WHAT IS Chronic Kidney Disaese (CKD)
Chronic Kidney Disease (CKD) or kidney failure is caused due to damage and loss of function of the kidney over a period of time.
The filtering, absorbing and secreting capacity of the kidney to excrete wastes and form urine gradually becomes less efficient. This can happen due to chronic diseases of the kidney itself or diseases of other organs.
CAUSES
DISEASES OF KIDNEY
- Glomerulonephritis: Inflammation of the filtering units (glomeruli – network of blood capillaries) of the kidney cells (nephrons)
- Tubulointerstitial nephritis: Inflammation of the tubules and surrounding structures of the nephrons (kidney cells)
- Inherited kidney diseases like polycystic kidney disease
- Prolonged obstruction of the urinary tract, from conditions such as enlarged prostate, urinary stones, strictures and other causes of LUTS.
- Urinary tract infections especially when recurrent and spreading to the kidney (pyelonephritis) due to abnormal vesicoureteral reflux, a condition that causes urine to backflow up the ureters into your kidneys.
- Kidney cancers
OTHER DISORDERS AFFECTING KIDNEY
Diabetes is the leading cause of chronic kidney disease. Blood sugar when high complexes with other substances like proteins and lipids to form advanced glycation end products (AGEs) that can deposit and damage blood vessel walls, and the kidney. Kidney damage due to diabetes is called diabetic nephropathy and progressively leads to Chronic Kidney Disease (CKD).
Hypertension – High blood pressure not properly controlled over time can cause the arteries to the kidneys to constrict (narrow) and its walls to weaken or harden. This reduces blood flow to the kidneys and the filtering capacity of the nephrons.
Cardiovascular disease (CVD) is the formation of plaques (atherosclerosis) that damage blood vessel walls and increase risk of clots and blockages of vessels. This can impact multiple arteries in the body including those of the kidneys thereby compromising renal blood flow and function over time. CVD risk factors include hypertension, diabetes, increased cholesterol-triglycerides, ageing, heart disease, obesity, smoking, etc.)
Renal artery stenosis is the narrowing of one or more arteries that carry blood to the kidneys (renal arteries). It can occur due to cardiovascular disease and atherosclerosis (build-up of plaques) in the renal arteries. However, renal artery stenosis can rarely be seen in childhood due to a condition called fibromuscular dysplasia, where the muscles in the artery wall do not develop properly. Renal artery stenosis can lead to high blood pressure that begins suddenly or worsens without explanation and may begin early in life. The BP is usually difficult to control, and progressively renal artery stenosis leads to CKD.
Heart Failure often leads to Chronic Kidney Disease and vice versa setting up a vicious cycle. When the heart is not pumping effectively, backflow can cause congestion in renal veins, and blood flow of oxygenated blood via renal artery is reduced. This leads to reduced filtration and urine production, electrolyte disturbance and fluid retention that further increases the congestion and resistance against which the heart has to pump. Therefore heart failure and kidney failure often progress together.
Liver Cirrhosis can cause what is called hepatorenal syndrome (HRS) which is a serious complication occurring due to severe constriction of the renal arteries, resulting from complex compensatory changes in splanchnic (blood circulation consists of the blood supply to the gastrointestinal tract, liver, spleen, and pancreas) and general circulations and disturbed balance and release of vasoconstrictor and vasodilator substances by the body. It leads to rapid and progressive renal failure.
Autoimmune diseases like Lupus, IgA nephropathy and many others can affect multiple organs including the glomerulus and tubules of the kidney. Chronic damage of the kidneys can lead to kidney failure.
Sepsis is a serious and severe blood infection that affects multiple organs and can cause an already compromised kidney to fail, as blood pressure and blood flow to the kidney can be reduced. Sepsis also increases formation of blood clots and obstruction of small vessels like capillaries that are crucial to the filtration process. Toxic wastes build-up due to the absence of proper filtration, worsening the sepsis and setting a vicious cycle. This is generally seen in hospitalized chronically ill patients who are already suffering from heart-lung problems.
