There are a number of sleep disorders, that can affect the duration, quality, and impact of sleep. In fact, sleep and its disorders are the areas of much research.
STAGES OF SLEEP
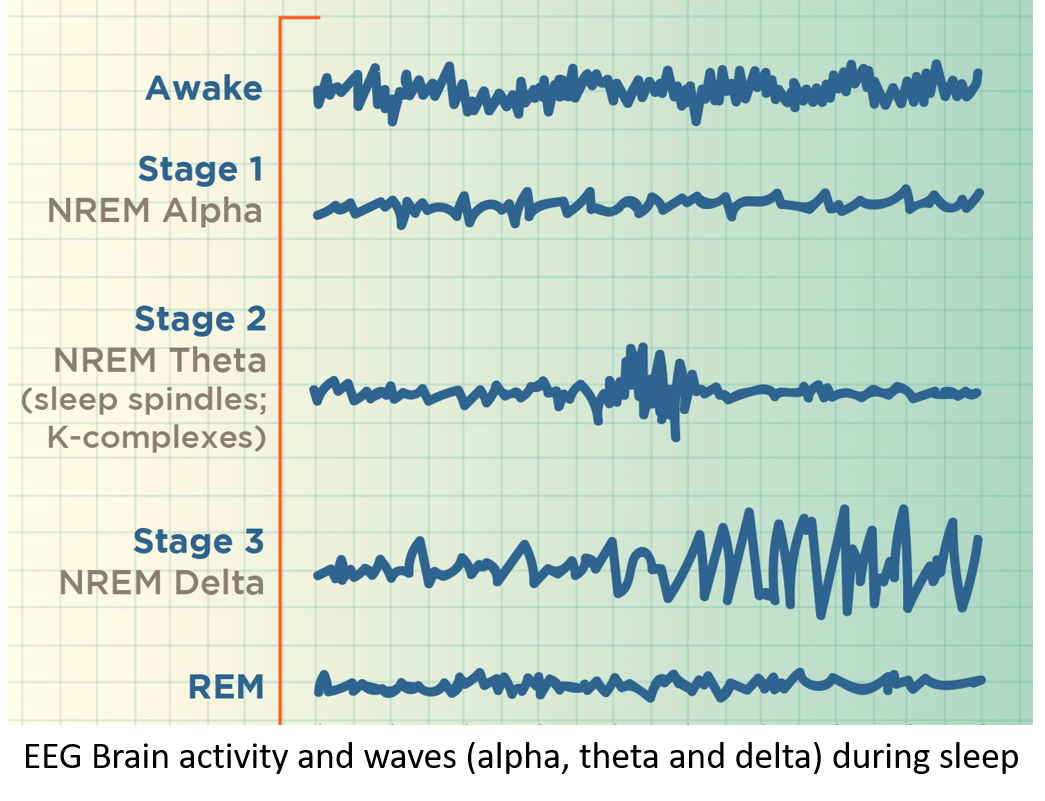
