Tubulointerstitial Nephritis
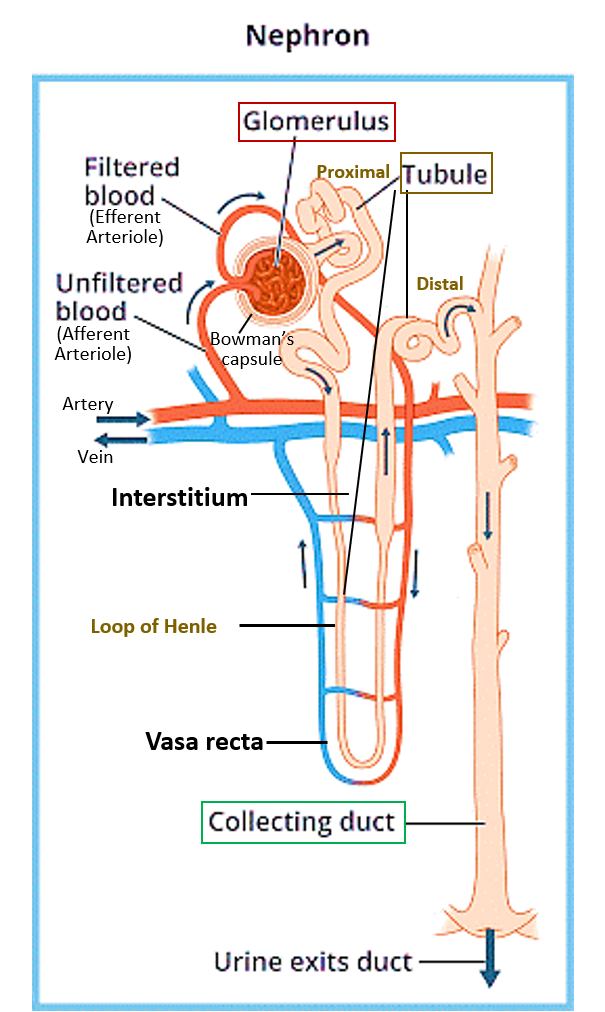
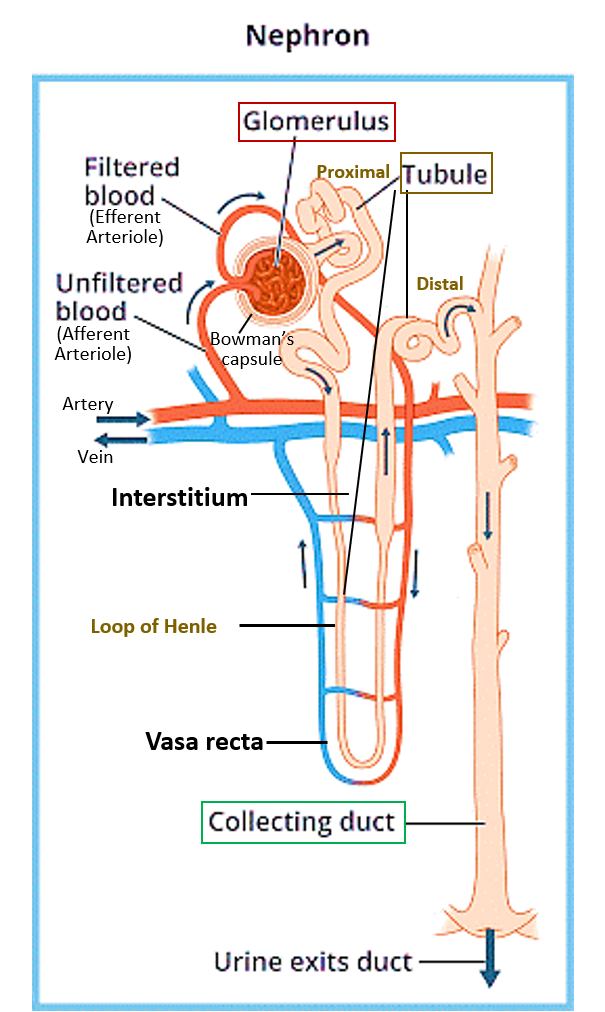
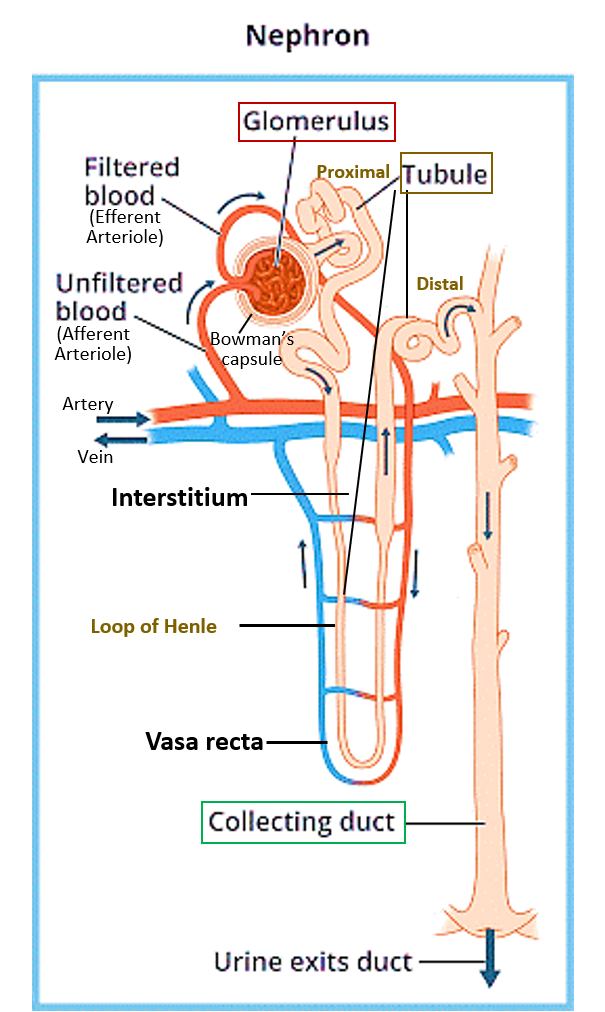
Tubulointerstitial nephritis (TIN) is the inflammation of the tubules of the nephrons (kidney cells) and the connective tissue (interstitium) in between them. This affects the functioning of the kidneys, as it is in the tubules that the urine is formed through the absorption and secretion of various substances and water.
Read: Kidney Structure and Function
SIGNS AND SYMPTOMS
Unfortunately, there are hardly any symptoms initially, and the condition comes to light only in the late stage when the kidney starts failing or its function reduces considerably. In acute cases due to a drug or allergic reaction, fever, itching, skin rashes, muscle/joint pain and abdominal discomfort may be present. Sometimes too much urination (polyuria) or increased frequency of night urination (nocturia) may be present. There may also be an unexplained rise in blood pressure or weight loss, fatigue, and anemia, in chronic cases.
CAUSES
Acute tubulointerstitial nephritis (ATIN) is usually caused by:
- Drug-induced or allergic reactions are the most common cause and can be due to antibiotics, TB drugs isoniazid and rifampicin, some antiepileptic and neuropsychiatric drugs, some diuretics, NSAIDs and many other drugs can be responsible, and it is hard to say which person will react to these drugs with TIN.
- Infections which may be bacterial, viral, parasitic, or fungal can spread to the kidney from other parts of the body to cause TIN.
- IgA nephropathy and other autoimmune diseases
- Poisoning substances
- Hyperoxaluria (too much oxalate in urine) due to genetic causes, intestine disease, or eating too many foods high in oxalate.
Acute tubulointerstitial nephritis can lead to acute kidney injury (AKI) and damage within days or months. It may take a few weeks in case of a first exposure to a drug, but the second exposure can cause damage within 3-5 days. If not treated promptly by stopping or removing the damaging substance chronic kidney damage can occur.
Chronic tubulointerstitial nephritis (CTIN) can occur due to
- Long-standing exposure to environmental or occupational toxins, or certain drugs – such as analgesics, lithium, heavy metals, unregulated herbal supplements, and radiation exposure.
- Obstruction or reflux of urine from the bladder into the ureters back into the kidney causing repeated infections.
- Increased uric acid (hyperuricemia), and other metabolic disturbances
- Cancers like multiple myeloma
- Tuberculosis
- Sarcoidosis
- Autoimmune diseases like IgA nephropathy
- Long-standing hypertension and formation of clots in blood vessels (thrombosis and emboli)
- Hereditary conditions like polycystic kidney disease are also a known association, in which clusters of cysts develop within the kidneys, causing kidneys to enlarge and lose function over time.
CTIN leads to gradual scarring (fibrosis) of the tubules and interstitial tissue and loss of renal function.
DIAGNOSIS
Clinical history and suspicion have to be very strong to pick up TIN. A careful drug and allergy history is imperative. One should also evaluate for any symptoms of infections anywhere in the body or autoimmune diseases like bowel symptoms (IBD) or eye symptoms (uveitis), along with family history. Blood pressure should be recorded.
A urine test may show blood (hematuria) and protein (proteinuria), along with increased white blood cells usually without evidence of infection (sterile pyuria). Sometimes there may be an increased presence of eosinophils. There may also be glucose and increased sodium in the urine. There have also been specific urinary markers developed and made available in some centers.
Blood tests may show raised blood urea nitrogen (BUN), creatinine, potassium and chloride (acidosis). There may also be evidence of anemia.
Imaging tests may show an enlarged kidney in ATIN and a shrunk scarred kidney in CTIN. The only specific test is a kidney biopsy.
TREATMENT
Treatment for ATIN is by removing exposure to the culprit drug/substance and treating any other underlying cause. Even after stopping exposure, some patients may continue to have damage for 6-8 weeks and eventually develop chronic scarring. Corticosteroids are the mainstay of treatment and work better if started within 2 weeks of exposure to the offending agent. Other immunosuppressant drugs may also be used to improve response.
CTIN is managed supportively by treating anemia and hypertension. In case of chronic kidney disease and failure, dialysis and kidney transplant will be required.
Also read:
Chronic Kidney Disease (CKD) – 5 Key Points of Understanding