SIGNS AND SYMPTOMS
In the initial stages, there may be no symptoms except the co-morbid conditions like high BP, or a routine urine test showing abnormalities in creatinine excretion, urinary volume, and the presence of other substances like blood, proteins, sugar, pus cells, casts, etc.
Gradually there is fluid and salt retention with swelling of the feet and ankles, and then the whole body, including a pot belly or puffed face appearance. There may be shortness of breath, weakness, and fatigue due to anemia, muscle cramps, loss of appetite, nausea, and vomiting as toxic wastes build up and there is electrolyte imbalance, and dry itchy skin.
Initially urine production may be increased and one may want to urinate often, which may even disturb sleep. This happens due to leaky inflamed nephrons and the urine may appear foamy due to proteins leaking out. However, this is usually followed by reduced urine production as the kidney damage and functional loss progress.
Renal osteodystrophy, seen in those with chronic kidney disease (CKD), is a group of bone abnormalities that can cause bone thinning, weakness, pain, and fractures. Compromised kidney function reduces the conversion of vitamin D to its active form, and leads to a lack of calcium and phosphorus in the bones.
DIAGNOSIS AND STAGING
Blood and urine tests (Kidney Function Tests) are conducted for levels of creatinine, blood urea nitrogen (BUN), electrolytes, proteins and other abnormalities suggesting compromised urine function.
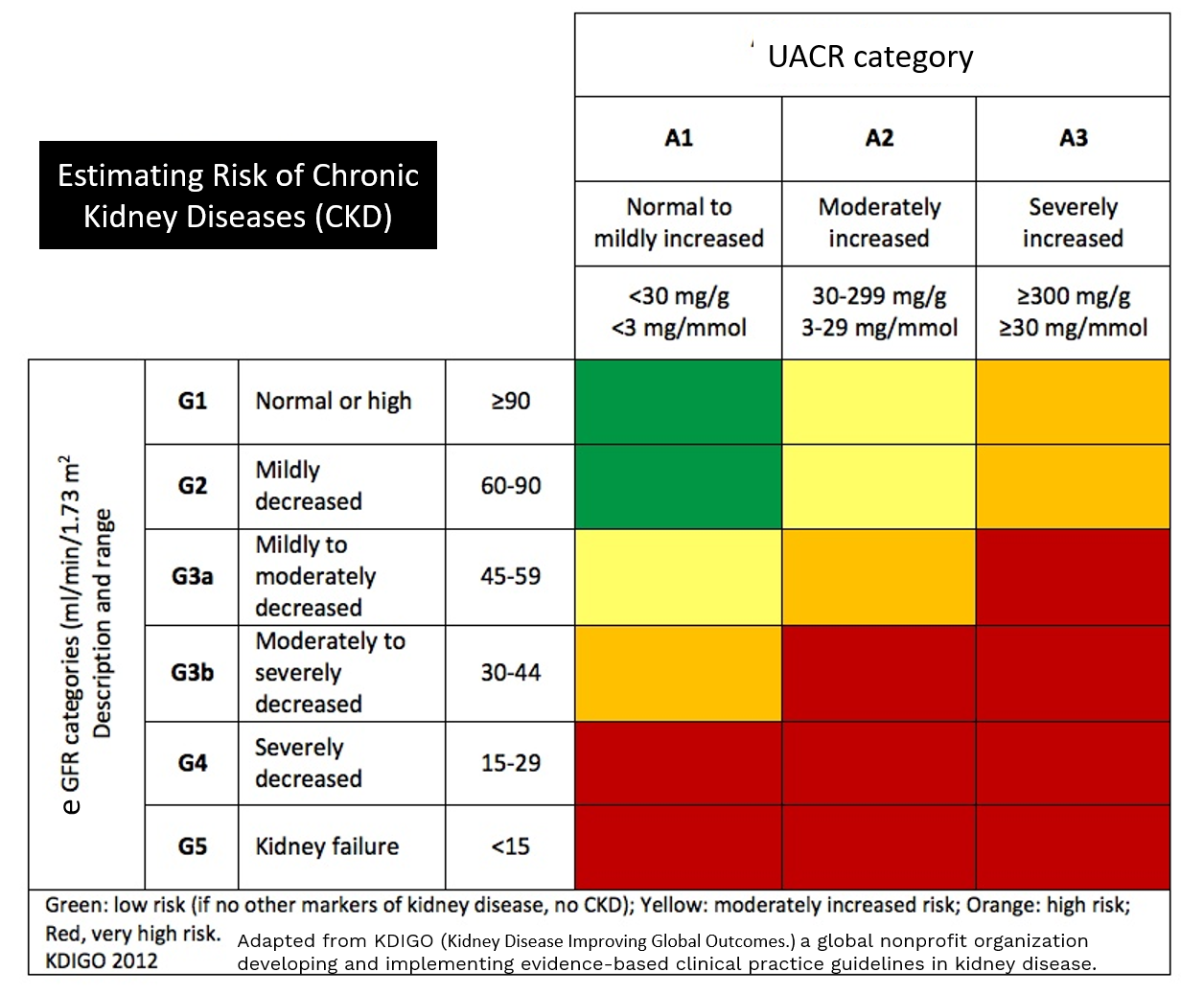
From the creatinine values based on age, gender, weight and race, an estimated glomerular filtration rate (eGFR) can be calculated, which gives an idea of the filtering function of the glomerulus. The values are given as % of what is normal for that age, gender, weight and race. Sometimes UACR ((Urinary albumin to creatinine ratio) and eGFR are used to grade level of kidney dysfunction and risk of chronic kidney disease (CKD).
TREATMENT
Diet should be nutritious with vegetables and whole wheat/rice and low in proteins, salt, and fat. Supplements like Calcitriol (active form of vitamin D) should be supplemented to maintain bone health. Erythropoietin (kidney hormone that stimulates hemoglobin production) injections may be needed to manage anemia.
Treating underlying conditions
Treating comorbidities like blood pressure, diabetes, CVD, high cholesterol/triglycerides, heart failure, or liver cirrhosis is most important.
Diuretic drugs help to decrease swelling and eliminate fluid and salts.