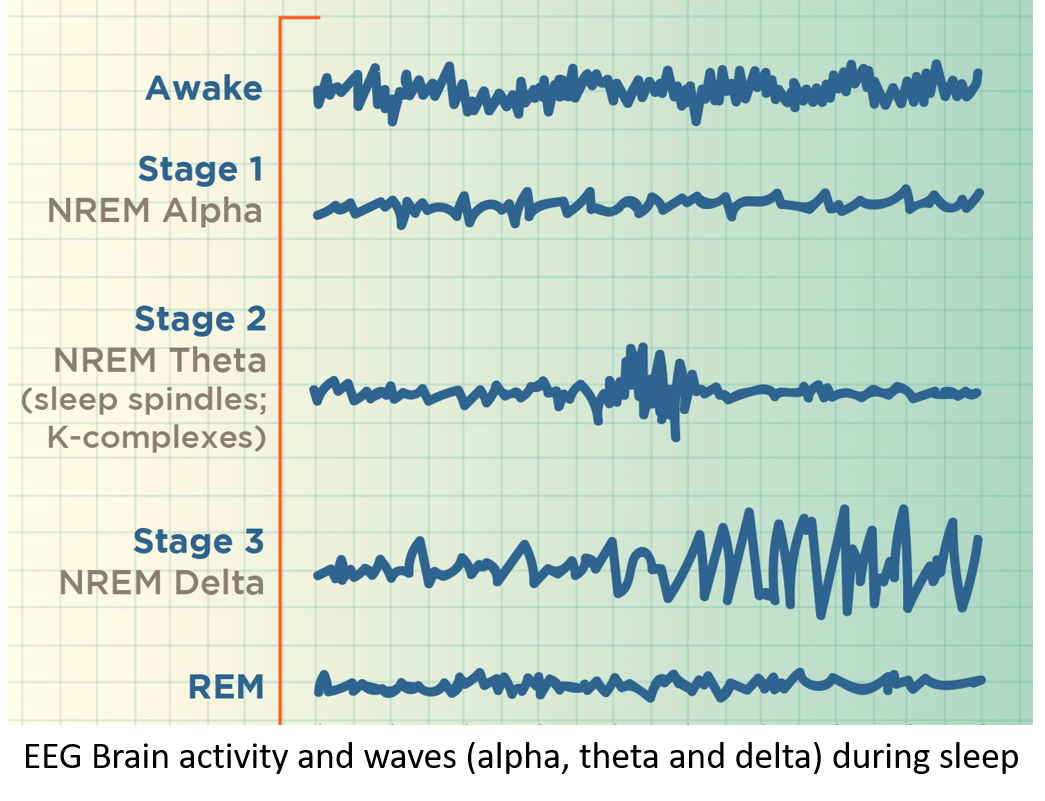
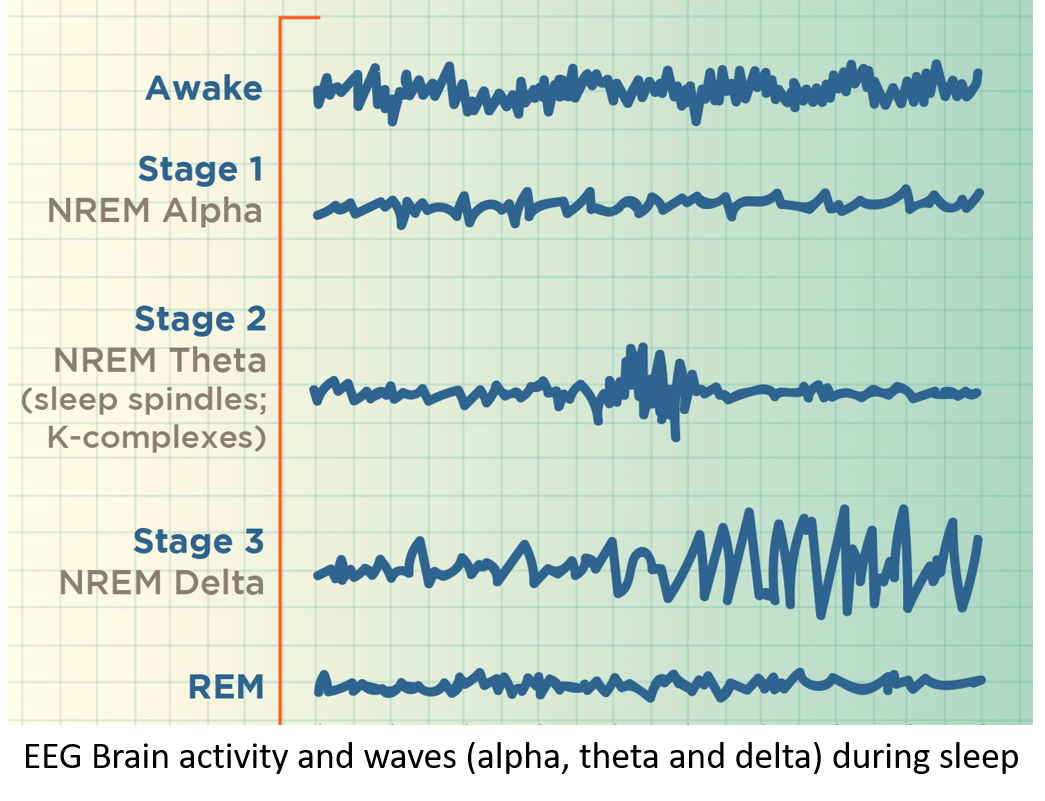
Sleep stages comprise of non-rapid eye movement (NREM) sleep as the first three stages of sleep followed by rapid eye movement (REM) sleep.
