What is Fibromyalgia?
Fibromyalgia (FM) is a condition where the sensitivity to pain is increased in the body. This results in chronic pain in muscles and joints in various parts of the body. The exact cause is not yet known, but it points towards altered signaling in nerve pathways that transmit and receive pain. This could be due to an imbalance of chemicals in our nervous system (neurotransmitters) that regulate pain and mood possibly elevated levels of the excitatory neurotransmitters like glutamate and substance P, reduced levels of serotonin and norepinephrine, and alteration in levels of dopamine and endogenous opioids.
Anyone can get fibromyalgia, but it usually starts in middle age (40-50 years) and is more common in women, or those with a family history. Other risk associations include autoimmune diseases (SLE, rheumatoid arthritis, ankylosing spondylitis), osteoarthritis, back pain, IBS, and anxiety-depression.
What is the Type of Pain in Fibromyalgia?
The pain is described as a constant dull ache and should have been present for at least three months to consider fibromyalgia. The pain is often widespread (on both sides of the body and above and below the waist) like muscle ache in the neck, back, arms, and legs, or joint pain in knees, hips, and hands/feet.
The pain can present in a variable manner in different people and can be severe and unbearable lasting from a day to even a few weeks. There may also be tenderness in various areas (increased pain on touching). The pain and stiffness may be present on waking up, and for some people, pain improves during the day and gets worse at night, while others may have pain all day long.
What are the Other Symptoms of Fibromyalgia?
There can be accompanying symptoms like:
- severe chronic fatigue and compromised day-to-day functioning
- inability to concentrate and effects on memory (feeling of brain fog)
- chronic sleep disturbances
- mood instability, and anxiety-depression
- muscle and joint stiffness
- numbness or tingling in the arms and legs
- increased sensitivity to light, sound, smell, and temperature
- indigestion, bloating or constipation
Fibromyalgia can cause similar symptoms as Chronic Fatigue Syndrome (CFS), but heightened sensitivity to pain and widespread musculoskeletal pain lasting 3 months or more, is the primary symptom of fibromyalgia. Fatigue, sleep, and cognitive problems are common symptoms in FM, but pain all over the body is its main characteristic, while pain though common in CFS, is not its defining characteristic.,
How is Fibromyalgia Diagnosed?
Fibromyalgia is a diagnosis of exclusion, based on the symptoms mentioned above, and when other causes of pain have been evaluated and examined for. Some clinicians require specific criteria for diagnosis to be fulfilled over a 3-month-period for establishing fibromyalgia.
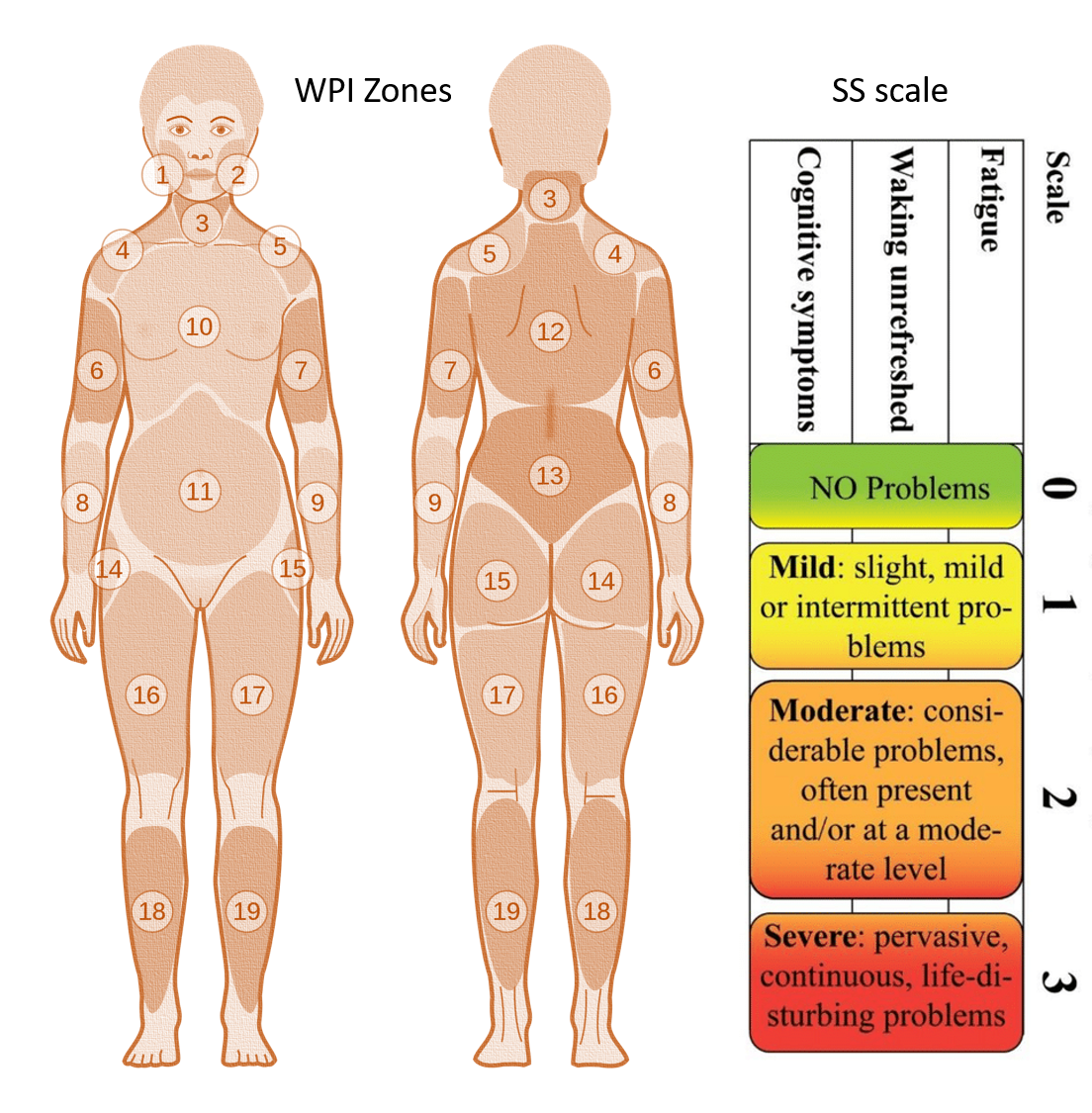
Widespread Pain Index (WPI): The index scores between 0 and 19 based on the number of regions with pain in the past week
