Keratitis and scleritis refer to inflammation of the cornea and sclera respectively.
The front eye surface is made up of the transparent cornea in the center, and the conjunctiva. Below the conjunctiva is the outer layer of the entire eyeball called the sclera (or the white of the eye). Inflammation or diseases of these eye surface layers often manifest as redness of the eye.
Inflammation of the conjunctiva is called conjunctivitis (Read: CONJUNCTIVITIS)
KERATITIS
Causes
Keratitis is the inflammation of the cornea which is the outer central transparent portion of the eye. Keratitis may occur due to an infection or a non-infectious cause.
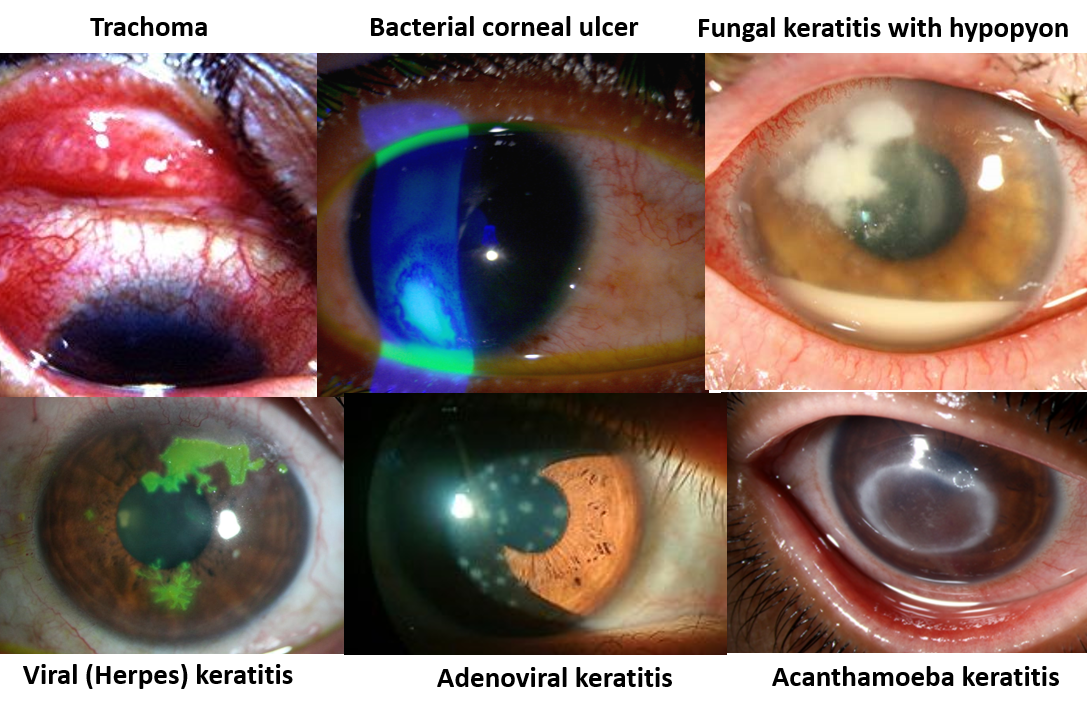
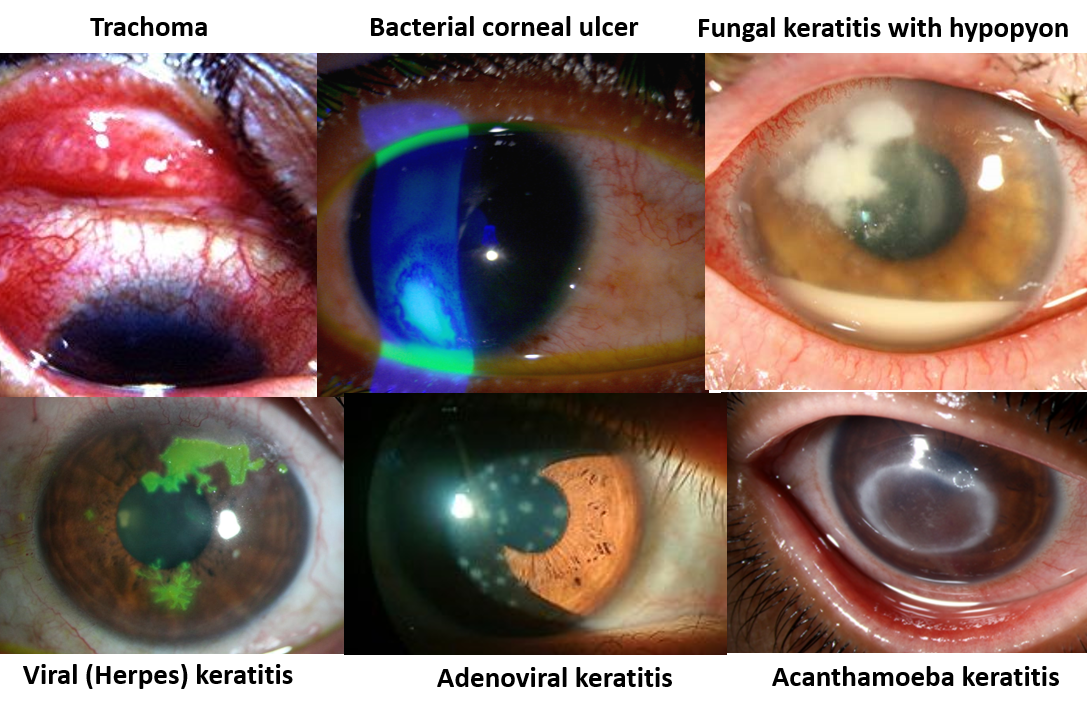
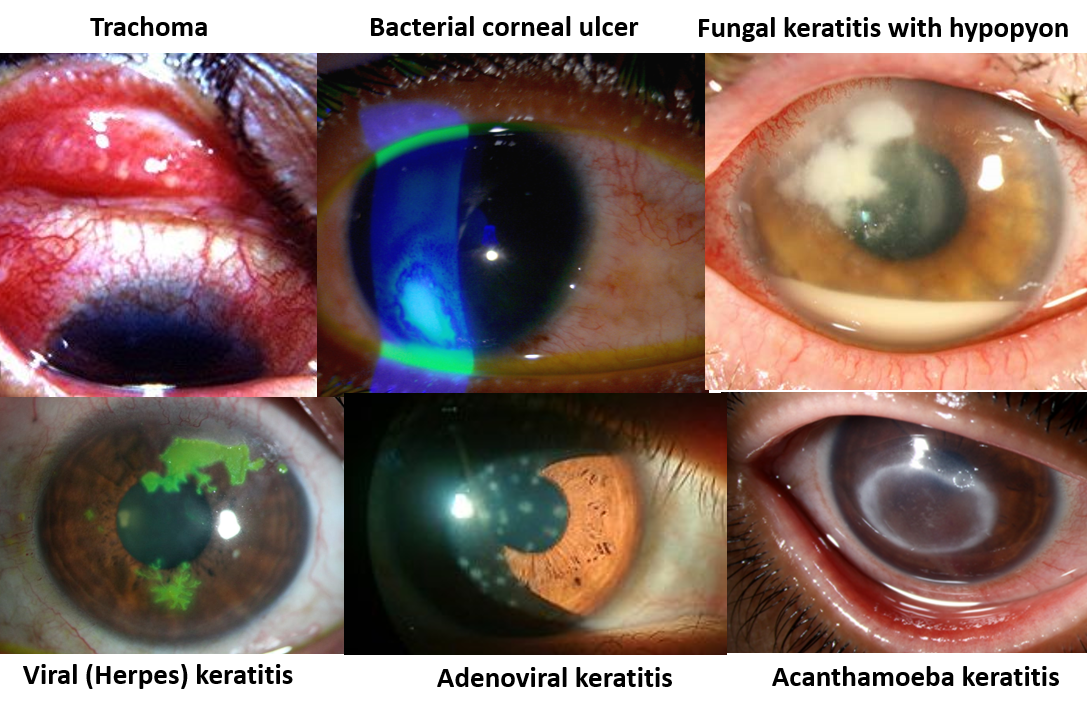
Infectious keratitis can be bacterial (Staphylococcus, Streptococcus and Pseudomonas), fungal (Aspergillus, Fusarium), viral (Herpes, Adenovirus) or parasitic (Acanthamoeba). Trachoma is keratitis caused by the bacteria Chlamydia, seen commonly in lower socioeconomic strata in underdeveloped countries, and is a common cause of preventable blindness.
