
COVID home care and isolation is an effective way of treating the majority of people infected, and the following important points can help in the right guidance and timely action.
The information below pertains to the first and second wave of COVID in 2020-2021. There has been no change in clinical protocol for variant strains. Variants like Omicron are suspected with S gene drop out in RTPCR, in which case additional genome testing may be done.
WHO IS CONSIDERED OR SUSPECTED TO HAVE COVID
One is considered as a case of COVID and should isolate immediately when
- RT-PCR or RAT COVID test is positive.
- RT-PCR is negative, but HR-CT chest scan was done on strong suspicion which revealed typical COVID-induced lung changes.
One is suspected of having COVID and should also isolate and self-monitor if:
- RT-PCR test is pending/negative, but symptoms are strongly suggestive of COVID like loss of smell/taste, fever, cough, sore throat, cold, body ache, headache, fatigue, nausea-vomiting, etc. (The Omicron variant may not present with loss of smell/taste).
- RT-PCR is pending/negative, but any of the above symptoms are present and there is a history of being in close contact with COVID positive family/household member in the last 7-10 days.
IDENTIFYING DAY 1 OF ILLNESS
- It is important to record the first day of illness as accurately as possible, for monitoring the course of the disease and taking timely action.
- For people with symptoms: Day 1 is the day one first started experiencing symptoms (fever, sore throat, cough, cold, body ache, fatigue/weakness, loss of smell/taste, headache, indigestion, etc.)
- For asymptomatic positive people (without symptoms but tested due to contact with COVID case, travel, or other requirements): Day 1 is the day the nasal/throat swab was taken for testing.
MONITORING AND DECIDING ON HOME CARE OR HOSPITALIZATION
- On diagnosis or suspicion of COVID, a treating physician should immediately be contacted and briefed to oversee your progress and treatment. The doctor will start appropriate medicines and supplements, and may also advise blood tests only if required like CBC, CRP, and other inflammatory markers. CT scan of the chest may be advised only in certain high-risk cases, or on high clinical suspicion, and at the appropriate time.
- Daily monitoring of oxygen saturation by the pulse oximeter, and temperature by an oral thermometer, is mandatory every 4-6 hours for 14 days. An individual chart of the same should be maintained day-wise.
- Isolation and treatment can be done at home if the oxygen level is being maintained at 94% or above and there is no breathlessness. The isolation room should be well ventilated (having openable windows) with an attached toilet. If home isolation is not possible due to other family members not being infected and the absence of a separate room, shifting to COVID care isolation centers (repurposed care centers – not hospitals) can be considered.
- 6-minute walk test – This should be done at least once daily for 14 days. Walk for 6 minutes at a normal pace in your room, and measure oxygen saturation just before and after. If the oxygen level decreases by more than 3-5% (for example if 99% falls to 94% or less; 95% falls to 92% or less), it can suggest ‘happy hypoxia’ (subclinical oxygen deficiency) which is an alert for compromised lung function and risk/tendency for falling oxygen levels.
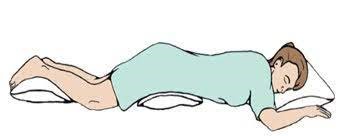
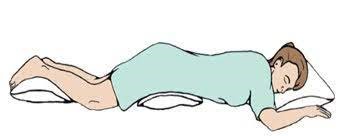
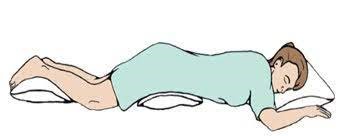
- Proning – This is a technique (as shown) of lying on the belly with a pillow under your head and neck, lower belly and thighs, and legs. This should be done 2-3 times daily (not within 1-hour post-meals). While lying prone, 5-10 deep breaths should be taken every 5-10 minutes. This helps improve lung ventilation and function, and can bring up intermittent dips in oxygen saturation of 90-94% above the 94% desired mark in many cases. (Note: People with obesity, spine/joint or heart problems, and pregnant women are advised not to do proning).
