WHAT IS MUCORMYCOSIS AND WHY DOES IT OCCUR
Mucor is a fungus found usually in damp and hot environments, in the soil, contaminated water, plants, decaying vegetables-fruits and wood. The fungal disease (mycosis) it causes is called Mucormycosis. The term ‘black fungus’ is due to the blackish discoloration of the affected parts damaged by the fungus.
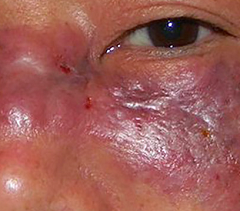
It is a very rare fungal infection impacting those with significantly weakened immunity. The fungus usually invades on inhalation of the spores and entry through a breach or damage in the lining of the nose (nasal mucosa). Once inside, it can rapidly spread causing clots and blockages in blood vessels leading to the destruction of the affected body tissues (dead tissue appears blackish). From the nose, it can move upwards into the sinuses, eye, and then the brain (rhino-orbital Mucormycosis, rhino-cerebral Mucormycosis) or it can move downwards into the lungs (pulmonary Mucormycosis).
WHO IS AT RISK?
Mucor affects people who have any condition which reduces their immunity and ability to suppress/fight infections significantly. This includes
- COVID
- Diabetes (especially if uncontrolled)
- Use of corticosteroids in high dose or prolonged duration
- Use of other immunosuppressive medicines
- Prolonged hospital/ICU stay and oxygen therapy
- Cancers
- HIV and immunodeficiency diseases
- Organ transplants
- Post burns, trauma, or surgery
- Antifungals used for other fungal infections (like voriconazole for Aspergillus)
COVID and Mucormycosis
A rise in Mucormycosis cases post-COVID was worryingly seen during the 2nd wave in 2021 in some countries like India. COVID increases the risk of Mucormycosis in multiple ways, and this can occur anywhere between 10 days to 3 months after COVID onset, most commonly in the 2-3 weeks post-recovery period. The multiple factors at play are:
- Coronavirus itself has a suppressive effect on immunity. Variant strains like Delta can particularly show more immunosuppression, immune escape, and low lymphocyte counts.
- Rise in blood sugar in COVID infection occurs sometimes even in patients who have not been diagnosed with diabetes before. COVID can impact sugar control in patients with diabetes and cause sugar levels to go up or fluctuate.
- Steroid medicines (oral/injectable corticosteroids) have a suppressive effect on immunity, and also increase blood sugar therefore act as a double whammy in increasing Mucormycosis risk in COVID patients.
- Hospital admission especially prolonged ICU stay, due to severe COVID along with strong antivirals, antibiotics, injectable corticosteroids and other immunosuppressant medicines like tocilizumab lead to a highly weakened immune system.
- Oxygen therapy can add to the risk of mucor exposure and infection. The oxygen is humidified to prevent drying of nasal passages and airway, therefore the water used predisposes to harboring and growth of Mucor. Prolonged use of nasal prongs for high flow oxygen can cause micro-damage and compromised local immunity of the nasal mucosa.
WHAT ARE THE SYMPTOMS
- Blocked or stuffy nose (nasal congestion)
- Crusting in the nose or discharge from the nose which is thick/bloodstained/discolored
- Pain, swelling, numbness, or any discoloration on the face, especially of or around the nose or eyes
- Headache and pain in sinus area on the cheeks
- Vision changes (double vision, blurring or loss)
- Eye protrusion or inability to move eyes in a particular direction
- Pain in teeth/gums, loosening of teeth
- Fever
- Cough, shortness of breath or chest pain
- Blood in cough or vomit
- Altered or decreased consciousness/alertness, or seizures
HOW IS IT DIAGNOSED AND TREATED
Diagnosis involves the collection of mucus/phlegm or tissue (biopsy) from the affected parts and evaluating it by KOH staining-microscopy, culture, RT-PCR and mass spectroscopy techniques to confirm the presence of the Mucor fungus. Others include CBC, sugar, and routine blood tests. Imaging is important to see extent of spread and include nasal endoscopy, CT scan and preferably MRI with contrast (when planning surgery) in accordance with involved areas and symptoms.
Treatment should be done in the hospital. Blood sugar control and discontinuation of steroids and other immunosuppressant drugs is urgently needed. Removal of dead and damaged tissue (surgical debridement) should be performed. The patient is hydrated with intravenous normal saline.
Amphotericin B (AmB) is the first-line antifungal of choice and is given intravenously. It can have toxic side effects like nausea, vomiting, chills-rigors, fever, BP fluctuations, breathlessness and decrease in kidney function. Liposomal preparations of amphotericin B are available which are far less toxic to the kidney. A nanofibre-based, controlled-release oral tablet of amphotericin B has recently been developed and is awaiting approval. The treatment duration is 4-6 weeks. Alternate drugs like isavuconazole and posaconazole are sometimes used if amphotericin B is causing too much toxicity and intolerance. However other antifungals like voriconazole, fluconazole, etc should not be used and these can worsen the disease.
Extensive surgery involving removal of eye, parts of the face and sinus with extension into the base of the skull may be required for saving life. Draining fluid from around the lungs (pleura) may also be needed. Treatment is performed by a multispecialty medical team consisting of ENT, eye and general surgeons, radiologist, pulmonologist, intensivist, neurologist, microbiologist, pathologist and dentist.
If diagnosed and treated in time, there is a good chance of recovery. The mortality rate is high at almost 50%.
WHAT PRECAUTIONS SHOULD BE TAKEN
- Blood sugar monitoring should be regular in diabetes patients and sugar should be well controlled with medicines. Blood sugar should be monitored in COVID patients during treatment, hospitalization and up to 3 months post-discharge/recovery.
- Steroids should be used appropriately in COVID patients and in the minimum dose and duration required. Oral steroids are not to be routinely prescribed in mildly symptomatic homecare COVID patients. Injectable steroids in hospitals should be given with strict monitoring of blood sugar and white blood cell counts, with constant observation for new symptoms.
- Be vigilant for any of the symptoms and warning signs of Mucormycosis. Seek immediate medical consultation and treatment.
- Avoid self-medication and over-the-counter (OTC) use of antibiotics, antifungals, and corticosteroids. These medicines should be used under the strict guidance and monitoring of a medical practitioner.
- Medicines like antibiotics, antifungals and immunosuppressants should be used judiciously in hospitals. Drugs like tocilizumab etc. should be used only in select patients for a brief duration, who conform to the indication of cytokine storm.
- Hygienic oxygen delivery should be maintained in hospitals. Sterility of industrial oxygen diverted for medical use should be strictly ensured. Water used for the humidifiers of oxygen should be clean, sterile, and changed frequently. The nasal cannula and masks used for oxygen delivery should be cleaned regularly.
- Personal hygiene. Wash and sanitize hands frequently. Wash face, hands and feet after contact with soil, plants, rotting fruits-vegetables, wood or possibly contaminated water. Wear mask with gloves and proper footwear while handling such sources. Keep wet garbage covered and dispose it regularly.
- Steam is not indicated routinely in COVID patients. Home steamers should be used with distilled/sterilized water, and be properly cleaned and dried before each use.
- Nose and mouth hygiene should be maintained. The nose can be cleaned with sterile saline drops/spray. Brush your teeth twice daily. Rinse mouth after meals and after coming from outside. Gargling with salt water or antiseptic (like betadine) may be done twice daily. Mouth ulcers should be treated timely.
- Mask hygiene should be maintained, and one should not wear wet or damp masks. Change disposable masks frequently every 4-6 hours. Cloth masks should be washed after every wear. After removing mask, wash your hands and face well.
Also read:
For any query, additional information or to discuss any case, write to info@drvarsha.com, and be assured of a response soon.
Reference: ICMR Mucormycosis Advisory