SS scale score: It evaluated fatigue, waking unrefreshed, and cognitive symptoms, each on a 0-3 severity level making a score range of 0-12.
To diagnose fibromyalgia, the following 3 points should be present:
- The widespread pain index (WPI) is at least 7 and the symptom severity (SS) scale score is at least 5, or WPI equals 3 to 6, and the SS scale score is at least 9.
- Symptomatology has been present at a similar level for at least 3 months.
- The patient does not have any other condition that would otherwise explain the pain.
How does one Manage Fibromyalgia?
The management of Fibromyalgia is centered around the management of Pain. This includes medicines, as well as various other therapies.
- Physical therapy and Exercise should be gradually graded up and balanced. A physical therapist should be consulted to design and monitor a plan of aerobic exercises. Physical Therapy includes gentle manual therapy techniques that improve tightness in limbs and spine, making movement easier. Stretching, movement therapies, gentle massage, and water therapy can also be helpful for pain management. Yoga should focus more on stretching, de-stressing, and breathing and then graded up to more complex postures. Acupuncture, massage therapy, and chiropractic care may provide additional pain relief in FM, along with stress management.
- Diet followed should be well-structured. A healthy diet not only helps improve energy levels but also decreases BMI and cuts the risk of other chronic diseases. Obesity or being overweight has been linked to a greater risk of developing fibromyalgia.
- Sleep should be adequate in both duration and quality. Improving sleep should be a central part of managing fibromyalgia.
- Psychological counseling can help in managing stress as well as the impact on mental health or the presence of depression. Counseling can also help in cognitive training and improvement.
- Medicines: Pain-relieving medicines (over-the-counter ones like paracetamol, ibuprofen, etc.) or prescription medications (pregabalin, gabapentin) are central to managing FM. Other medicines include antidepressants that are often prescribed to improve low moods, body pains, and lack of sleep and mainly have a supportive role. Sometimes immunomodulator medicines are tried, but their efficacy varies. Medications to regulate blood pressure or heart rhythms may be helpful for symptoms of palpitations and dizziness worsening on standing (orthostatic intolerance).
- Supplements: These may include vitamin B (B12, B3, B6, folic acid), C, and D, minerals like magnesium, and other supplements like melatonin, CoQ10, and L-carnitine.
There is still a need for more robust clinical evidence on these treatments for FM, and there is a likelihood of variation in the benefit and response not only in different patients but also in the same patient over the years.
Read in detail below:
Reference: Fibromyalgia clinical understanding
Also read:

