Back pain is one of the most common health problems encountered which can reduce work capacity, productivity and quality of life.
THE BACKBONE
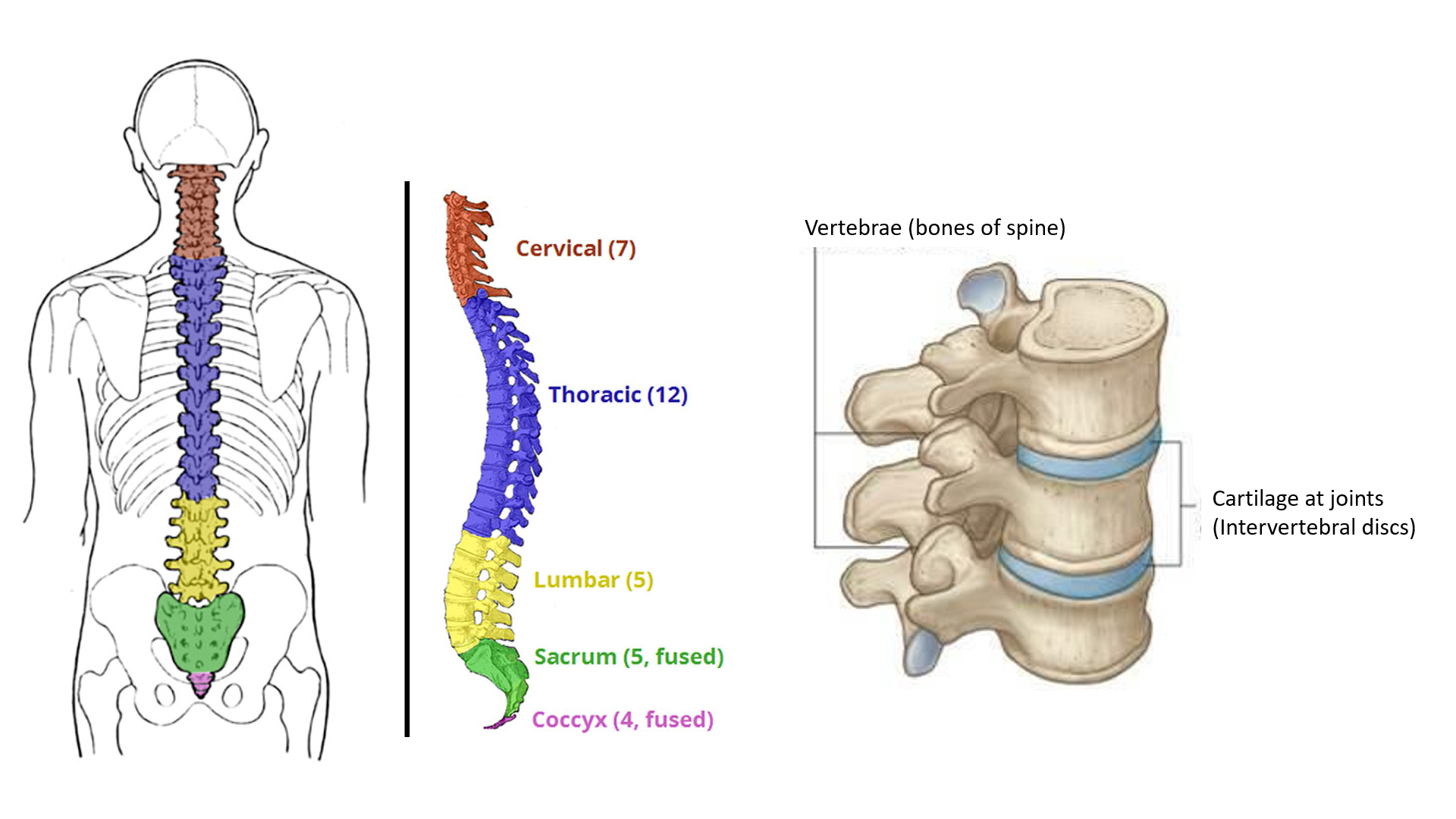
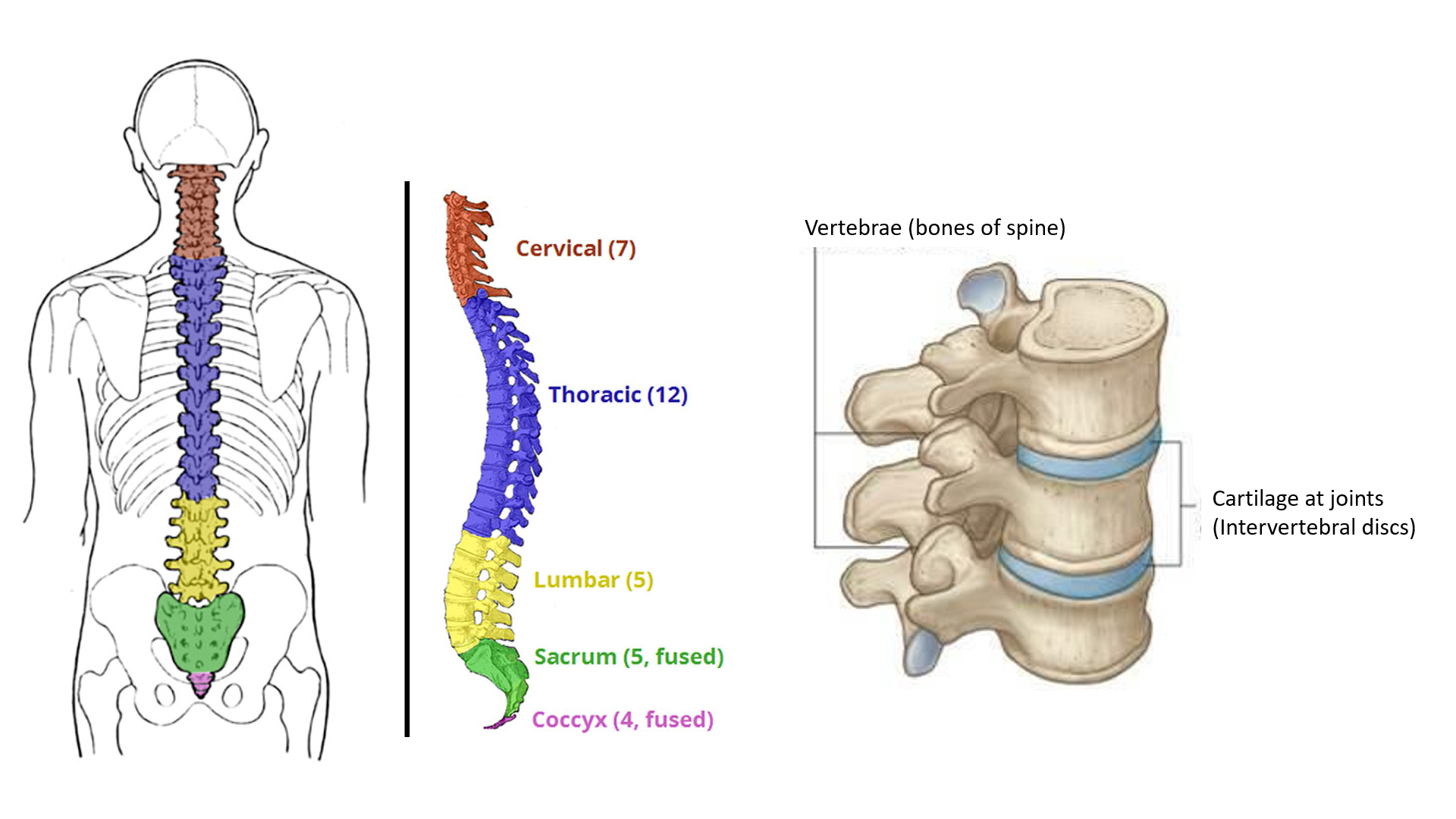
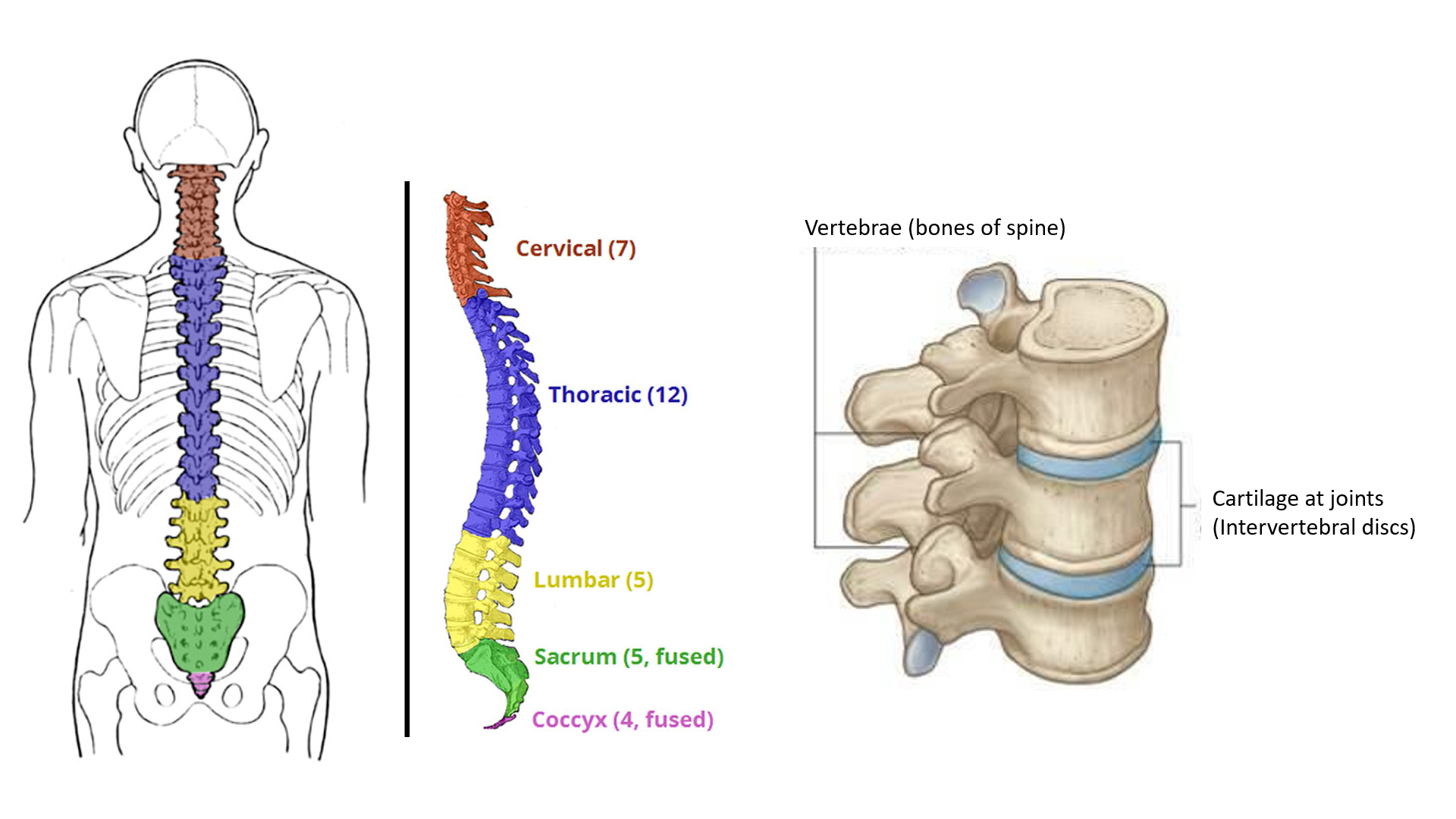
Our back is made up of the vertebral column (backbone or spine) along with muscles and nerves. The vertebral column is made up of several individual ‘vertebrae’, joint by cushion-like cartilage pads called ‘intervertebral discs’ between them. Enclosed within the backbone is the spinal cord (connected to the brain) from which spinal nerves come out through openings in the vertebrae on either side. These nerves supply the back, limbs, and abdomen.
The region of the back is divided into cervical (neck region – 7 vertebrae: C1-C7), thoracic (chest region – 12 vertebrae joining the 12 ribs: T1-T12), lumbar (lower back region – 5 vertebrae: L1-L5), sacrum (base of the spine – 5 fused vertebrae: S1-S5) and Coccyx (tail bone – 4 fused vertebrae).
Back pain may be due to problems of the vertebrae, intervertebral discs, muscles, nerves, or organs in the vicinity.
CAUSES OF BACK PAIN
Strain of the back can be due to short-term and long-term causes.
Short-term strain is commonly caused by:
- working/sitting in faulty postures for prolonged periods
- sudden twisting, bending, overstretching
- heavy exercise
- lifting weights
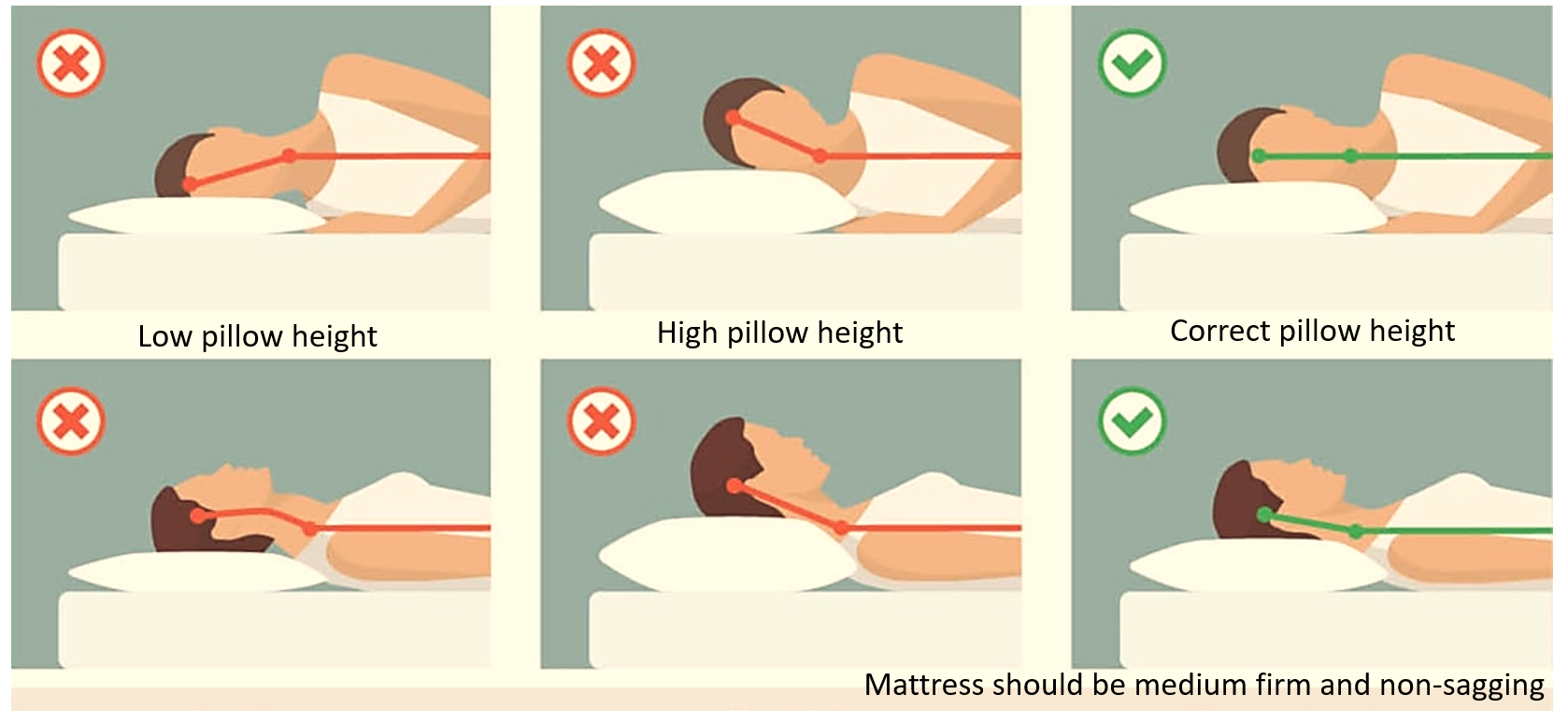
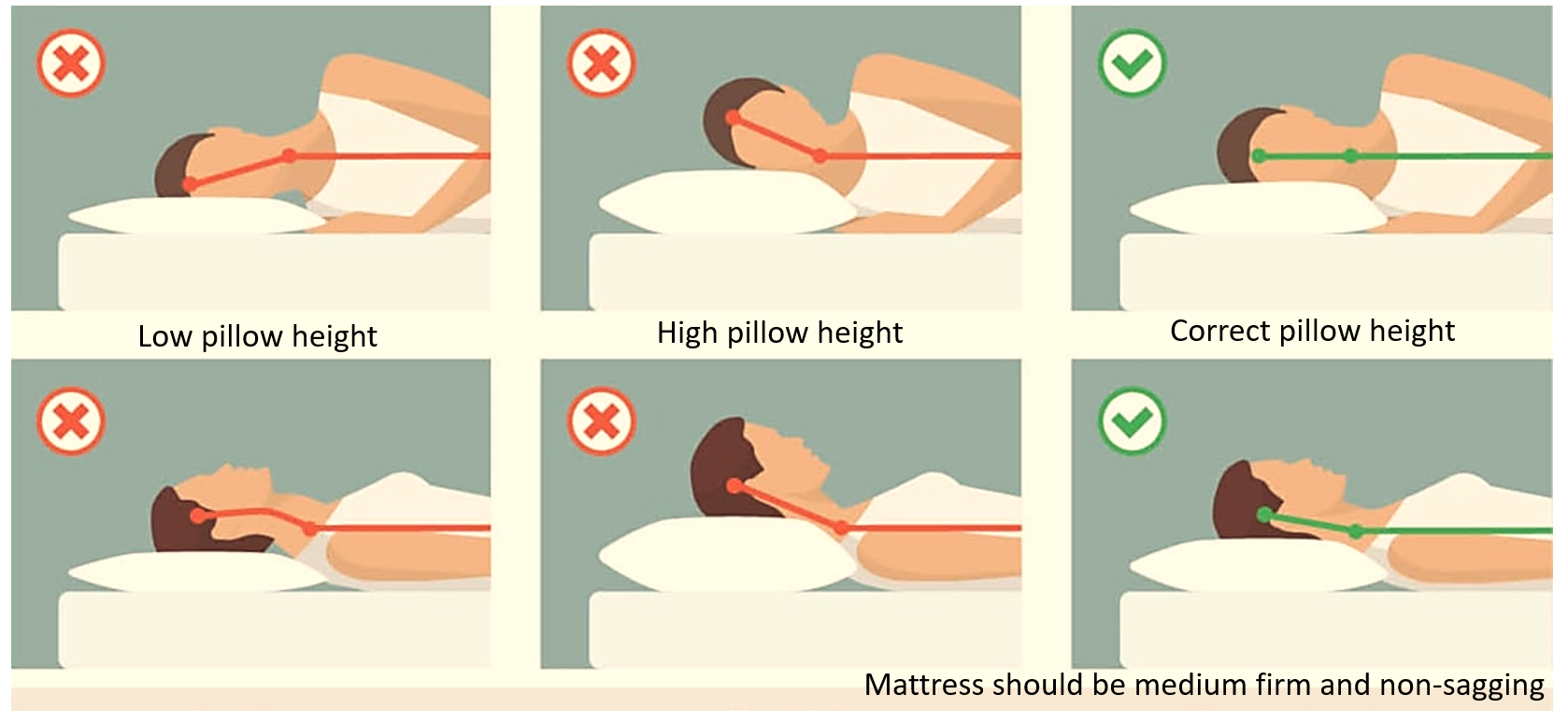
- sleeping in an abnormal posture
- fall/injury on the back
Short-term strain is usually due to muscle tension, spasm or injury.
Long-term strain is seen due to faulty lifestyle-
- prolonged working hours
- improper posture
- occupational strain
- extensive use of gadgets like mobile phones and laptops.
