Hypopigmentation is a patch of skin that is significantly lighter than the surrounding skin. Hypopigmentation occurs due to a reduction in synthesis of the skin pigment ‘melanin’.
Leukoderma, (also called achromoderma) refers to localized areas of white (leuko) depigmented skin due to total loss of melanin. In common parlance, it usually refers to vitiligo.
A lack of melanin synthesis can occur due to a genetic mutation causing an abnormality in the melanin synthesis pathway, as seen in albinism. Hypopigmented patches (macules) can occur due to the destruction of melanin-producing cells (melanocytes) resulting from immune-mediated or inflammatory mechanisms, skin diseases, or skin injury.
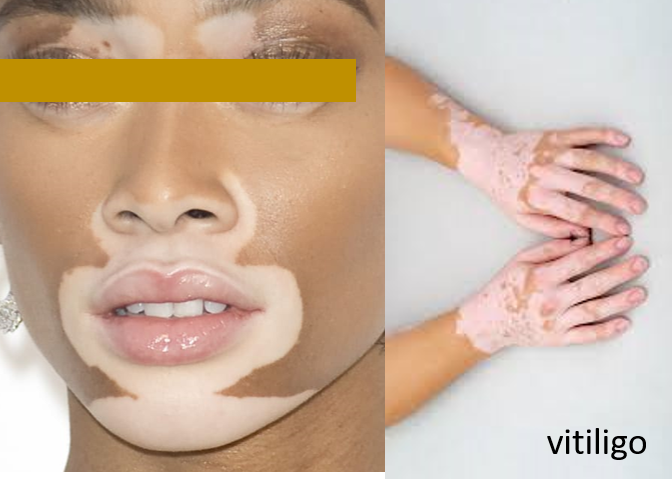
VITILIGO
Vitiligo presents as hypopigmented patches that usually start before the age of 30, and may then progress with time. These patches can be present throughout the body (generalized) on both sides (symmetrical) or one side (segmental), or in a particular area (localized/focal) like the face, in and around the mouth, hands, trunk, or legs. It can also affect the hair including eyebrows and eyelashes. The cause is the destruction of melanocytes due to a complex mechanism that could be possibly inflammatory or immune-mediated, and may be hereditary or triggered by stress or skin injury.
Medicines available currently, are unfortunately not curative or highly effective. These treatments also take time to produce visible or sustained results and skin darkening, which may take many months. Most of these medicines act by reducing inflammatory or hyper-immune responses, both implicated as mechanisms for vitiligo. Often different groups of medicines may be combined for better results. Few of these medicines are applied as topical patches after a dermabrasion or needling procedure. Some of these medicines may also be combined with UV light and laser therapy.
- Corticosteroids: Prescribed as creams/ointments and less commonly as pills/injections.
- Vitamin D3 analogs: Calcipotriol as a topical cream is usually used in combination with corticosteroids.
- Calcineurin inhibitors: These are immune modulators and suppressants that include topical agents (TCI) tacrolimus or pimecrolimus, used as ointments under caution due to side effects and long-term skin cancer/lymphoma risk (reserved more for localized vitiligo on the face).
- Immune suppressants: These include methotrexate (oral/gel), 5 fluorouracil (5FU gel), cyclosporine (oral), and azathioprine (oral).
- JAK inhibitors: They act by immune modulation and were developed for rheumatoid arthritis. They are available as creams (ruxolitinib, tofacitinib) and as tablets (tofacitinib).
- Deca Peptide is a re-pigmenting agent. It works by causing the migration of skin cells (melanocytes) from the area of skin surrounding the vitiligo patch, leading to the production of melanin to restore the skin colour. It is to be applied as a thin layer to the pigmented areas of skin and rubbed into the vitiligo patch gently. Since it makes the skin more sensitive to the sun, a sunscreen and protective clothing when outdoors are needed.
- Anti-oxidant enzymes and agents: These include catalase/pseudocatalase, superoxide dismutase, glutathione, and vitamin C/E/B12. These remove free radicals or reactive oxygen species-ROS, a possible cause of melanocyte destruction. They are also used as creams or tablets, with limited success but without risk of side effects.
- Prostaglandin F2 analogs: These include latanoprost and bimatoprost They are used to improve melanin synthesis and skin coloring.
- Afamelanotide: This medicine is implanted under the skin and is similar to melanocyte-stimulating hormone promoting the growth and development of melanocytes.
- Apremilast: It acts as an oral anti-inflammatory agent and was originally developed for psoriasis.
- Minocycline: It is an antibiotic that helps to protect melanocytes by reducing oxidative stress and destruction. It may help in the early stages.
- Phenylalanine is the precursor amino acid for melanin synthesis. It has been used orally but requires very high doses – up to 6-10g/day. So recently it has been explored topically as a 10% concentration.
Light therapy (phototherapy): It is the most effective among treatments available for vitiligo. Narrowband ultraviolet B (UVB) usually given 2-3 times/week and frequently combined with corticosteroids or calcineurin inhibitors can help slow progression, though it may take a few months to see visible sustained effects. Alternatively, photochemotherapy with UVA treatment can be given after oral intake or skin application of an activating chemical called methoxalen (psoralen). Transient skin, irritation, and redness may be seen after UV therapies. Laser (excimer, erbium, CO2) can also be used for phototherapy sometimes in combination with UV therapy, and/or with the above medicines.
Herbs can be natural treatments for vitiligo. These include Picrorhiza kurroa and Polypodium leucotomos given orally, both of which have antioxidant and immune-modulating activities and have shown to improve the results of phototherapy when used together. Gingko biloba is also available orally and has been shown to attenuate oxidative stress and scavenge superoxides that damage melanocytes. Nigella Sativa has been seen to show re-pigmentation in vitiligo and is available as a 10% seed oil extract. Green tea extract – Epigallocatechin-3-gallate (EGCG) has anti-inflammatory, antioxidant, and immunomodulatory properties, and is being explored as a 5% hydrophilic EGCG cream in vitiligo. Piper nigrum extract and its main alkaloid, piperine, promote melanocyte proliferation, and can benefit vitiligo patients in combination with Nigella sativa. Khellin is a herb that was used earlier in oral vitiligo treatment but was limited due to its potential for liver toxicity. So now it is used topically as a 5% extract in combination with nigella sativa and sometimes phenylalanine. Curcumin melo gel (rich in superoxide dismutase) was available in India but results in studies have been inconsistent.
Cosmetic concealing of vitiligo patches especially on the face with make-up is usually a satisfactory day-to-day option. There are self-tanning or sunless tanning agents (the approved one being the color additive dihydroxyacetone – DHA), which when applied, cause temporary skin darkening for a few days by reacting with the dead skin cells. Vitiligo patches should be protected from the sun by an SPF 30+, PA+++ sunscreens. In the case of large vitiligo patches, rarely depigmenting creams for normal skin may be given.
There are also social forums, help groups and counseling services available for people with vitiligo to better cope both practically and psychosocially.
Skin-grafting or transplantation are available in advanced centers.
PITYRIASIS ALBA
This is one of the most common and least concerning causes of white or hypopigmented patches, most commonly on the face. It is seen more in children and adolescents. The cause is not known but it is believed to be a form of mild dermatitis that causes local and transient damage to melanocytes, decreasing pigmentation. There may sometimes be a personal or family history of allergies (atopic dermatitis, asthma, or allergic rhinitis). The white spots may in some cases be preceded by a rash.



Usually, no treatment is needed and spontaneous resolution occurs in most cases in a few weeks to months. In select cases, anti-inflammatory agents like mild (low potency) corticosteroids like hydrocortisone with/without calcipotriol may be prescribed. In severe or persistent cases, calcineurin inhibitors or very rarely phototherapy is given.
INFLAMMATORY DERMATOSIS
These are various skin conditions that produce rash and itching and may leave behind hypopigmented patches after resolution, due to the intense inflammation causing local destruction of skin cells including melanocytes. This is sometimes seen in eczema, atopic dermatitis, and psoriasis, as well as acne.
INFECTION
A fungus called Malassezia can cause a skin infection that causes dark and white patches to develop on the skin due to pigment irregularity (Pityriasis versicolor). It is treated with topical antifungals. Herpes Zoster is a viral skin and nerve infection, that can also leave behind hypopigmented patches. Sometimes a boil or a blister after draining can also leave a transient hypopigmented patch. Parasitic/worm infestations should also be considered as a possible cause in tropical rural areas.
Leprosy may also be a cause of hypopigmented patches especially in regions where this disease is still prevalent. Leprosy is caused by infection with the bacterium Mycobacterium leprae. It mainly affects the skin, nerves, eyes, and nose. Symptoms include light-colored or sometimes red skin patches with the hallmark being reduced sensation or numbness in the affected area. The skin and nerves of the limbs are commonly affected and there may be accompanying weakness in hands and feet. Leprosy can be cured with timely 6-12 months of multi-drug therapy.
LICHEN SCLEROSUS
It presents as areas of thin, stretched-out, light-colored, and wrinkled skin. It is seen most commonly in postmenopausal women, so hormonal imbalance may be an underlying mechanism. It may also occur in children and men, and there may be a family history. Apart from hormonal imbalance, skin trauma or an immune-mediated response may also be underlying mechanisms. People with other autoimmune disorders, (like hyperthyroidism, diabetes type 1, vitiligo, etc.) are more at risk of having lichen sclerosus.
It affects the external genitals, and sometimes the mouth, neck, shoulder, breast, thighs or anus. It can produce itching, dryness, irritation, and pain, along with a rash. Complications can include local bleeding, skin bruises or tears, and the formation of painful blisters. It can lead to pain during intercourse, urination or passing stool in case of genital or anal involvement. It can also cause narrowing of the vagina in women due to scarring, or shrinking of the foreskin and impaired retraction in men. Genital lichen sclerosus is associated with a higher skin cancer risk than the general population.