NREM-1 (5-10 minutes – 5% of total sleep) – It is the stage of transition from wakefulness to sleep. The brain activity, heart rate, breathing and eye movements begin to slow down, and the body starts to relax. The brain is still active in this stage.
NREM-2 (20 minutes/cycle – 50% of total sleep) – In this stage the body relaxes further, awareness of surroundings diminishes, body temperature drops, eye movements stop, and the breathing and heart rate become more regular. It is a stage of processing and consolidating the day’s memories by the brain.
NREM-3 (20-40 minutes/cycle – 20-25% of total sleep ) – It is the stage of deep sleep when it is difficult to be woken. The heart rate and breathing slow down, blood pressure drops, and the muscles are relaxed. It is the stage of body repair and rejuvenation as well as consolidation of knowledge, experiences, learnings, and long-term memory.
REM– It is the stage of sleep beginning about 90 minutes after falling asleep, and accounts for 20-25% of total sleep. While the body’s voluntary muscles are immobilized, the brain is active (like while being awake), breathing is faster and irregular, and there is rapid eye movement (REM). It is a stage of consolidating emotional memories and also when dreams occur.
NREM-3 and REM are stages of deep sleep when the body rebuilds itself by strengthening its immunity, promoting growth, and repairing damaged tissues. The cycle of NREM-2, 3 and REM is repeated 4-5 times every night, every 90 to 110 minutes. The duration of REM sleep increases with every cycle starting with 10 minutes in the first cycle.
SLEEP DISORDERS
Sleep disorders may be classified as:
INSOMNIA
It is the most common among sleep disorders and includes difficulty in falling asleep at night, maintaining or staying asleep, waking too early with the inability to fall asleep again, and decreased quality of sleep causing daytime sleepiness, tiredness or impacted functioning.
Read in detail: Insomnia and not getting enough sleep
HYPERSOMNIA
It is also called hypersomnolence disorder and refers to excessive daytime sleepiness (EDS), increased time spent sleeping, or difficulty in staying awake during the day. People who have hypersomnia can fall asleep anytime in the day thereby impacting and increasing risk during work, performance, daily activities, and driving.
Primary hypersomnia is attributed to abnormal sleep-wake control by the brain. Secondary hypersomnia can occur because of:
- Insomnia and poor sleep at night
- Sleep apnea
- Increase in weight or obesity
- Hypothyroidism
- Neurological conditions like multiple sclerosis, Alzheimer’s and Parkinson’s disease
- Head injury
- Alcohol or narcotic drugs abuse
- Mental health disorders like depression, bipolar disease.
- Use of prescription sedatives, tranquilizers, anti-anxiety pills, antihistamines, decongestants etc.
- Kidney or liver disease
Narcolepsy
Narcolepsy is a chronic sleep disorder of uncontrollable daytime drowsiness, sudden attacks of sleep, inability to stay awake for long, and significant disruptions in daily activities. One may fall asleep even while performing a task like writing, typing or driving, and continue to perform that task while asleep with no recollection of what was done on waking.
Narcolepsy has been linked to deficiency or destruction (due to a mistaken recognition by the immune system) of a brain chemical called hypocretin (also called orexin), which regulates sleep. Narcolepsy may be type 1 when it is accompanied by a sudden loss of muscle tone (cataplexy) triggered by strong emotion, or type 2 without cataplexy. People with narcolepsy often transition quickly to REM sleep, usually within 15 minutes of falling asleep. They also sometimes experience sleep paralysis, and vivid hallucinations, while falling asleep (hypnagogic hallucinations) and while waking from sleep (hypnopompic hallucinations) that can feel real and scary.
DIAGNOSIS AND TREATMENT OF HYPERSOMNIA
Temporary hypersomnia is just the body’s way of making up for inadequate sleep. If hypersomnia is persistent and impacts day-day functioning, it’s best to seek medical consultation. The treating doctor will analyze the course of the symptoms, conduct a physical examination and may order basic blood tests, and brain imaging tests like CT/MRI where needed. A psychological evaluation is also recommended to manage underlying depression or other conditions.
Sometimes a test called polysomnography is performed overnight at a sleep center, that monitors brain activity, eye movements, time spent in reaching and maintaining various stages of sleep, heart rate, oxygen levels, and breathing, to enable better diagnosis and treatment.
Treatment involves lifestyle measures including a nutritious diet, adequate exercise and physical activity, weight management, stress management, and avoiding alcohol and drug/substance abuse. Regularizing sleep-wake timings and ensuring adequate (8 hours) quality sleep at night, along with maintaining sleep diaries/records and monitoring day-time naps is most important.
Medicines may be prescribed in required cases, especially in narcolepsy. These include stimulant drugs like modafinil and armodafinil, and some newer ones like solriamfetol, pitosilant and sodium oxybate, the latter two being useful drugs in type1 narcolepsy. Conventional stimulant medicines like methylphenidate or amphetamines are sometimes prescribed but they have high addiction potential. Anti-depressant medicines (SSRIs, SNRIs, and TCAs) have also been found to be beneficial in some cases. All medicines mentioned have some side effects and are to be taken under strict medical advice and monitoring only.
Sleeping Sickness
PARASOMNIA
This refers to unnatural and disturbing events that disrupt sleep. Parasomnia can occur while falling asleep, during sleep, or while waking from sleep. Parasomnia can occur in both Non-REM or REM phase of sleep.
Non-REM sleep disorders (also called arousal disorders), include parasomnias that involve physical and verbal activity. One is not completely awake or responsive to interaction or intervention during the event, with no or little memory of the same the day after. These events are:
- Sleep terrors: Waking up suddenly in a terrified state, sometimes screaming and crying, along with physical signs like sweating, palpitations, fast breathing, dilated pupils, etc. (lasts for half-few minutes).
- Sleepwalking (somnambulism): Getting out of bed and walking with eyes wide open, and also performing tasks that may sometimes increase the risk of injury/accidents. It may also be accompanied by sleep talking or sleep-related eating disorders (eating foods often not a normal part of the routine diet).
- Confusional arousals: Being partially awake with eyes open, but disoriented in time and space, sometimes with emotional disturbance, speech, and comprehension (lasts for a few minutes to an hour, and is more common in childhood).
REM sleep parasomnias can often be recollected and described if woken up during the event. These parasomnias are more common during periods of stress, trauma, extreme fatigue, fever, illness and high alcohol intake. These include:
- Nightmares: Vivid, scary, dreams that cause significant fear and anxiety, sometimes waking and difficulty going back to sleep.
- Sleep paralysis: Inability to move body or limbs during sleep, usually while falling asleep or waking up. The episode can last for a few minutes and can be terrifying, but can be stopped if touched by family member/bed partner.
- REM sleep behavior disorder (RSBD): Acting (hitting out, punching, grabbing, kicking, fighting) or talking (scolding, swearing, shouting, laughing). It is more common in the elderly especially with neurological conditions.
Other parasomnias include exploding head syndrome (hearing a loud explosive crashing sound or seeing light flashes), catathrenia (groaning and grunting in sleep), enuresis (bedwetting) in adults/older children, hallucinations, and sexosmia (performing sexual acts during sleep).
Risk factors for Parasomnia
These conditions increase the risk and frequency of suffering from parasomnias.
- Disturbed sleep and transitions into sleep stages,
- Circadian rhythm sleep-wake disorders – irregular sleep-wake schedules (jet lag or shift working) where sleep cycle is not in sync with the natural light-dark cycle.
- Sleep apnea
- Alcohol or substance abuse
- Children with neurologic or psychiatric health issues like epilepsy, attention-deficit hyperactive disorder (ADHD) or developmental delay.
- Elderly or those with neurodegenerative conditions like stroke, multiple sclerosis, Alzheimer’s and Parkinson’s disease
- Narcolepsy
- Fever and/or body pain
- Severe stress
- Anxiety-Depression
- Head injury
- Headaches and migraine
- Brain tumors, or infection (encephalitis)
- During pregnancy, hormonal imbalance, menstruation, perimenopause.
- Restless legs syndrome (RLS) -Uncontrollable urge to move legs due to uncomfortable sensations, seen in the evening and night after sitting or lying down for some time, and relieved by moving the legs or walking.
- Genetic predisposition or family history
- Drugs for sleep, anxiety, depression, and psychosis, certain drugs for high BP or convulsions, specific antibiotics and antiallergics.
DIAGNOSIS AND TREATMENT OF PARASOMNIA
Sleep disorders are often treated by a multispecialty team of a family physician, psychiatrist, psychologist, neurologist and sleep specialist. The treating doctor will analyze the course of the symptoms and seek a detailed history from both the individual with the sleep disorder as well as the bed partner and other family members. A general physical examination and basic blood tests and brain imaging tests like CT/MRI are also done where needed, to rule out any underlying cause. A psychological evaluation is also performed.
Sleep studies performed overnight at a sleep center include polysomnography, which monitors brain activity, eye movements, time spent in reaching and maintaining various stages of sleep, heart rate, oxygen levels, and breathing. A sleep video EEG (electroencephalogram) may also be done to record and observe brain activity during the parasomnia event.
Treatment involves a combination of lifestyle measures and medicines where needed.
Most important is maintaining a regular sleep-wake cycle, with a consistent time of going to bed and waking. Putting in place relaxing bedtime routines like a warm bath, listening to soothing music or reading, avoiding heavy exercise at night, and avoiding electronic gadget use at bedtime are recommended along with maintaining consistent timings of going to bed and waking.
A healthy nutritious diet should be taken along with avoidance of caffeine, alcohol and substances of abuse or recreational drugs.
Psychotherapy with counseling and cognitive behavioral therapy can help especially in underlying stress and anxiety-depression. Guided breathing and relaxation techniques at bedtime are also beneficial.
Maintaining safety of the home and surrounding environment is required to avoid injury and accidents during a parasomnia episode especially sleepwalking. These include removal of glassware, sharp items or sharp-edged furniture, and locking and installing alarms on the main door and windows.
Non-REM parasomnias are common during childhood and usually subside by adolescence. Reassurance to parents is all that is usually needed.
Medicines may be prescribed in persistent cases of non-REM parasomnia as well as for REM parasomnia. Anti-anxiety medicines (benzodiazepines) are prescribed for short periods (4-6 weeks) to improve sleep. Melatonin is a useful medicine to regularize circadian sleep-wake rhythm, improve sleep and transition into sleep stages especially REM sleep. Antidepressants may also be beneficial for some people.
SLEEP BREATHING DISORDERS
These include various forms of sleep apnea. Read on:
Snoring and Sleep Apnea – Causes and Simple Lifestyle Solutions
Also read:
Not getting enough sleep can be detrimental to health: Tackling Insomnia
Depression and Anxiety – Causes, Signs and Holistic Treatment
For any query, additional information or to discuss any case, write to info@drvarsha.com and be assured of a response soon
Reference: Sleep Disorder Guidelines