Predisposing factors for corneal infection include swimming in contaminated water, wearing unclean contact lenses, working in agricultural fields, use of steroid eyedrops, etc. Hygienic measures like washing hands and eyes after exposure to an unclean environment, wearing protective goggles and swimming in well-maintained pools, and taking regular care of contact lenses, are important for prevention.
Non-infectious keratitis can be caused by injury or a foreign body in the eye, but these also increase the risk of developing infectious keratitis. Dry eyes also increase risk of corneal abrasions, infections and inflammation. Overwear of contact lenses can sometimes cause temporary non-infectious keratitis.
Neurotrophic keratitis is caused by damage to the nerve that carries sensations from the cornea. This leads to repeated corneal injury and poor healing leading to erosions, ulceration and inflammation.
Vitamin A deficiency can cause severe dry eye (xerophthalmia), corneal ulcers and sometimes clouding and softening of the cornea (keratomalacia). This is a significant problem in children from underdeveloped or poorer areas and is far rarer today due to the fortification of many food items with vitamin A as well as social programs for both nutrition awareness and administering vitamin A to children.
Symptoms and Signs
Symptoms include redness, pain and irritation, tearing, foreign body sensation, blurring or reduced vision and sensitivity to light (photophobia).
Infections can sometimes lead to the breakdown of the corneal surface in the form of small superficial dot-like erosions (punctate keratitis) or forming a corneal ulcer. There can also be associated pus (white blood cells and inflammatory fluid) between the cornea and lens (in the anterior chamber) called hypopyon.
Often keratitis may be accompanied by conjunctivitis, so is commonly called keratoconjunctivitis.
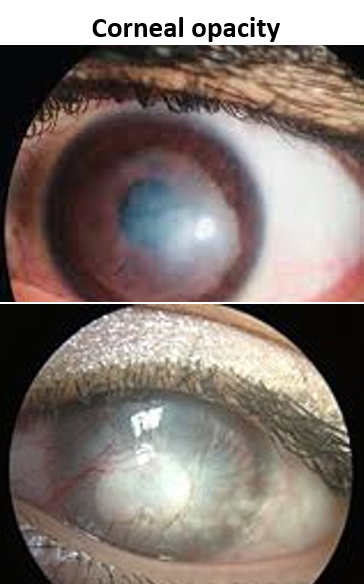
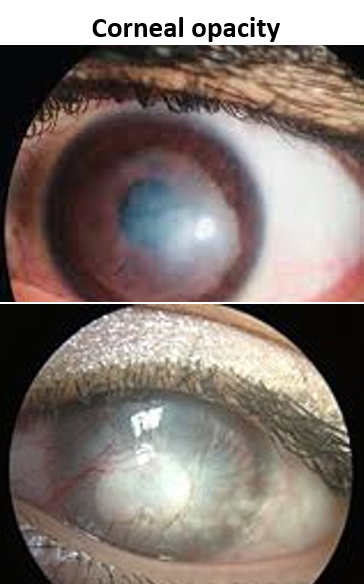
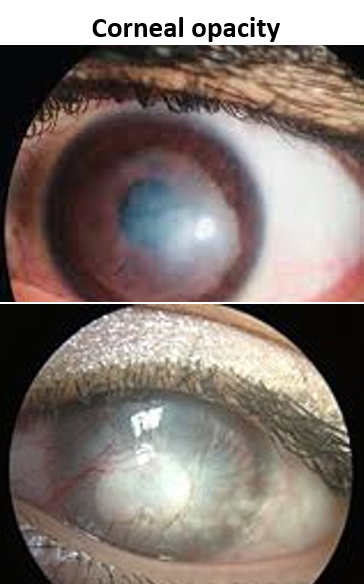
Healing of keratitis and corneal ulcers may cause corneal opacities that can impair vision, and may even cause blindness.
Management
A thorough evaluation is done by an eye examination with the slit lamp, and staining with fluorescein dye to demarcate the ulcer (ulcerated area of cornea stains green). Evaluation of the tear film and corneal sensitivity is also done. Based on the appearance and layer of corneal involvement, the keratitis may be given names like epithelial, nummular, disciform or interstitial.
Antibiotic eyedrops or ointments are the mainstays for infectious keratitis. Depending on the typical presentation of the corneal ulcer and keratitis, antibacterial, antifungal, antiviral or antiparasitic drops/ointments are prescribed. These drops may need very frequent instillation initially, and in some cases, treatment may be prolonged. In some cases, oral antibiotics may also be needed. An ulcer may sometimes need a short-term patch and bandaging of the eye to expedite healing.
For non-infectious non-ulcerated keratitis, and in the healing post-infectious stage of infectious keratitis, controlled use of corticosteroid eye drops is sometimes recommended to reduce inflammation and scarring.
In the case of neurotrophic keratitis, artificial tears eye drops are given. Such cases may also benefit from drops prepared from autologous (self) serum, a bandage contact lens, or amniotic membrane/conjunctival grafts.
For corneal opacities after healing that significantly impair vision, a corneal transplant (keratoplasty) may be needed.
SCLERITIS
Cause
Scleritis is inflammation of the white portion of the eye, the sclera. It is an uncommon and serious condition and is often associated with underlying autoimmune disorders like systemic lupus erythematosus (SLE), arthritis, ankylosing spondylitis, vasculitis, arteritis, systemic sclerosis, polymyositis, Sjogren’s syndrome, inflammatory bowel disease (IBD), and other connective tissue disorders. In such cases, it often involves both eyes. Scleritis may less commonly occur due to infections that may be bacterial (pseudomonas, mycobacterium), fungi, viruses or parasites. Rarely trauma may be a cause, but sometimes no cause is found.
Episcleritis refers to the inflammation of the surface membrane covering the sclera separating it from the conjunctiva. It is far less painful than scleritis and usually not serious.
Symptoms
Symptoms include redness of the eyes with pain and reduced vision. The redness may sometimes have a bluish tinge and may appear nodular with multiple round or oval elevated areas. Pain is the hallmark of scleritis and feels like a deep ‘inside the eye’ pain often worse with movement and at night, awakening one from sleep. A decrease in vision is often due to the extension of inflammation into the cornea (keratitis) or the uveal tissue (iris and ciliary body – uveitis/iridocyclitis). Corneal involvement can also cause tearing, and light sensitivity (photophobia). Inflammation of the eye muscles can restrict their movement and cause double vision.