It is usually treated with local application of corticosteroids, and in severe or non-responding cases, local steroid injections. Rarely stronger agents like calcineurin inhibitors, etc. may be needed. Medications for pain are given when required. Lifestyle measures include avoiding tight-fitting or synthetic clothing, cosmetics, soaps/detergents, and fragrant sprays in the affected area, and maintaining hygiene by gently washing and patting dry the part. Circumcision is advised in males.
SKIN TRAUMA
Burns are a common cause of hypopigmented patches as large areas of skin including melanocytes are destroyed. This may also be seen in scars after an extensive skin injury, after skin procedures like laser, peels, etc, or after some skin bleaching or lead-based cosmetic use.
NUTRITIONAL DEFICIENCY
Vitamin and Mineral deficiency like that of Iron, Copper or Vitamin B12 should be ruled out. Malnutrition (like protein, carbs, and fats deficiency – Kwashiorkor and Marasmus) can cause hypopigmented patches in children from low-income or rural areas.
DRUGS
Some medicines like depigmenting agents, corticosteroids, retinoids and benzoyl peroxide that may be used for other skin conditions like acne, can also cause hypopigmented patches.
TUMORS
These are rare causes of hypopigmented patches. Tuberous sclerosis is a rare, genetic disease that causes non-cancerous (benign) tumors to grow in the brain, skin, eyes, and also kidneys, heart, and lungs.
Mycosis fungoides is a cutaneous T cell lymphoma (cancer of the T-lymphocytes a type of white blood cell in the skin) that classically causes a reddish-brown rash, but as a rarer variant can also present with hypopigmented lesions.
ALBINISM
This is caused by an inherited genetic mutation that leads to a defect that prevents melanin synthesis. The skin, as well as hair, are white or light-colored and the eye (iris) blue. Albinism can show a range of presentations involving just eyes (ocular); eye, skin, and hair (oculocutaneous); or be part of syndromes where other organs or the immune system also shows deficiencies (Chediak Higashi. Hermansky Pudlak, and Griscelli syndromes).
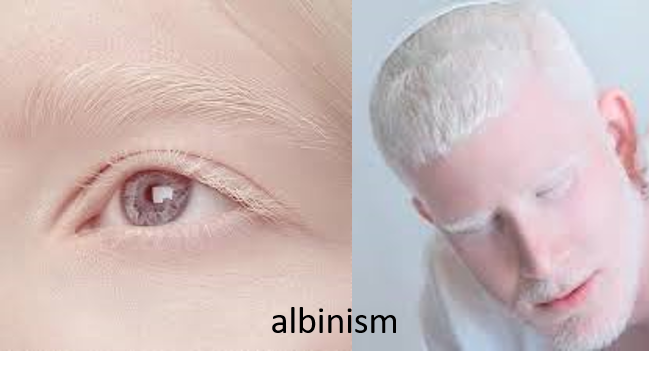
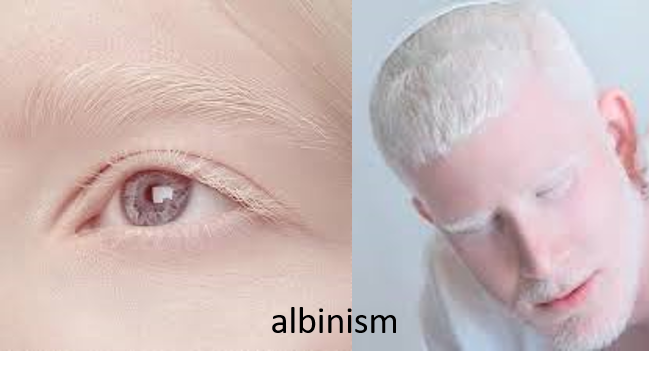
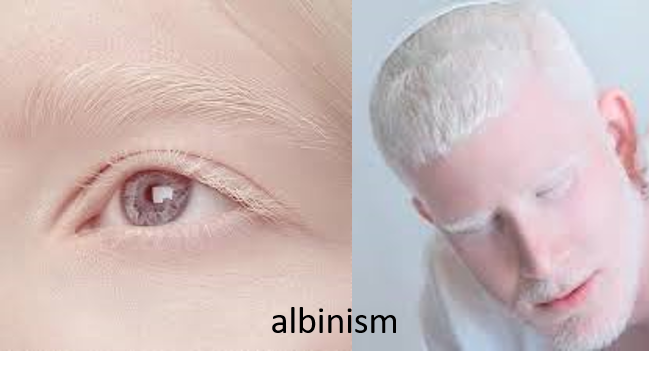
People with albinism should wear protective clothing and high 30-50+ SPF – PA+++ sunscreens, limit their outdoor activities, and also screen regularly for skin cancers for which they are at a higher risk than the general population. Albinos can have eye problems like squints, and refraction (astigmatism) that may require surgical correction and spectacles respectively. They may also have increased sensitivity to light (photophobia) needing glares, or rapid oscillatory eye movements (nystagmus) with impaired vision, requiring low vision aids and rehabilitation.
Also read:
Skin Infections – Types, Predisposing Factors and Health Measures
For any query, additional information or to discuss any case, write to info@drvarsha.com, or leave a comment, and be assured of a response soon.
References:

