also present may be an ASD or VSD, that help as compensatory mechanisms for blood flow.
A patent ductus arteriosus may also help as an alternate route for blood flow so medicines for the same may be given. Early and multi-stage surgeries, with long-term, follow up are required.
VASCULAR DEFECTS
Coarctation of the Aorta
It is a birth defect in which a part of the aorta, that carries oxygen-rich blood from the left ventricle to the body, is narrower than usual, just after the branches to the upper body (head-neck, arms) are given off. The narrowing reduces blood flow to the lower body and creates back pressure and load on the left ventricle that can lead eventually to heart failure. Coarctation can lead to normal or high blood pressure and pulsing of blood in the head and arms and low blood pressure with weak pulses in the legs and lower body.
Coarctation of the aorta often occurs with other congenital heart defects. The narrow aorta will need to be widened once symptoms are present, by balloon angioplasty during cardiac catheterization and a stent used to keep the aorta wide. Surgery to remove the narrow portion and reconstruction or patching to allow normal blood flow is done.
Transposition of the Great Arteries (TGA)
The two main arteries carrying blood out of the heart – the pulmonary artery and the aorta, are switched in position, or transposed. The aorta is in front of the pulmonary artery and is either mainly to the right (dextro) or to the left (levo) of the pulmonary artery. Dextro-TGA (d-TGA) is far more common. Due to this, de-oxygenated (oxygen-poor) blood from the right ventricle gets pumped to the body through the aorta, and oxygenated (oxygen-rich) blood from the lungs is pumped back into the lungs through the pulmonary artery.
ASD and VSD may sometimes be co-present as compensatory mechanisms. The patent ductus arteriosus also allows some oxygen-rich blood to be pumped to the rest of the body. It is corrected by arterial switch or atrial switch surgery.
Total Anomalous Pulmonary Venous Return (TAPVR)
It is a birth defect of the heart where oxygen-rich blood does not return from the lungs to the left atrium. Instead, the oxygen-rich blood returns to the right side of the heart and mixes with oxygen-poor blood. ASD is often co-present as a compensatory mechanism.
Surgical repair of TAPVR is to restore normal blood flow through the heart by connecting the pulmonary veins to the left atrium and patching the ASD and any abnormal connections between blood vessels. Multistage surgeries may be needed with regular follow-up.
Truncus Arteriosus
The blood vessel coming out of the heart in the developing baby fails to separate completely during development, leaving a connection (a common trunk – truncus arteriosus) between the aorta and pulmonary artery. It is associated with VSD.
Here the right side of the heart pumps oxygen-poor blood through the pulmonary artery to the lungs. The left side of the heart pumps oxygen-rich blood through the aorta to the rest of the body. But due to the truncus arteriosus, oxygen-poor blood and oxygen-rich blood are mixed together as blood flows to the lungs and the rest of the body. As a result, too much blood goes to the lungs and the load on the heart to pump blood to the rest of the body increases.
Also, instead of having a separate aortic valve and a pulmonary valve, babies with truncus arteriosus have a single abnormal, often leaky common valve (truncal valve) controlling blood flow out of the heart.
Usually, surgery to repair this defect involves closing the VSD, creating a new aorta from the truncus to the left ventricle, and connecting the right ventricle to the lung with an artificial conduit. Multistage surgeries may be needed with regular follow-up.
COMBINATION OR MULTIPLE DEFECTS
Tetralogy of Fallot (ToF)
Tetralogy of Fallot is made up of the following four (tetra) defects of the heart and its blood vessels: VSD, narrowing of the pulmonary valve and pulmonary artery (pulmonary stenosis), an aortic valve sitting on the VSD causing the aorta to open out from both ventricles, and thickening (hypertrophy) of the right ventricle. This heart defect also, therefore, causes reduced oxygen in the blood flowing to the rest of the body.
Tetralogy of Fallot can be treated by surgery to widen or replace the pulmonary valve and enlarge the passage to the pulmonary artery, with a patch over the VSD. Outcomes are usually good, but regular follow-up is always required.
Hypoplastic Left Heart Syndrome
This refers to an underdeveloped left ventricle, its mitral and aortic valves, as well as the portion of the aorta ascending out from it. There may be an associated ASD as well. The left side of the heart in such cases cannot pump oxygen-rich blood to the body properly.
The child may require multiple corrective surgeries at different stages and ages. Infants with hypoplastic left heart syndrome may have lifelong complications and need regular follow-up. In some cases, the heart becomes weak after the surgeries, and a heart transplant may be needed.
Also read:
Inflammation of Heart Layers (Carditis) – Pericarditis, Myocarditis, Endocarditis