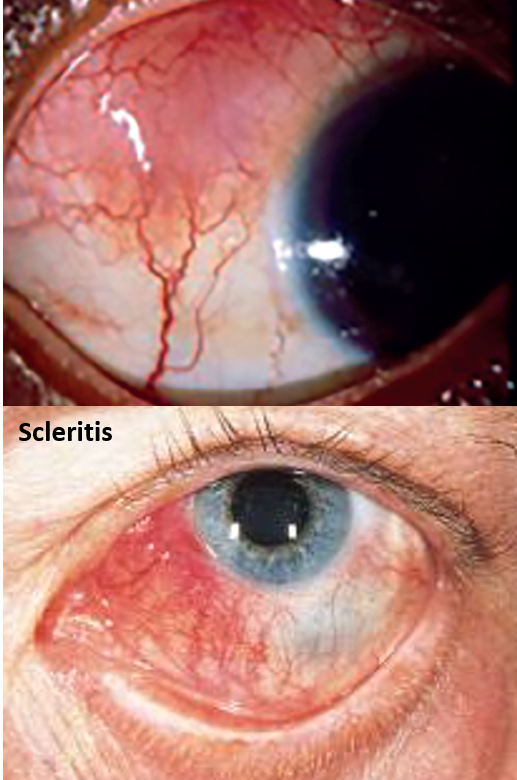
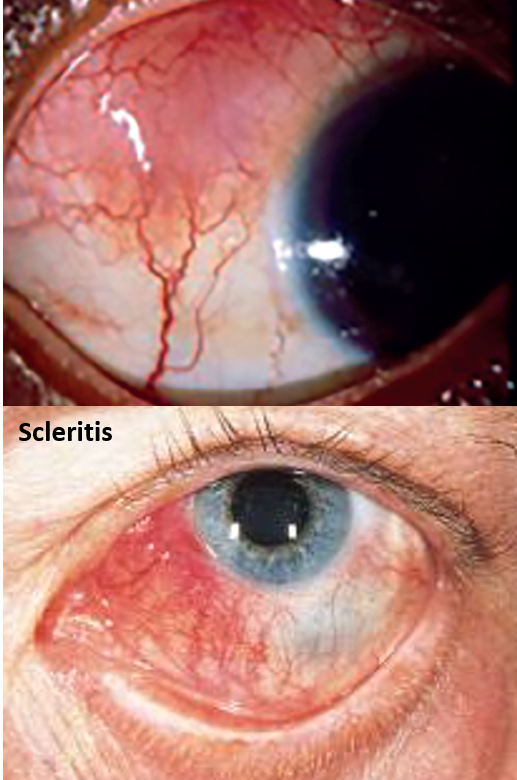
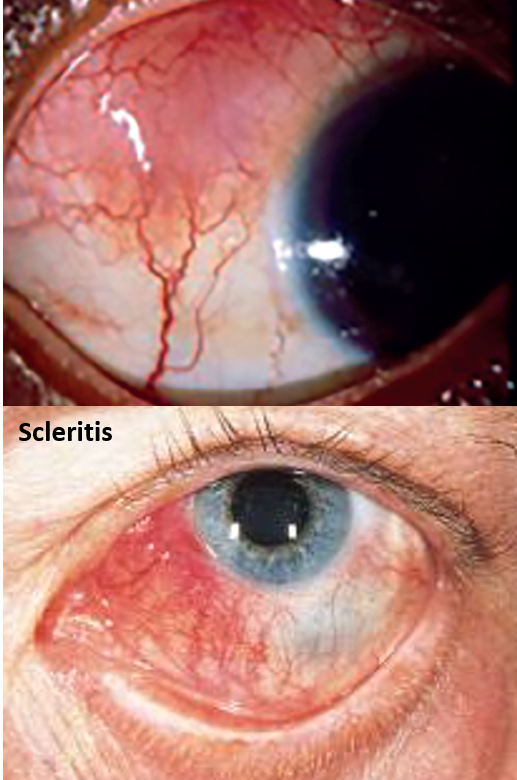
Complications can also include the development of glaucoma or cataract. If the back part of the sclera is involved the inflammation can also extend to the choroid and retina. Prompt diagnosis and treatment are of utmost importance as sometimes a severe form (necrotizing scleritis) can cause rapid destruction and loss of vision.
Management
Treating scleritis has to be a multispecialty approach as many systemic conditions are associated with scleritis that need to be investigated for, diagnosed, and managed.
Anti-inflammatory eye drops are given that may be corticosteroid drops or nonsteroidal anti-inflammatory (NSAIDs) drops. Antibiotic eyedrops are given in case of infectious scleritis. Corticosteroids may also be given as subconjunctival injections. In many cases, oral NSAIDs, corticosteroids and/or immune-modulating drugs like methotrexate, azathioprine, or cyclosporine are required. Biological injections like infliximab and adalimumab are also given in certain cases. Rarely surgical grafting may be needed in extreme cases.
Also read:
Vision Reduction and Loss – Understanding Causes and Points for Timely Action
Reference