- Hospitalization should be considered in the following cases after more detailed evaluation in consultation with the treating physician:
- breathlessness or chest pain/pressure
- oxygen saturation constantly at or <94% for three consecutive readings in a day, not improving by proning, or dropping anytime below 90%
- high-grade fever (>101 deg F), and cough with phlegm beyond the first 3-5 days of illness, not responding to medications
- feeling very sick or weak, not able to eat or take medicines orally
- mental confusion, disorientation or reduced consciousness
- associated comorbidities (uncontrolled diabetes, illness of heart, lung, kidney or liver, cancer and post-surgery/transplant)
- HR-CT chest showing severe lung involvement
- high or rapidly rising levels of CRP along with persistent moderate-severe clinical symptoms suggesting increasing inflammation or clinical deterioration.
HOME CARE AND TREATMENT
This treatment consists of the following components-
GENERAL HEALTH AND HYGIENE
- Drink plenty of water along with healthy liquids like coconut water, buttermilk, lemon juice, and fresh fruit juices. Remain well hydrated at all times.
- Eat a healthy diet with vegetables, fruits, nuts, curd, protein-rich foods like eggs or pulses, and turmeric milk. Avoid spicy, irritant and cold food items. Take meals at regular times.
- Vitamin supplements are usually given for improving health and immunity like vitamin C, D, B complex.
- Apart from proning sessions and 6-minute walk test, do only that much physical activity as you feel up to without getting tired. This can include relaxed or medium-paced walking in the room, pranayama breathing exercises and light body stretches.
- Gargling (with antiseptic betadine/chlorhexidine) can be done twice daily. Steam is not required routinely but may be taken once daily if nasal/throat congestion or phlegm is present.
- Keep the mind relaxed by reading and watching pleasant content, listening to music and having video chats with friends/family. Unnecessary panic, anxiety and stress can worsen health, and induce a feeling of breathlessness, palpitation and worsening of symptoms. This can lead to taking inappropriate decisions by you, your family or the treating physician.
- Wear 2 triple-layer disposable surgical masks or N95 mask when near a family member, care-giver or health worker who should also do the same.
- Sanitize with a 70% alcohol-based sanitizer or wash hands frequently for 30-40 seconds.
MEDICINES
All medicines should be taken as prescribed by the overseeing doctor in the dose and duration advised. Do not add or stop medicines, or change dosage/frequency on your own. Clinical symptoms and progress along with oxygen saturation are the best guides to treatment. Investigations and tests only play a supportive role.
- Fever-Pain medications – Paracetamol is prescribed for fever and body pain 4-6 hourly. Sometimes the doctor may add combinations with aceclofenac, mefenamic acid or naproxen but only in select cases when required.
- Cough-Cold medicines – Antiallergics (like levocetirizine and montelukast), or cough syrups may be prescribed for symptomatic relief.
- Antivirals – Ivermectin and hydroxychloroquine were part of the homecare protocol in some countries like India in the first and second wave in 2020-21, however apart from being economical their effectiveness or benefit especially with respect to the new Omicron strain are doubtful, therefore are now not routinely recommended. Antivirals like favipiravir or the new molnupiravir may be prescribed by the treating doctor in very selective cases depending on viral load, symptom severity, risk factors and comorbidities present, vaccination status, and clinical experience. Antiviral agents may help reduce viral shedding, recovery time and hospitalization risk. However, none of these medicines have definite or proven value in treating COVID. Therefore, do not panic if these medicines are not prescribed or available, and do not take these medicines on your own without a doctor’s prescription or advice.
- Antibiotics – These drugs like azithromycin and doxycycline are prescribed when a secondary bacterial infection is suspected. Symptoms like significant throat pain, difficulty in swallowing, and thick greenish-yellow mucus (phlegm) being coughed out, are suggestive. They are not to be used routinely.