- aging (accentuates strain)
Long-term strain increases wear and tear of muscles, vertebrae, and the discs, while aging reduces the body’s capacity to repair and regenerate effectively.
Arthritis of the Backbone (Spondylitis)
Increased wear and tear lead to degenerative changes in the bones and joints of the cervical or lumbar backbone causing spondylosis (spondylo-arthrosis). When this progresses to inflammation, it manifests as constant/frequent back pain and reduced flexibility and mobility. The condition is then said to be spondylitis (spondylo-arthritis).
Arthritis is the inflammation of the joints, while arthrosis is a preceding condition of increased wear and tear with degeneration of joints. Therefore spondylosis and spondylitis refer to the arthrosis and arthritis of the backbone. Cervical spondylitis causes neck and shoulder pain, while lumbar spondylitis causes lower back pain. Ankylosing spondylitis is an autoimmune condition causing inflammatory arthritis affecting the spine and large joints.
Disc prolapse
The Intervertebral disc can degenerate, or bulge out (called a slipped disc, herniated disc or disc prolapse). Disc prolapse can exert pressure on the adjoining nerves leaving the spinal cord, causing a shooting pain along the line of the nerve supply. Sciatica is such a sharp, shooting pain going from the lower back through the buttock and down the back of the leg, due to a disc prolapse between L4-L5 or L5-S1.
Other Spine related causes
Apart from the above common causes of back pain, there may be less common and rare causes that may need to be explored in certain cases. Fracture of the vertebra should be ruled out especially if a history of injury is present, or in aging people with osteoporosis.
Sometimes spinal curvature abnormalities like scoliosis (side curve) and lordosis (inward curve) can cause chronic back pain. Back pain may also be due to spinal infections (usually accompanied by fever), herpes (shingles) of the spinal nerves, or spinal tumors.
Autoimmune arthritis has been seen in the backbone which leads to damage and inflammation (caused by the body’s own immune system) of the intervertebral discs and adjoining vertebra. This makes the spine appear fused like a ‘bamboo’ on X-ray, a condition called ankylosing spondylitis which causes a stiff and painful back. Sometimes this may be associated with similar arthritis of other peripheral joints, as well as inflammation inside the eye (uveitis).
Non-Spinal causes
Diseases of organs in the vicinity also sometimes manifest as back pain. This is seen in certain abdominal conditions (like pancreatitis, kidney stones, pelvic inflammatory disease, etc.) causing lower back pain, and chest conditions (like some diseases or tumors of lung and aorta) causing upper back pain.
Obesity, lack of physical exercise, dietary deficiencies (decreased vitamin D and calcium), and smoking increase the overall risk of back pain. Pregnancy is also a common cause of back pain due to the pressure of the growing uterus. Stress, lack of sleep, and anxiety also aggravate back pain.
MANAGEMENT OF BACK PAIN
Short-term back strain and pain are managed by:
- adequate rest
- relaxing exercises or stretches to relieve muscle tension
- using warm compress/pads
- taking analgesic and muscle relaxant medicines when required.
Strenuous exercises like weights and push-ups should be started or undertaken only under the guidance of a qualified trainer.
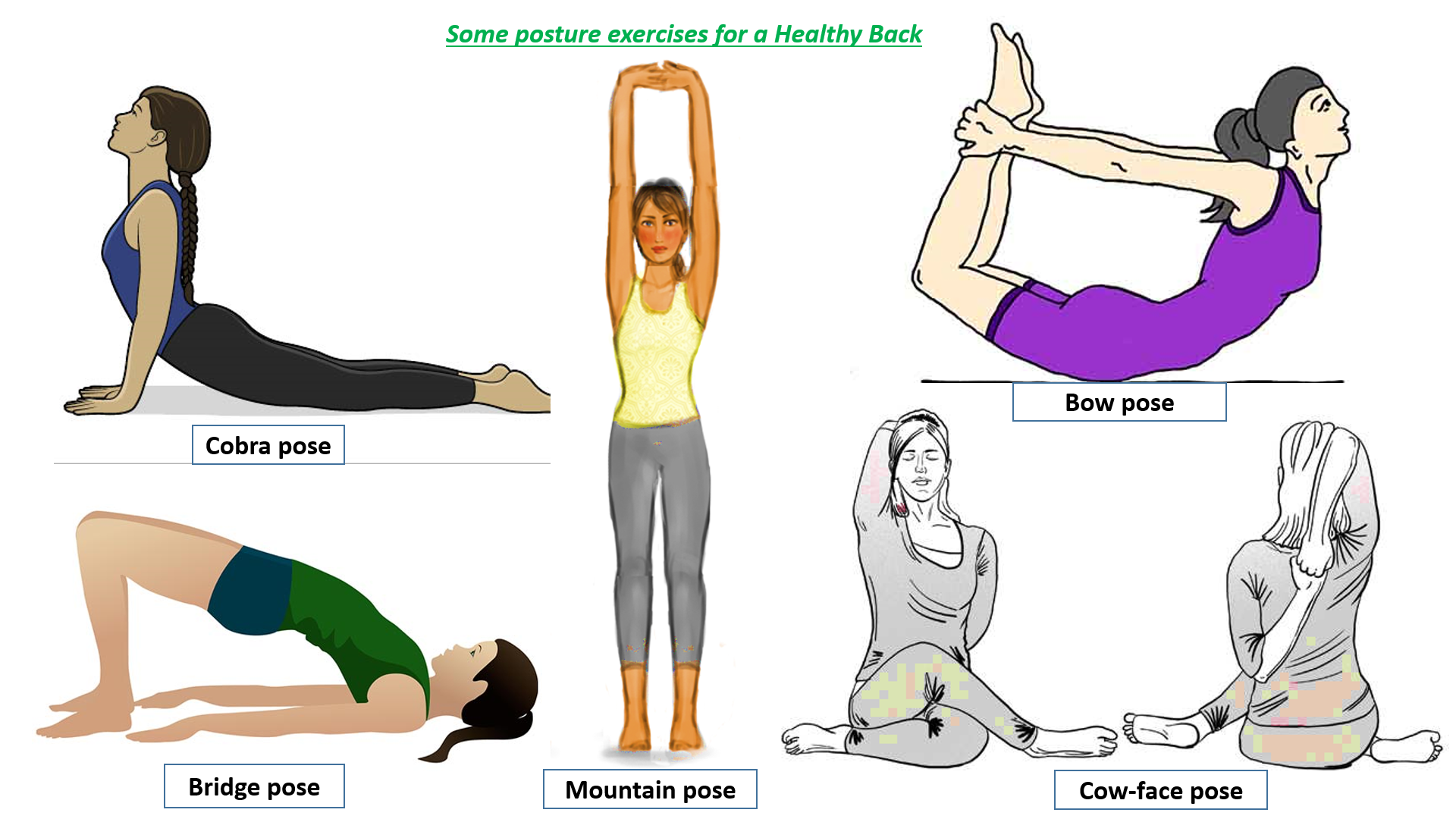
To avoid and manage long-term back strain, the following lifestyle modifications are helpful –
- maintaining a nutritious diet and appropriate weight
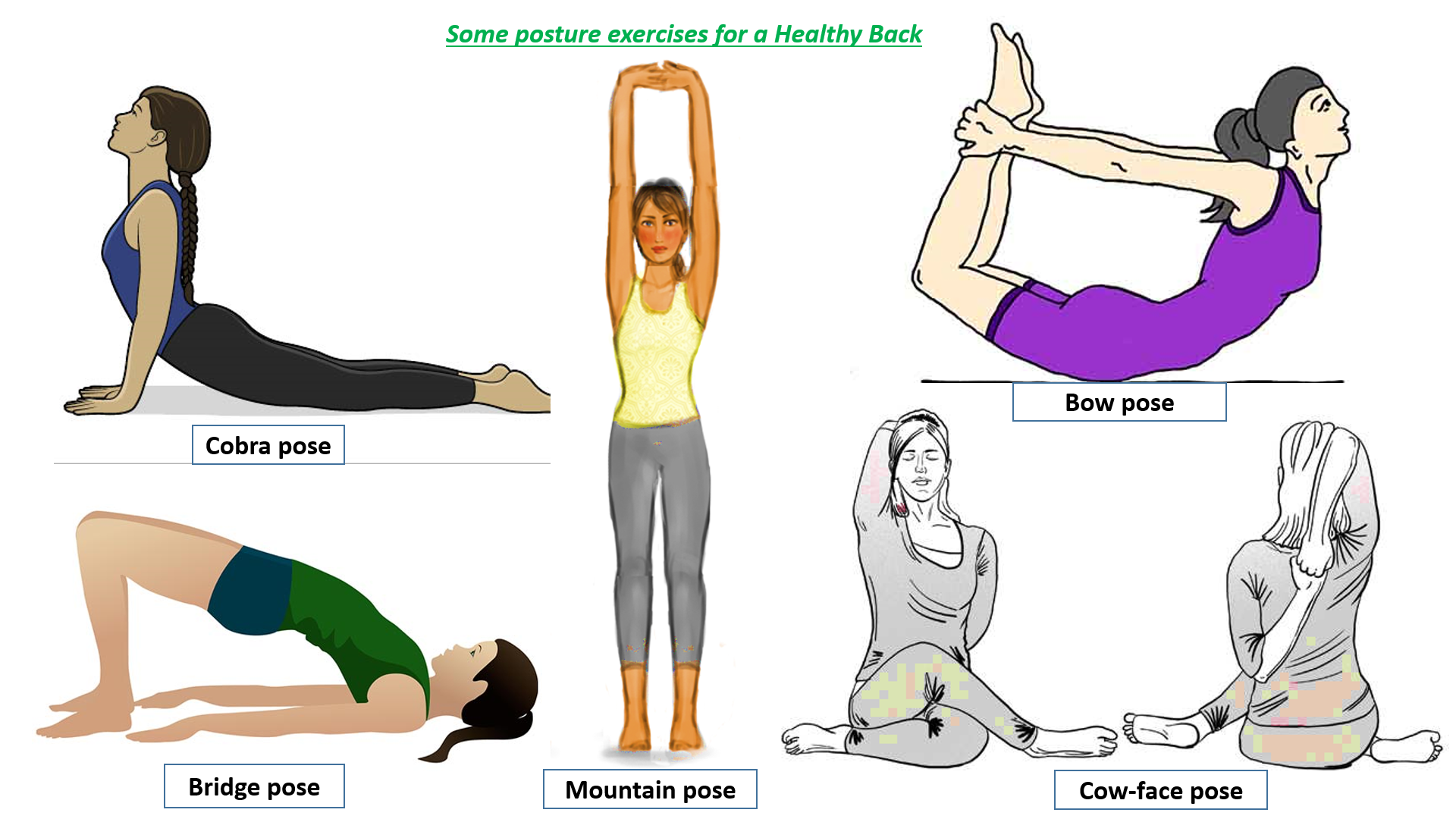
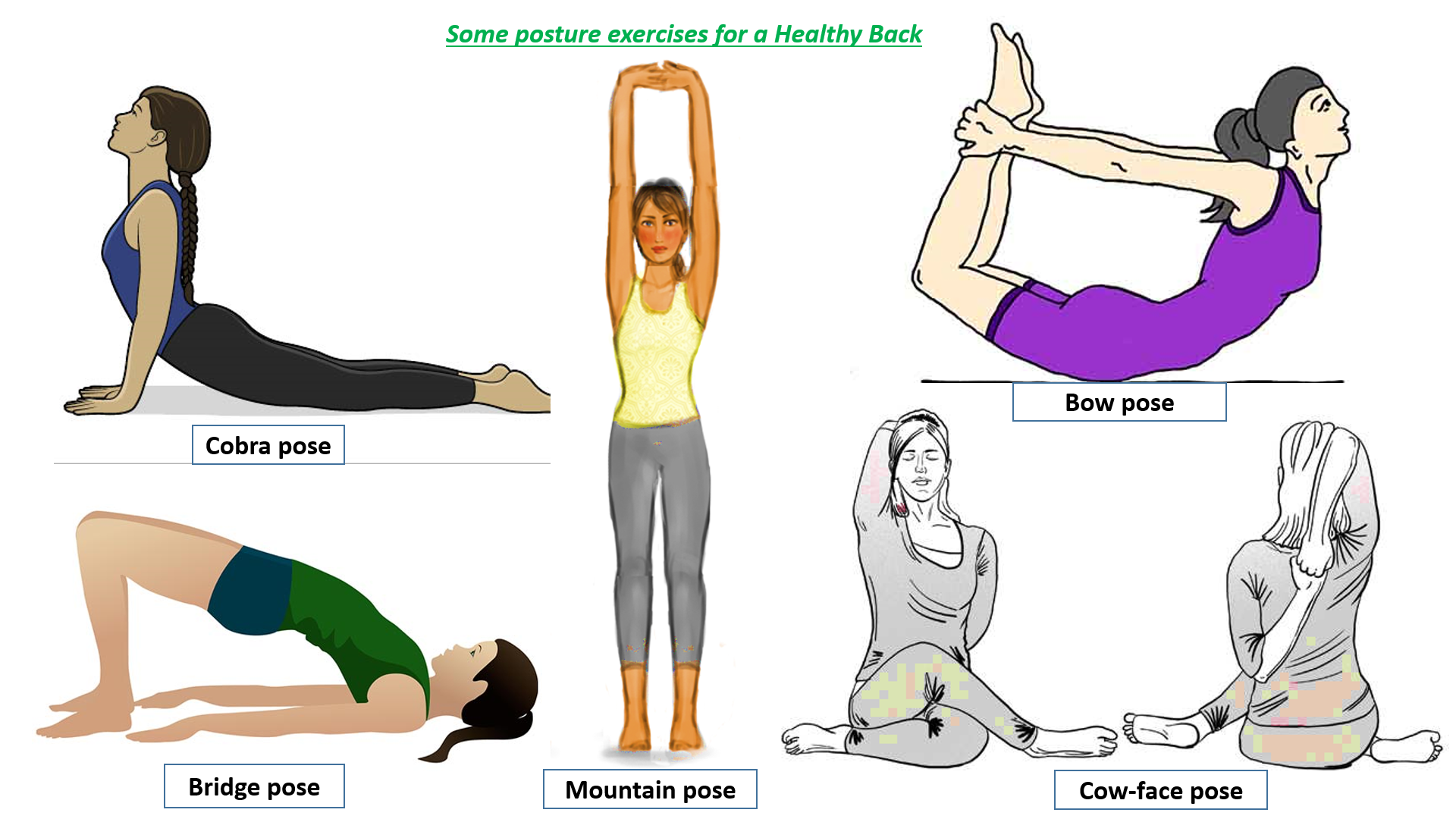
- regular physical exercise, with specific back stretches
- correcting posture, taking precautions during gadget use and ensuring workplace ergonomics
- testing for vitamin D and calcium deficiency
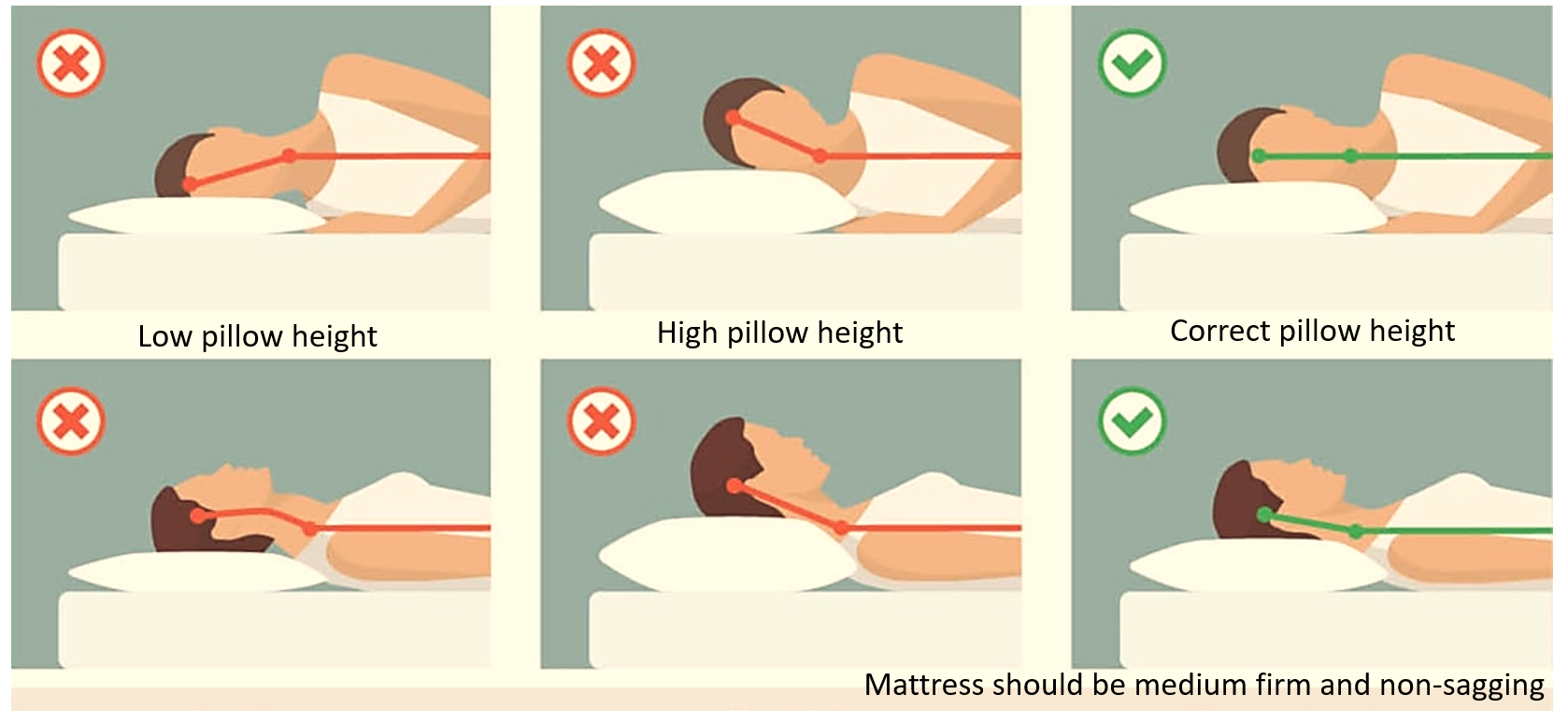
- ensuring adequate rest and sleep, with appropriate pillow and mattress
Read – Precautions while using Computer/Laptop at work and Points of care for mobile phone usage.
Investigating long-term Backache
In the case of long-term back pain, it is prudent to meet a doctor who would examine and advise required investigations according to history and examination. Disc prolapse is indicated by the slow straight leg raising test on medical examination. While lying flat, one leg is raised without bending the knee, and a pain radiating from the back down the back of the leg is indicative of sciatica.
Investigations required include blood tests, X-rays, CT, MRI or Ultrasound to establish the diagnosis. Special tests may also be recommended like nerve conduction tests, muscle function test (EMG- Electromyography) and myelogram (X-ray after dye injection into the spinal fluid to show nerve pressure due to prolapsed disc).
Treatment modalities
These include-
- pain-relieving and anti-inflammatory medicines
- healthy diet and nutritional supplements (like vitamin D, calcium and sometimes collagen supplements)
- appropriate guided exercises
- physiotherapy sessions
- traction therapy (in disc prolapse)
- wearing of collar/brace/belts when required
Read – Arthritis Health Solutions – Diet, Lifestyle, Medicines and Supplements
Spinal surgery may be needed if conservative treatment is ineffective, especially for releasing pressure on nerves, removing bone overgrowths and tumors, stabilizing fractures, or for correcting the spinal curvature. Commonly performed back surgeries include discectomy (removing the prolapsed portion of the disc), laminectomy (removing a portion of the vertebrae), fusion (fusing two vertebrae for stability), and putting in an implant (like artificial discs).
Further reading-
Arthritis – Awareness of the Causes, Types and Health Impact
Weak, Thinning Bones: Osteoporosis Risks and How to get Screened
For any query, additional information, or to discuss any case, write to info@drvarsha.com and be assured of a response soon.
REFERENCES