Antihypertensive drugs usually include angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) as the first-line choice while MRAs (mineralocorticoid receptor antagonists) like spironolactone and the new drug finerenone are used in treatment of resistant hypertension.
The SGLT-2 inhibitors (flozins) reduce the risk of heart failure hospitalization and death, and kidney failure especially in people with diabetes, living with kidney disease.
Smoking and use of painkiller drugs like NSAIDs etc, should also be stopped.
One may have to use immunosuppressants like corticosteroids in autoimmune conditions and nephritis.
Infections if present, should be treated with appropriate antibiotics.
Regular monitoring of blood pressure, as well as blood and urine kidney function tests including eGFR is important.
However, the only definitive solution for chronic kidney disease is dialysis and kidney transplant.
DIALYSIS
It is a procedure that uses machines instead of kidneys to remove waste products from the body. There are two major types –
Hemodialysis: The blood is circulated and passed through the dialysis machine, wastes removed like excess salt/water, and then returned into the body. It usually takes a 4-hour sitting thrice a week.
Peritoneal dialysis: A dialysis solution is inserted through a catheter into the abdomen that absorbs excess salt and fluid and then is removed through the same catheter. Fresh solution is then re-introduced. There are two types of peritoneal dialysis: continuous ambulatory peritoneal dialysis (CAPD), which involves a change in dialysis solution four times a day; and continuous cycling peritoneal dialysis (CCPD) that uses a machine to automatically fill, remove and refill the fluid during the night time.
KIDNEY TRANSPLANT
Kidney transplant involves replacing an unhealthy kidney with a healthy kidney from a donor that can be living (family members – who have both healthy kidneys) or recently deceased. Deceased donor kidneys usually come from people who are organ donors, after screening for suitable matching and absence of any diseases. One has to usually be put on a transplant list and then is continued on dialysis and supportive treatment till a suitable match and their turn come up for transplant. This can take anywhere between 1-5 years if waiting for an organ donor, however much quicker if a family member donates a kidney.
Also read:
Tubulointerstitial nephritis – Causes, Diagnosis and Treatment
Urinary Tract Infection (UTI) – urethritis, cystitis, ureteritis, pyelonephritis