- Corticosteroids – These drugs are commonly called steroids. They are not to be taken in the first week of symptoms (unless indicated for other reasons or conditions) as they can do more harm than good. In case of persistent symptoms like fever and cough beyond the first week with evidence of oxygen saturation being borderline or tending to fall below 94%, or rising blood inflammatory markers like CRP, the doctor may choose to prescribe these medicines. These may be given as inhaler (budesonide MDI), or as low dose oral tablets (methylprednisolone, dexamethasone, prednisolone). These medicines should never be started, modified or stopped without medical advice or monitoring.
- Other medicines – The doctor may give medicines for acidity and indigestion which is common due to the infection and the above medicines. There is currently no recommendation for blood thinners (anticoagulants) when in home care, and do not start any such medicines on your own. Medicines being taken for other conditions and comorbidities like heart disease, high BP, diabetes, cholesterol, etc. should be continued as before and the doctor informed about it. Drugs like remdesivir, tocilizumab, baricitinib, enoxaparin and high dose corticosteroids are not to be used in the home care setting and are for use only on hospitalization.
- Antibody cocktail – Recently biological monoclonal antibody treatments have been approved and made available in select hospitals for treating mild-moderate COVID patients 12 years or older at high risk for progressing to severe COVID, complications, and hospitalization. This includes those who are 65 years of age or older, are unvaccinated, or who have certain associated comorbid medical conditions like diabetes, hypertension, heart/kidney/respiratory conditions, high obesity (BMI of 35 or more), and immunosuppressive disease or therapy. These agents are given together as a single intravenous infusion and act specifically against the spike protein of the coronavirus to prevent its entry into human cells. These agents work best if given within 72 hours of symptom onset (maximum within a week). They are not to be used in already hospitalized patients and those requiring oxygen therapy or ventilation. Their efficacy against the Omicron variant is not established.
OXYGEN
- Oxygen therapy in home care may be rarely needed only in case of breathlessness and falling or persistently low oxygen levels in the event of non-availability of immediate hospital admission. It may also be needed for those patients with respiratory comorbidities like COPD or ILD.
- Home-based oxygen cylinders and concentrators are to be used only temporarily to buy time and not as a substitute for hospitalization, as firstly these may not deliver the recommended and standardized flow rate and concentration of oxygen, and secondly, there may be a need for other injectable medicines at this stage to tackle the inflammation and disease severity.
- Oxygen delivery devices should be procured and used only under a doctor’s guidance.
UNDERSTANDING THE COURSE OF THE DISEASE
- It is important to note that the disease course consists of the first week of viremia (viral replication) and the second week of inflammation (due to the body’s immune response). The majority of people show a decline in symptoms with recovery after the first week. The Omicron variant particularly is mild, and symptom recovery is common in 3-5 days.
- If symptoms persist beyond 7 days, it is important to be under close monitoring by a physician. At this time some people doing well in home care can deteriorate with falling oxygen saturation due to disease progression. Therefore, monitoring of symptoms especially fever and cough with temperature and oxygen saturation is important till the end of the 2nd week.
- The doctor may also advise some blood tests in the 2nd week to check progress and pick up signs of disease progression and deterioration.
- A person is considered recovered from COVID if at least 7 days have elapsed after the onset of symptoms with no fever present for 3 consecutive days and oxygen saturation maintained >94%. Thereafter an additional one-week self-care period and wearing of mask are recommended while resuming public contact.
- No RT-PCR or RAT test is required post-recovery for COVID cases or for asymptomatic household contacts. The latter should self isolate and monitor for a week, and test if symptoms appear.
- COVID appropriate behavior of social distancing, mask, and sanitizer use (SMS) should be continued in accordance with health policies.
- Post recovery from COVID, there can be reduced lung capacity, energy levels, and general health-well being along with many symptoms for a few weeks to months. It is important to take adequate care and precautions in the 3 month period post-COVID recovery.
Also read:
Pulse Oximetry – 3 Important Points to Understand Usage and Interpretation
Temperature and Fever – Accurate Measurement and Interpretation
3 Effective Techniques to improve Breathing capacity and control
Mucormycosis or Black Fungus – Awareness, Precautions and Timely Action
Differentiating Breathlessness due to COVID/Flu from that due to Anxiety
References:

