Assessing the functioning of the respiratory system (airways and lungs) is done through pulmonary function tests (PFT). These include measurement of:
- Lung Volumes and Capacity
- Respiratory Flow rates and Pressures
- Diffusing Capacity of Gases
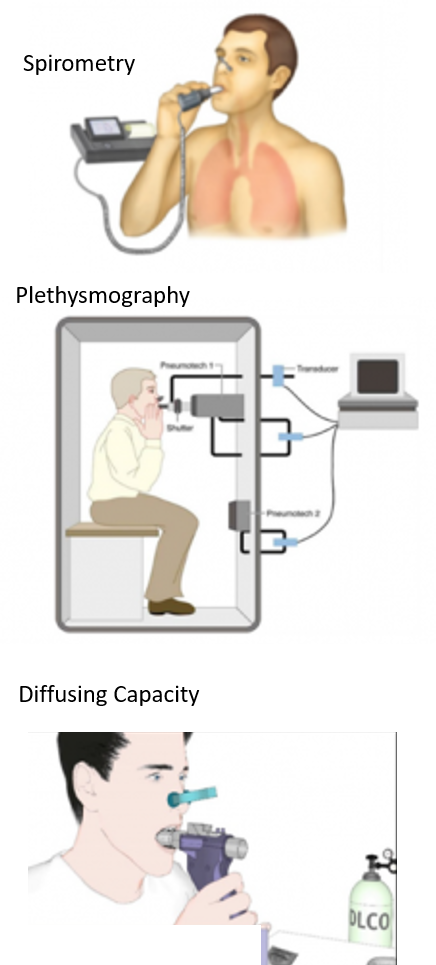
PFTs are performed by outpatient procedures called spirometry and sometimes an added test called plethysmography. These usually take under half-hour. PFTs require wearing loose clothing and removal of accessories. It is important that 2-3 hours preceding the test to not smoke, consume alcohol, eat/drink or exercise/exert. Routine daily medications can be had on the day of the test but symptomatic inhalers like short-acting bronchodilators should not be taken.
LUNG VOLUMES AND CAPACITY
Lung volumes (or respiratory volumes) are measures of air in the lungs at various times and stages of the respiratory cycle of inspiration and expiration. The lung volumes are then used to calculate different types of lung capacity. This helps to assess the functioning of the lung and type of lung disease. Lung volume normal values are based on gender, age, race, and body type (height/weight).
Decreased lung volumes and capacity may be seen in diseases of the lung, as well as those of the chest. The 3 most important lung volumes are assessed by spirometry – tidal volume, inspiratory reserve volume, and expiratory reserve volume. However, residual volume requires other tests like plethysmography.
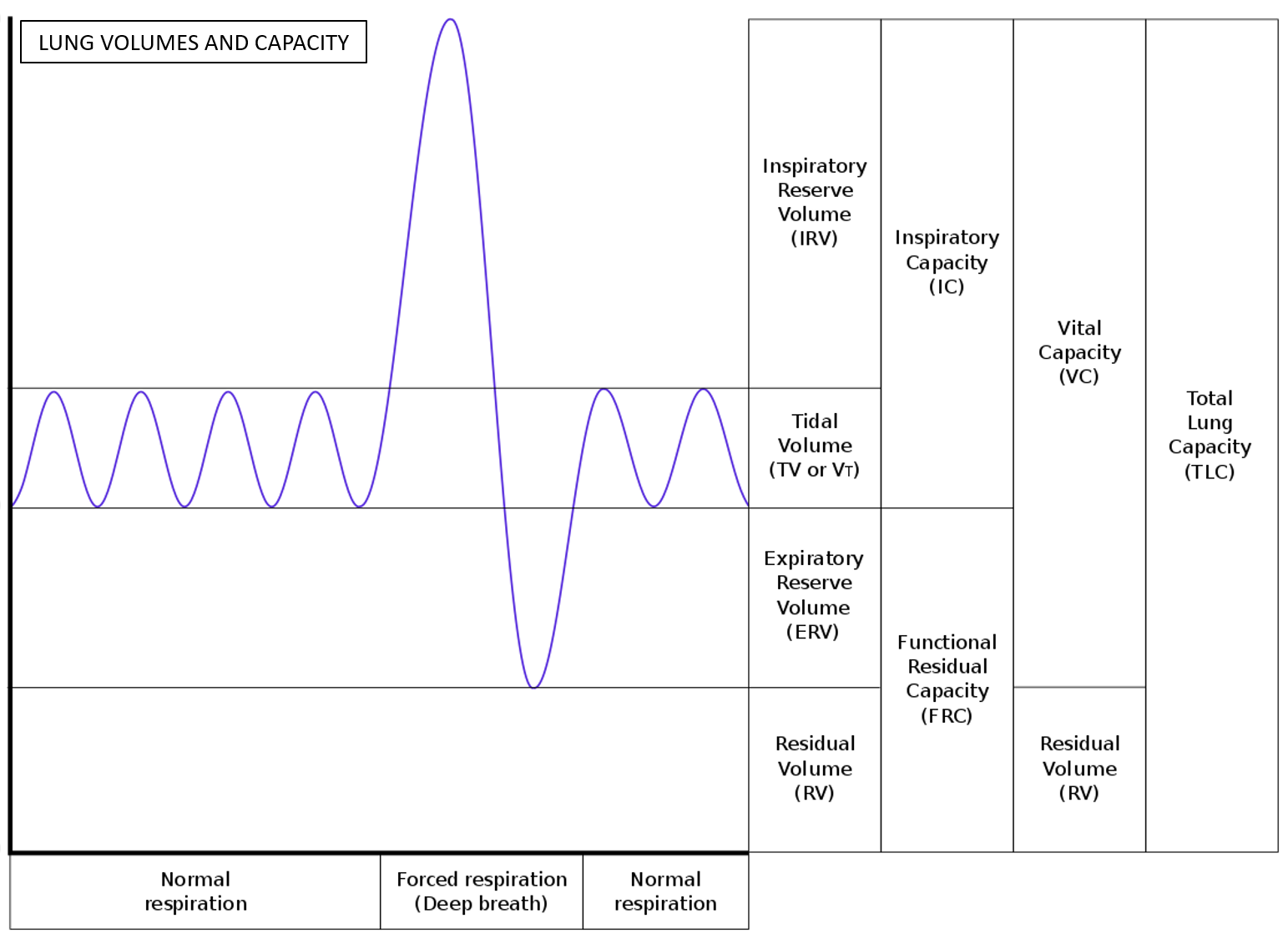
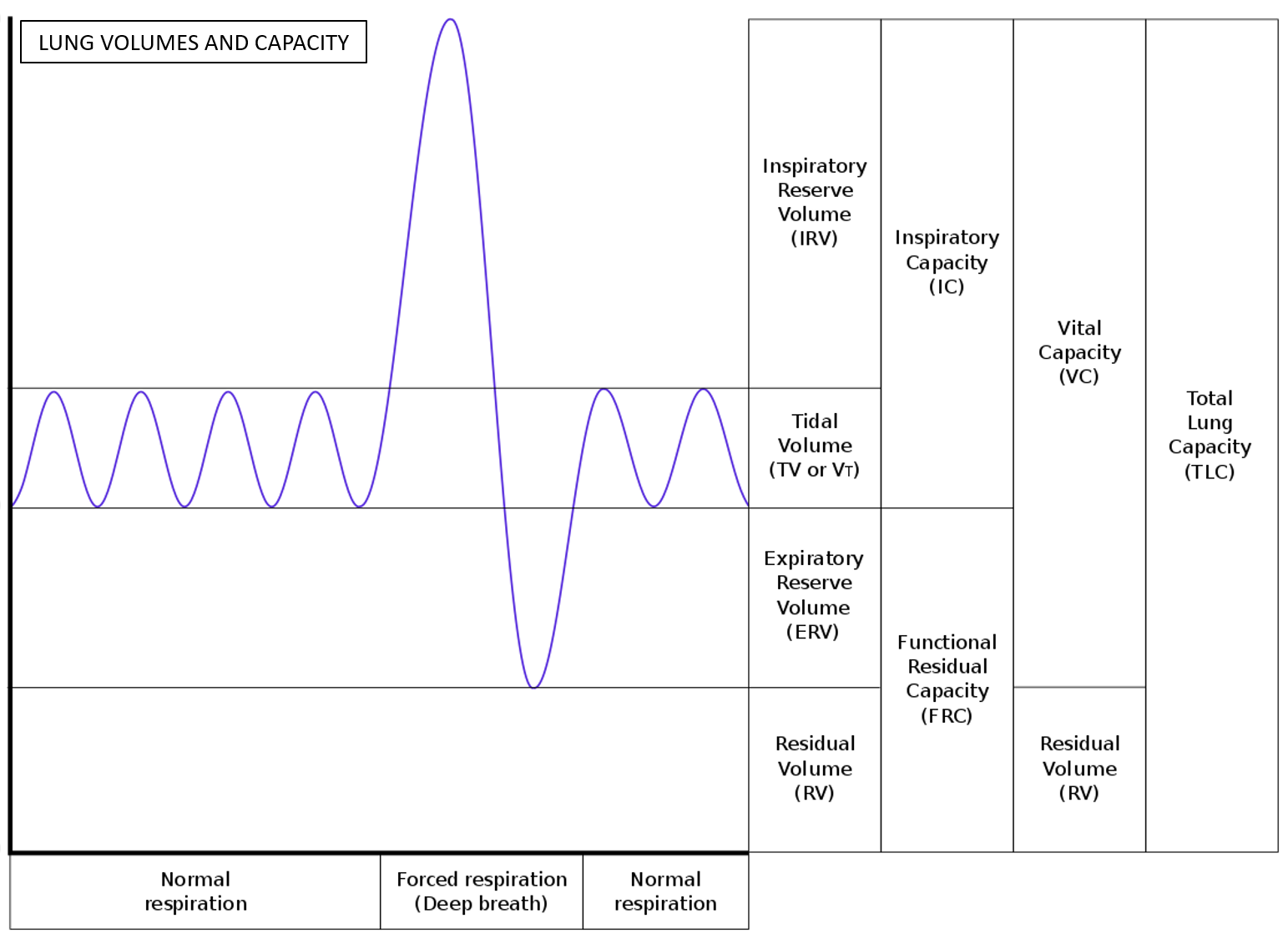
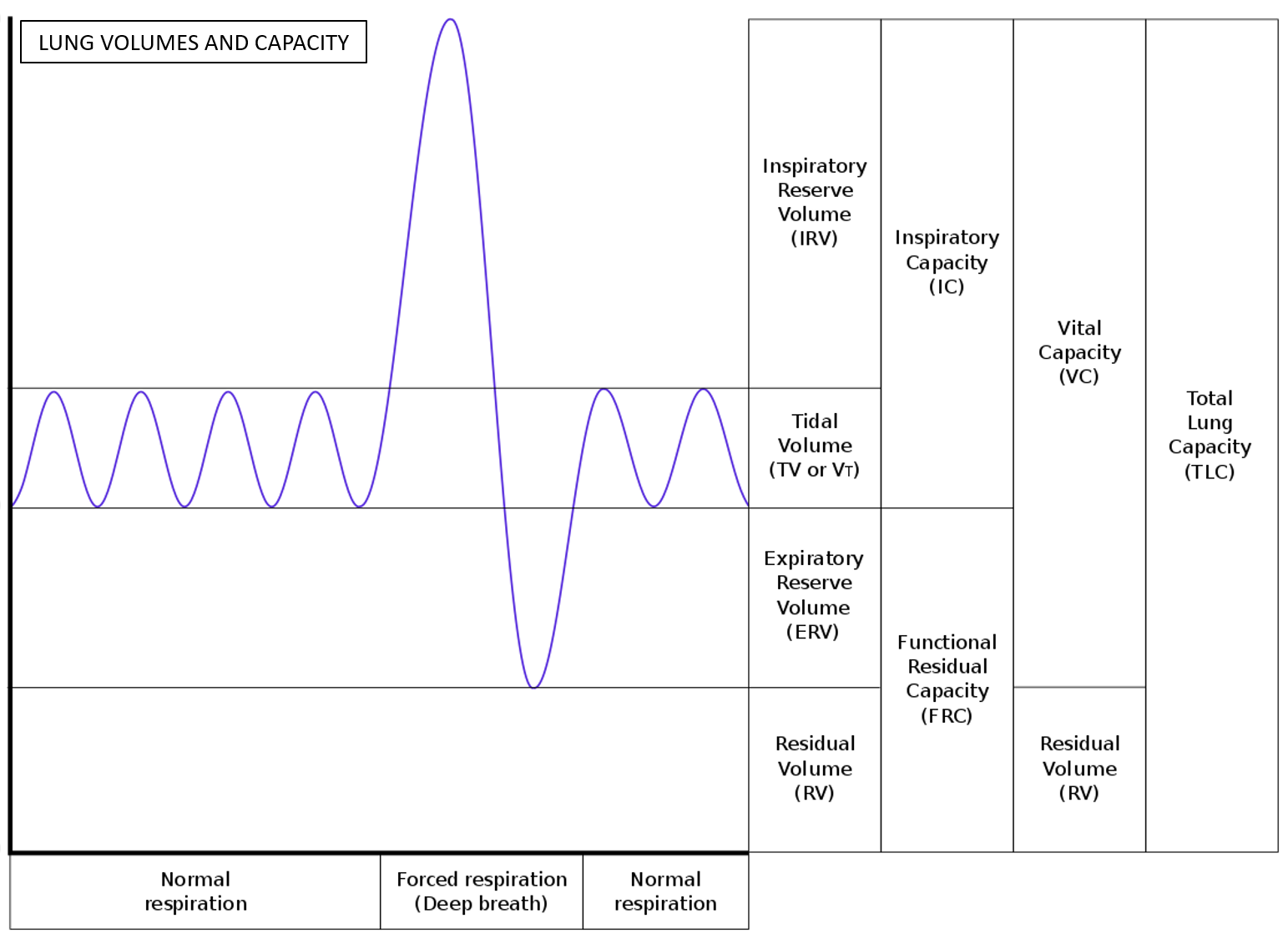
Tidal volume (TV) is the amount of air inhaled and exhaled in a normal respiratory cycle at rest. It gives an overall idea of the coordinated functioning of the systems involved in respiration – the airways and lungs, muscles of the chest, and respiratory center in the brain. The TV is around 0.3-0.5L (10% of vital capacity at rest, increasing to up to 50% of VC on exertion).
Inspiratory Reserve Volume (IRV) is the amount of air that can be forcibly further inhaled after the normal tidal volume. It is like a reserve that is used in deep breathing. The IRV is 2-3L.
Expiratory Reserve Volume (ERV) is the amount of air that can be forcibly further exhaled after the normal tidal volume. The ERV is 0.7-1.2L.
Residual Volume (RV) is the volume of air remaining in the lungs after maximal exhalation and is around 1.2-1.5mL.
Inspiratory capacity (IC) is the maximum volume of air that can be inhaled following a resting state. It is around 3.5L. (IC = IRV+TV)
Vital Capacity (VC) is the total amount of air exhaled after a maximal deep inhalation. It is around 4.5-5L. (VC = TV+IRV+ERV).
Total Lung Capacity (TLC) is the maximum volume of air the lungs can accommodate. It is around 6L. (TLC= TV+ IRV+ERV+RV).
Functional Residual Capacity (FRC) is the amount of air remaining in the lungs at the end of a normal exhalation. It is around 2L. (FRC = RV+ERV).
RESPIRATORY FLOW AND PRESSURES
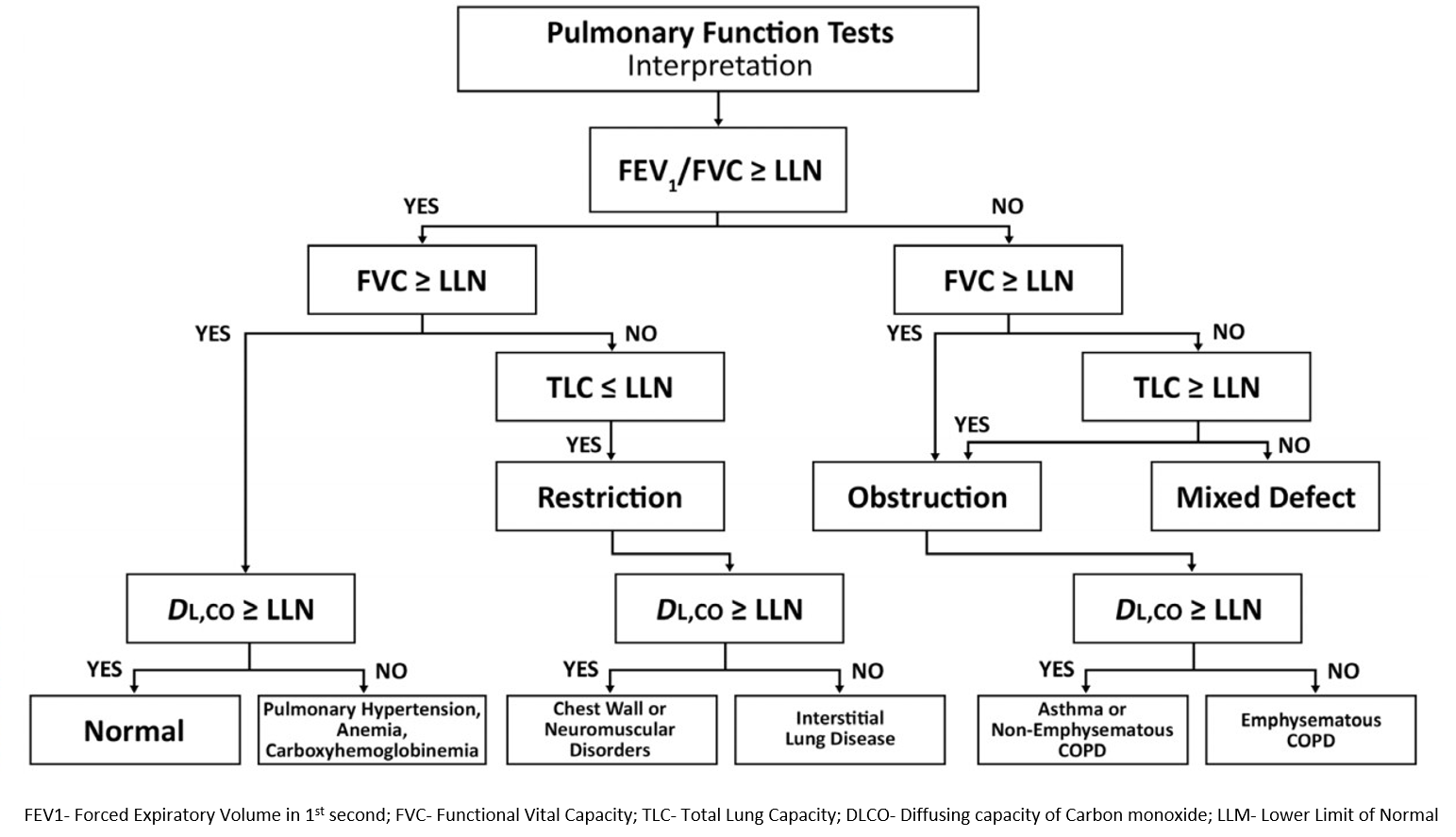
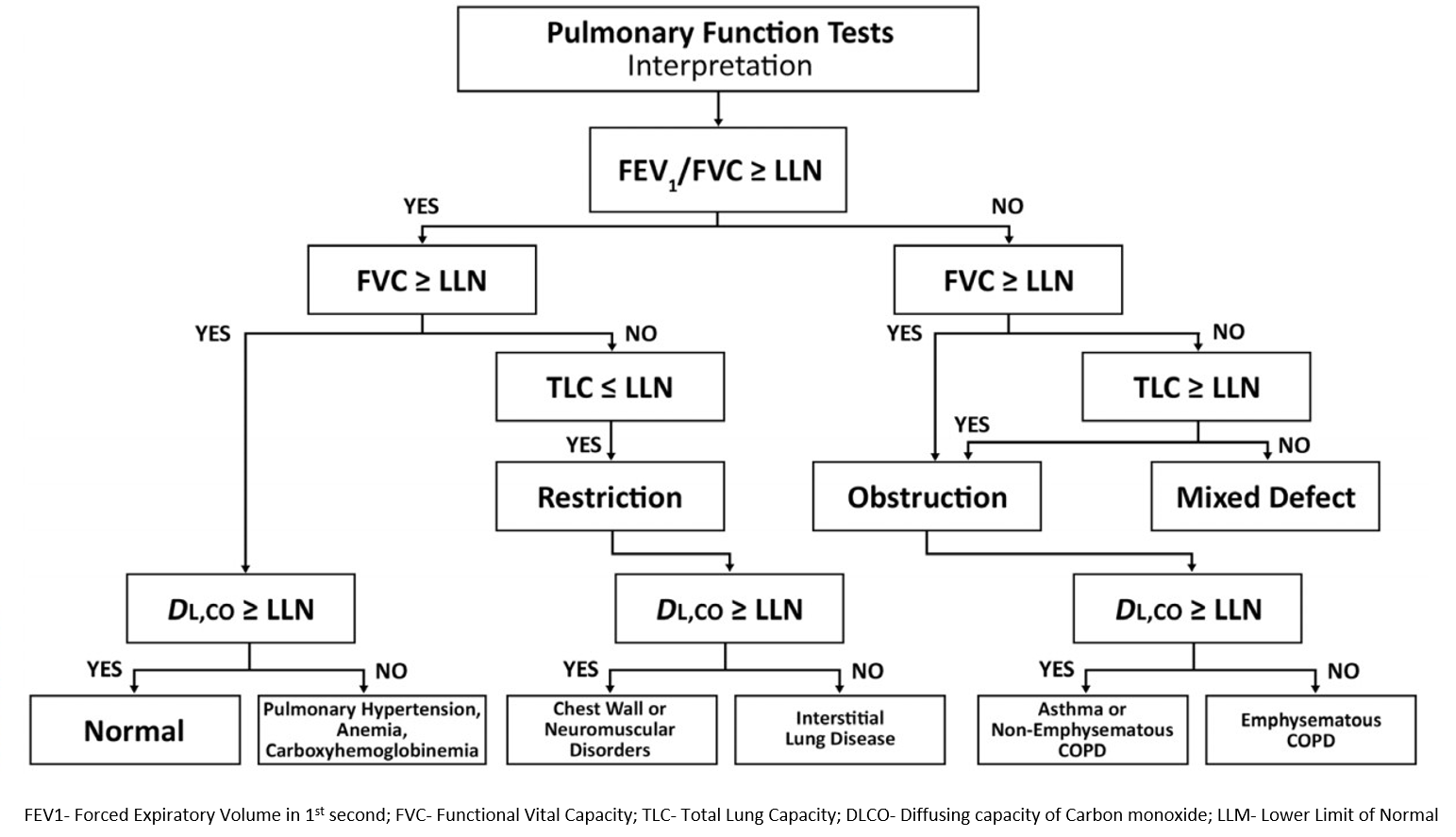
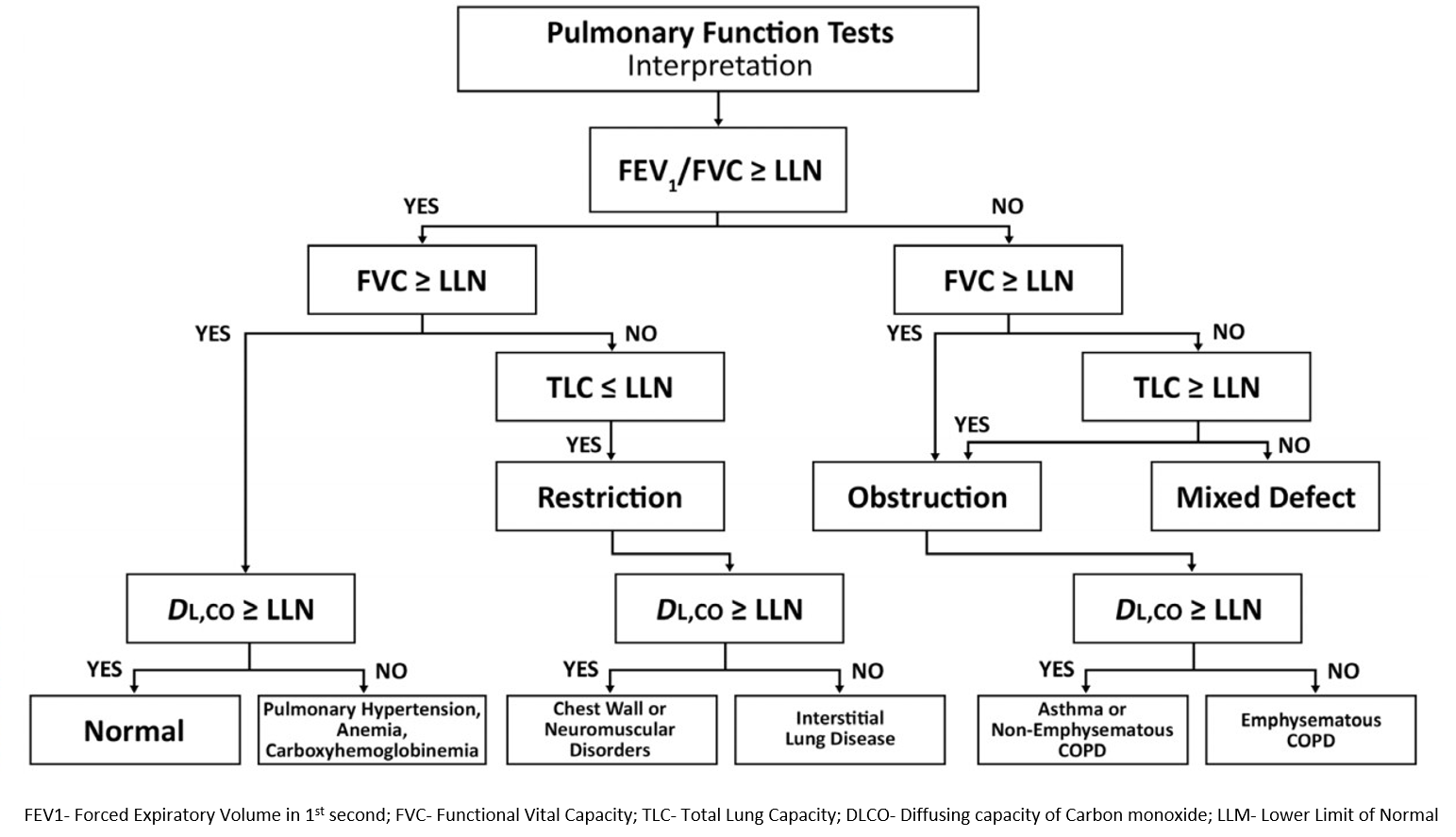
Flows and pressures reflect the functioning of the airway and the lungs. Predicted normal values are calculated and dependent on age, sex, height, mass, and ethnicity. The lower limit of normal (LLN) is accordingly provided. These values are useful in differentiating between obstructive diseases that primarily affect lower airways (like asthma and COPD) and restrictive diseases that reduce lung expansion and functioning (like interstitial lung disease-ILD and pneumonia).
Forced vital capacity (FVC). This is the amount of air exhaled forcefully and quickly after maximal inhalation.
Forced expiratory volume (FEV). This is the amount of air exhaled during the first, second, and third seconds of the FVC test. Usually, the amount of air exhaled in the first second (FEV1) is 80% or more of FVC.
Forced expiratory flow (FEF). This is the average rate of flow during the FVC test. The usual discrete intervals are at 25%, 50%, and 75% of the FVC exhaled (FEF25, FEF50, and FEF75). It can also be given as a mean of the flow during an interval, usually 25–75% (FEF25–75%).
Peak expiratory flow rate (PEFR). This is the fastest rate measured during the FVC test.
The above tests may sometimes be repeated after giving a bronchodilator medication, which helps establish diagnosis and response to treatment.
FEV1/FVC
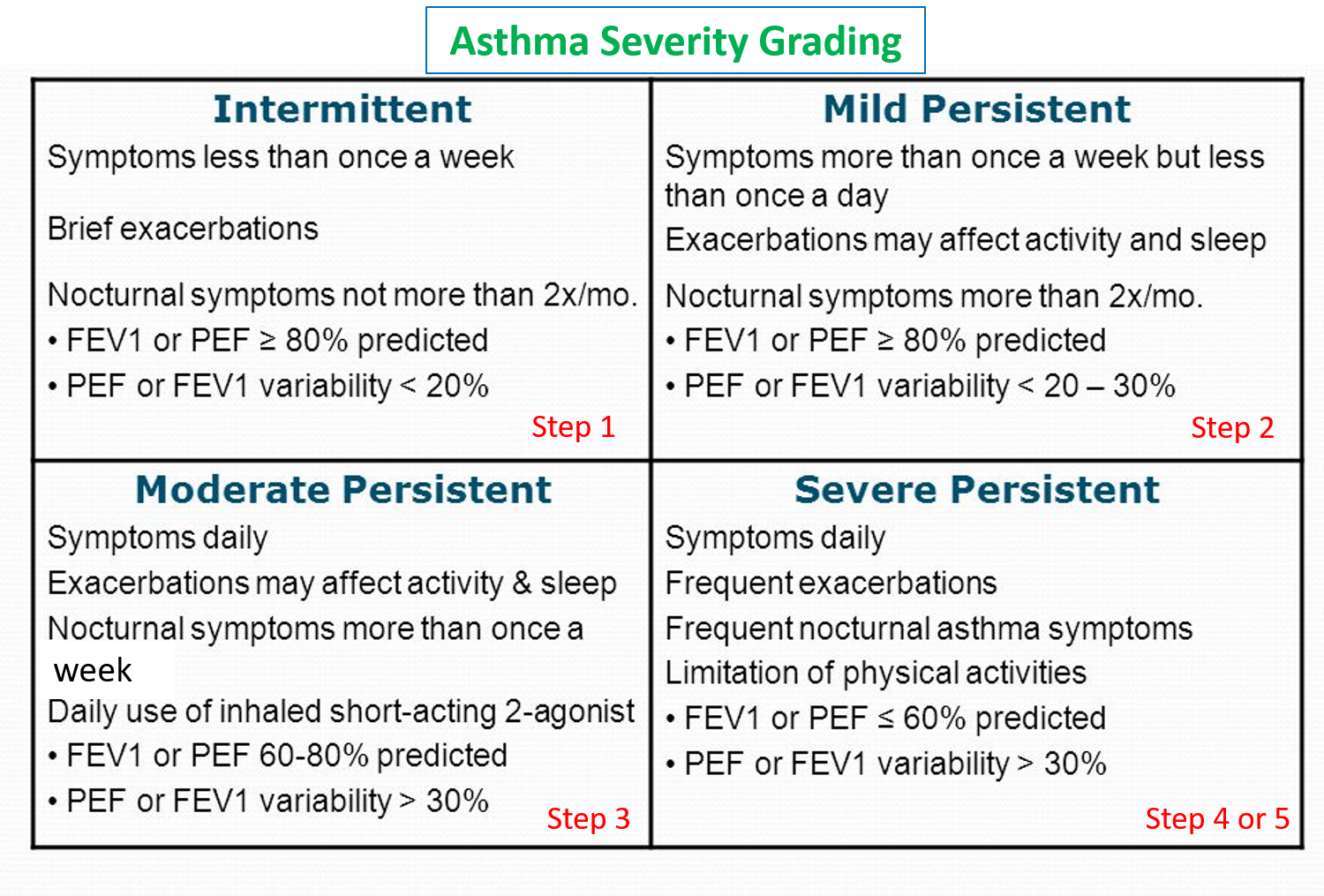
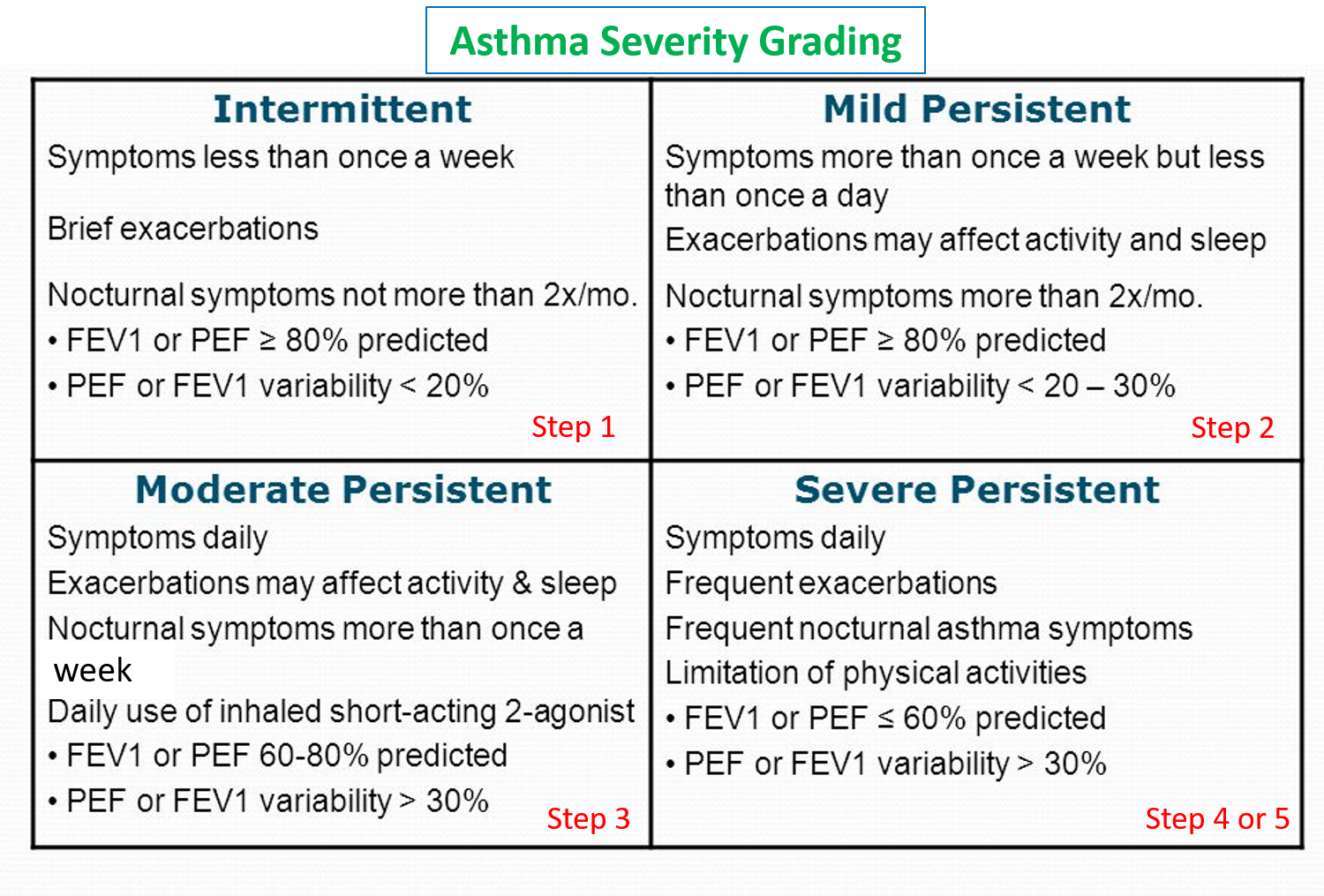
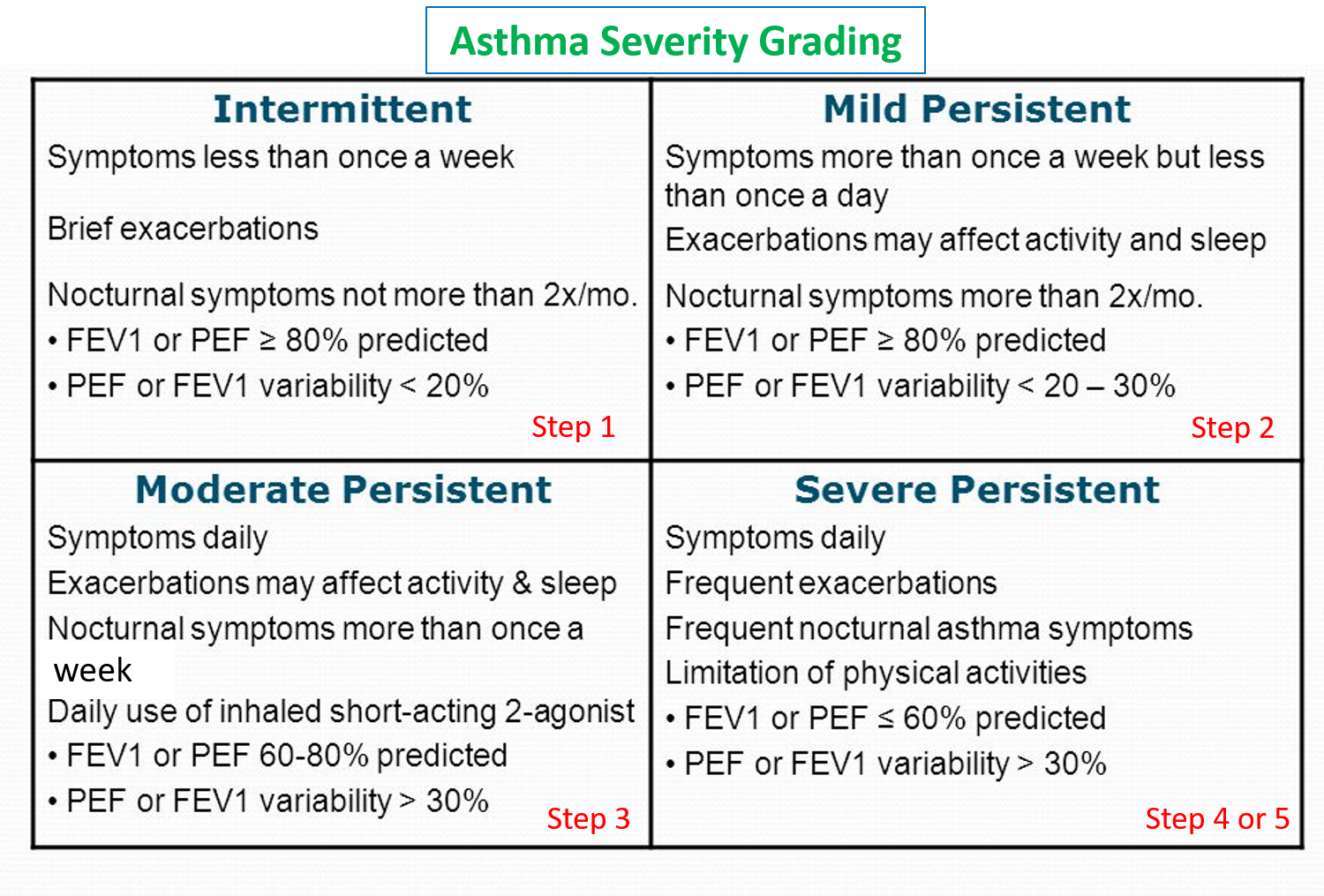
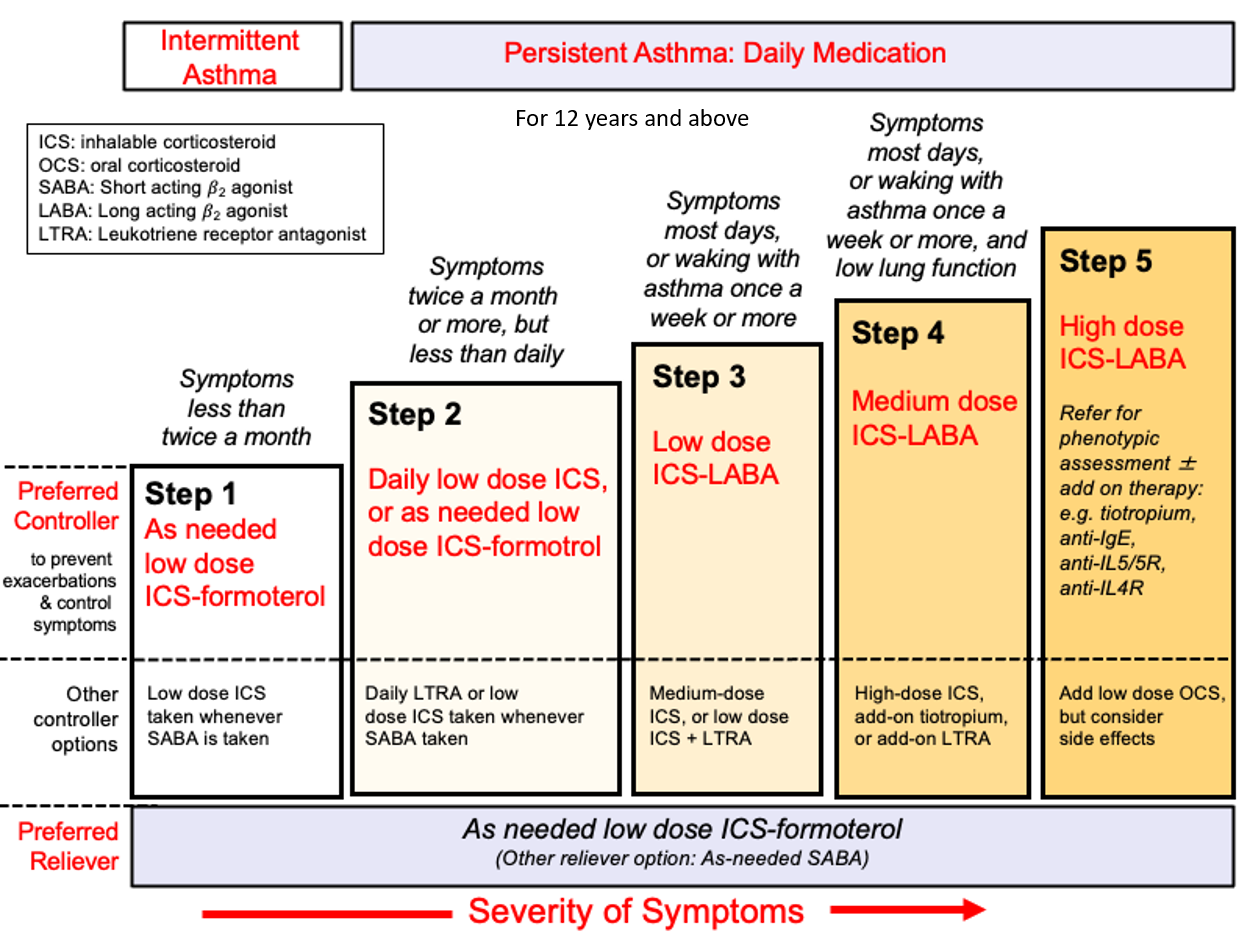
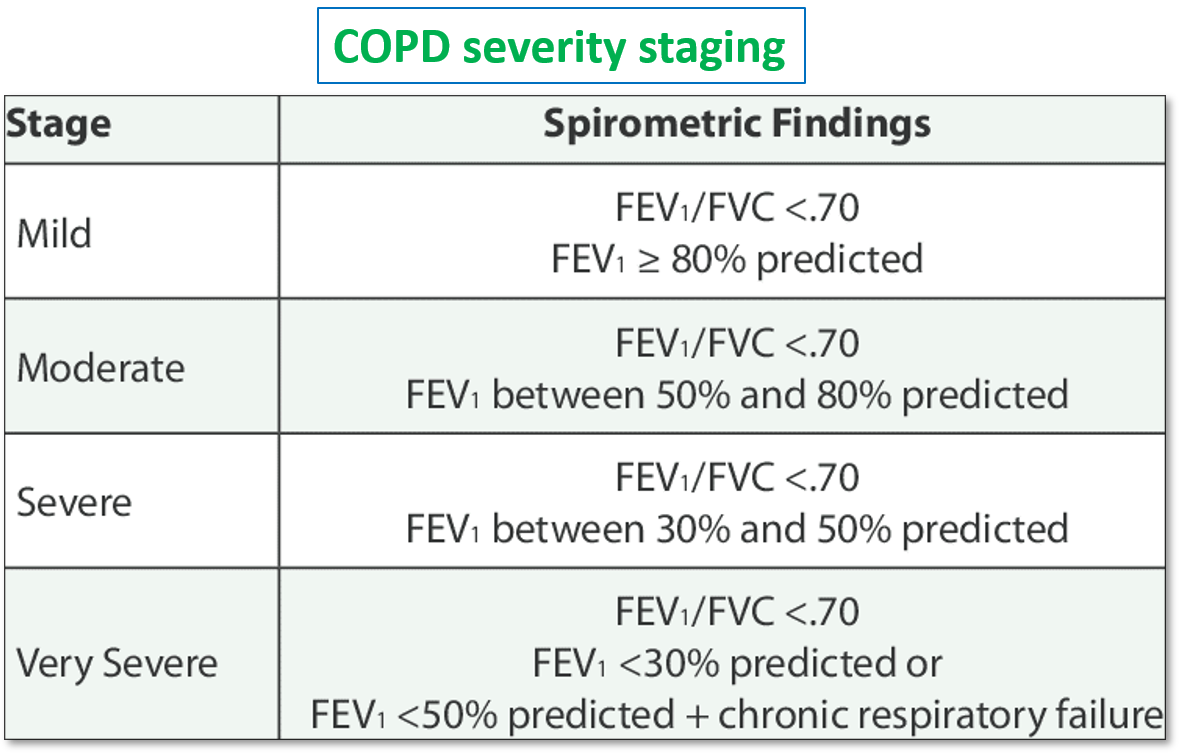
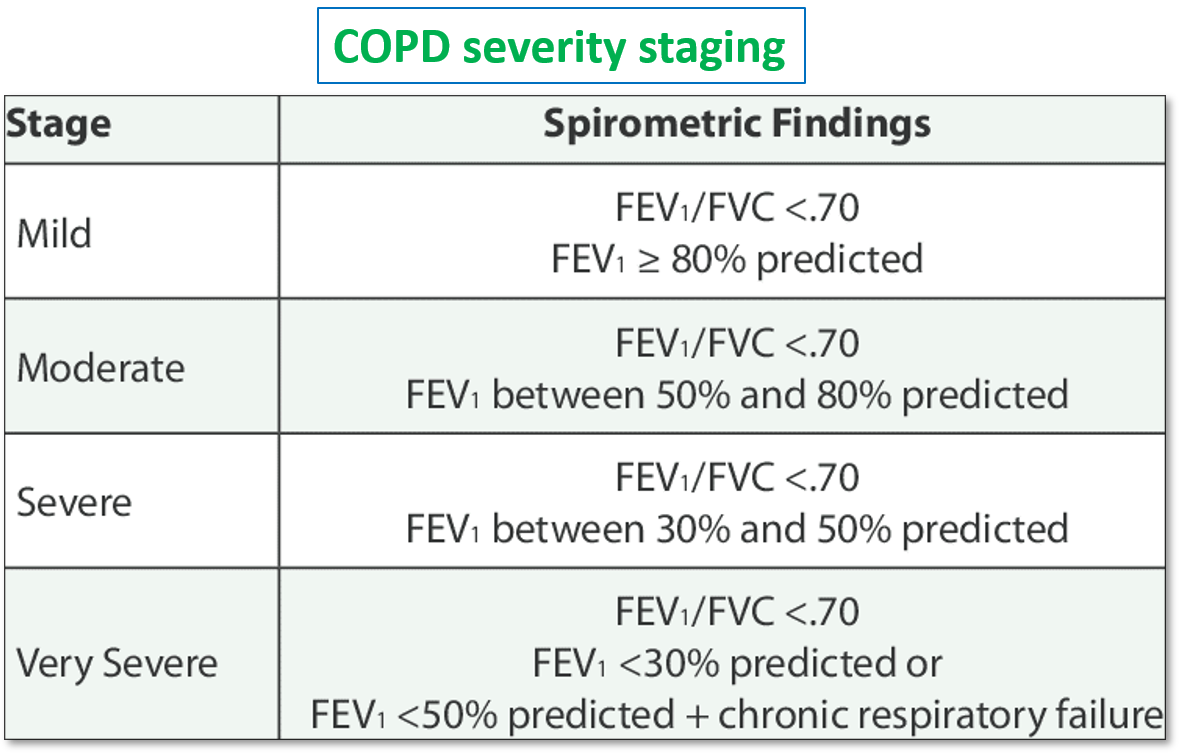
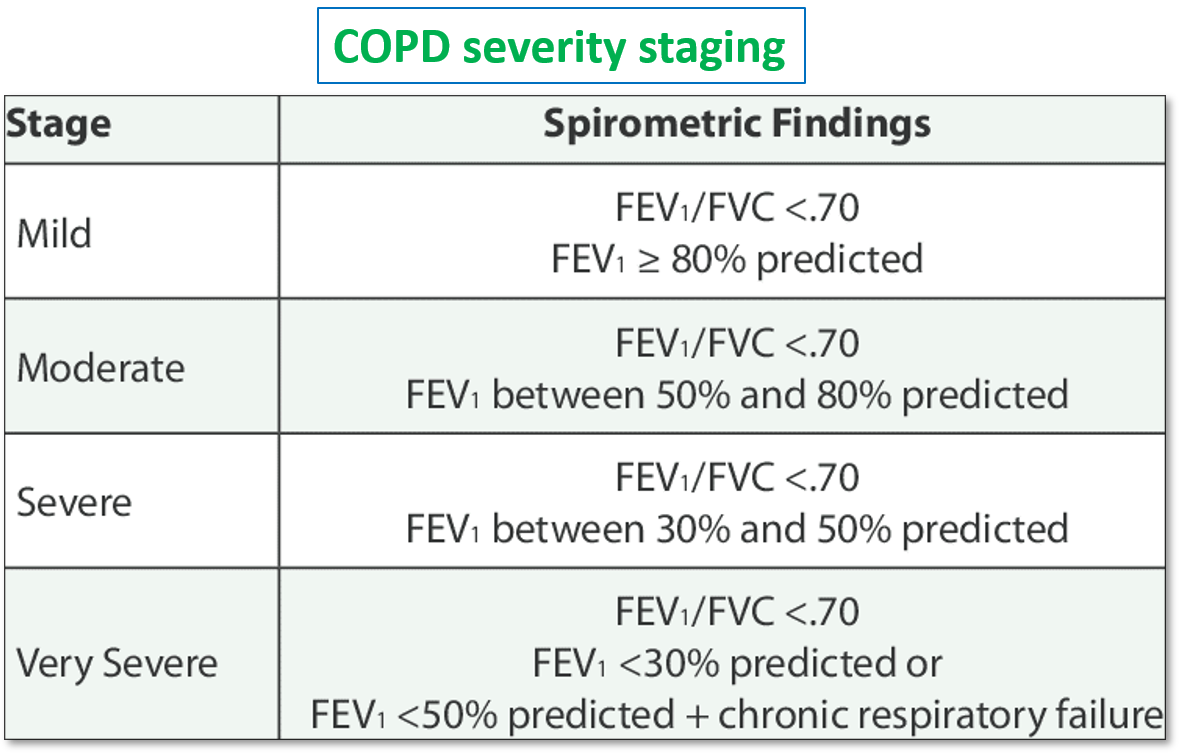
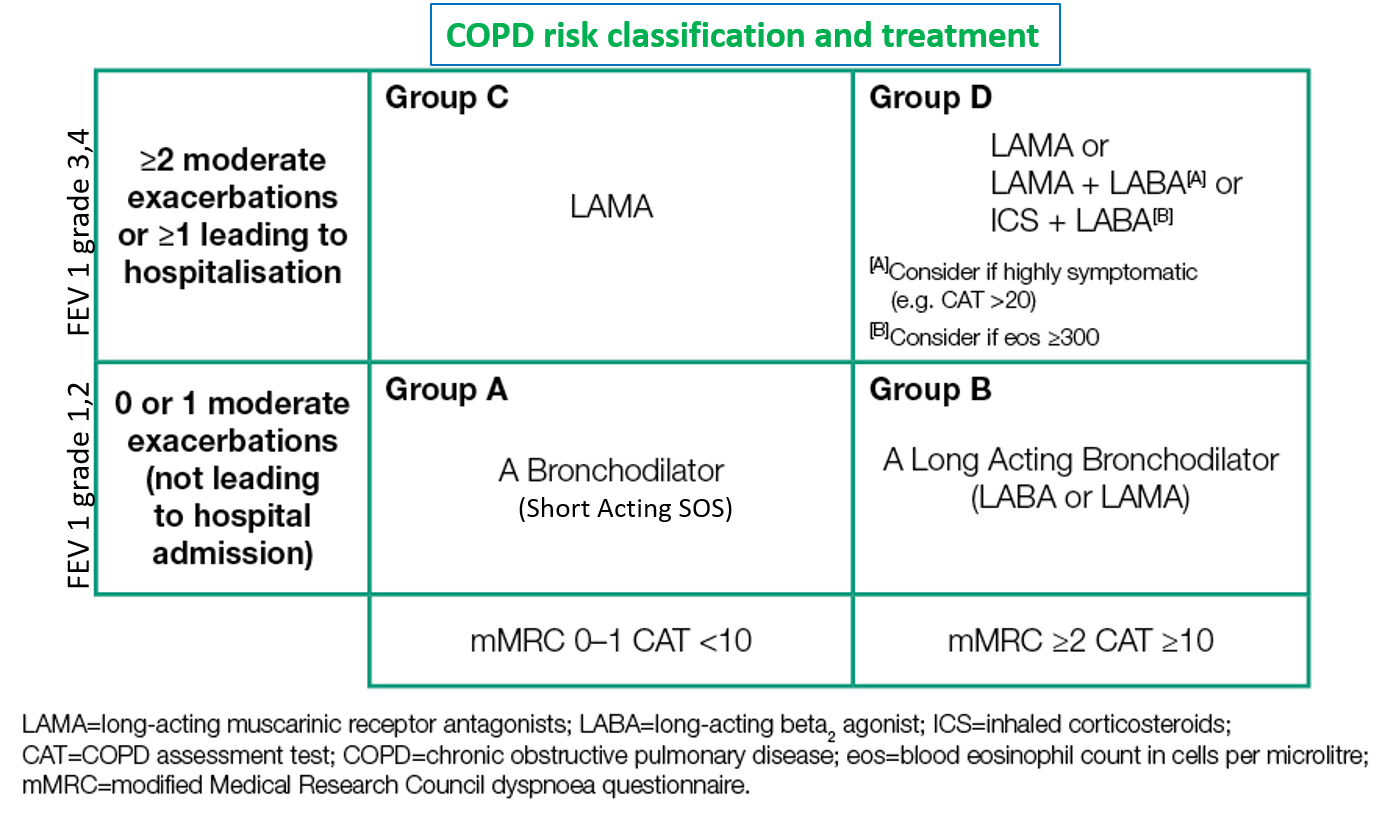
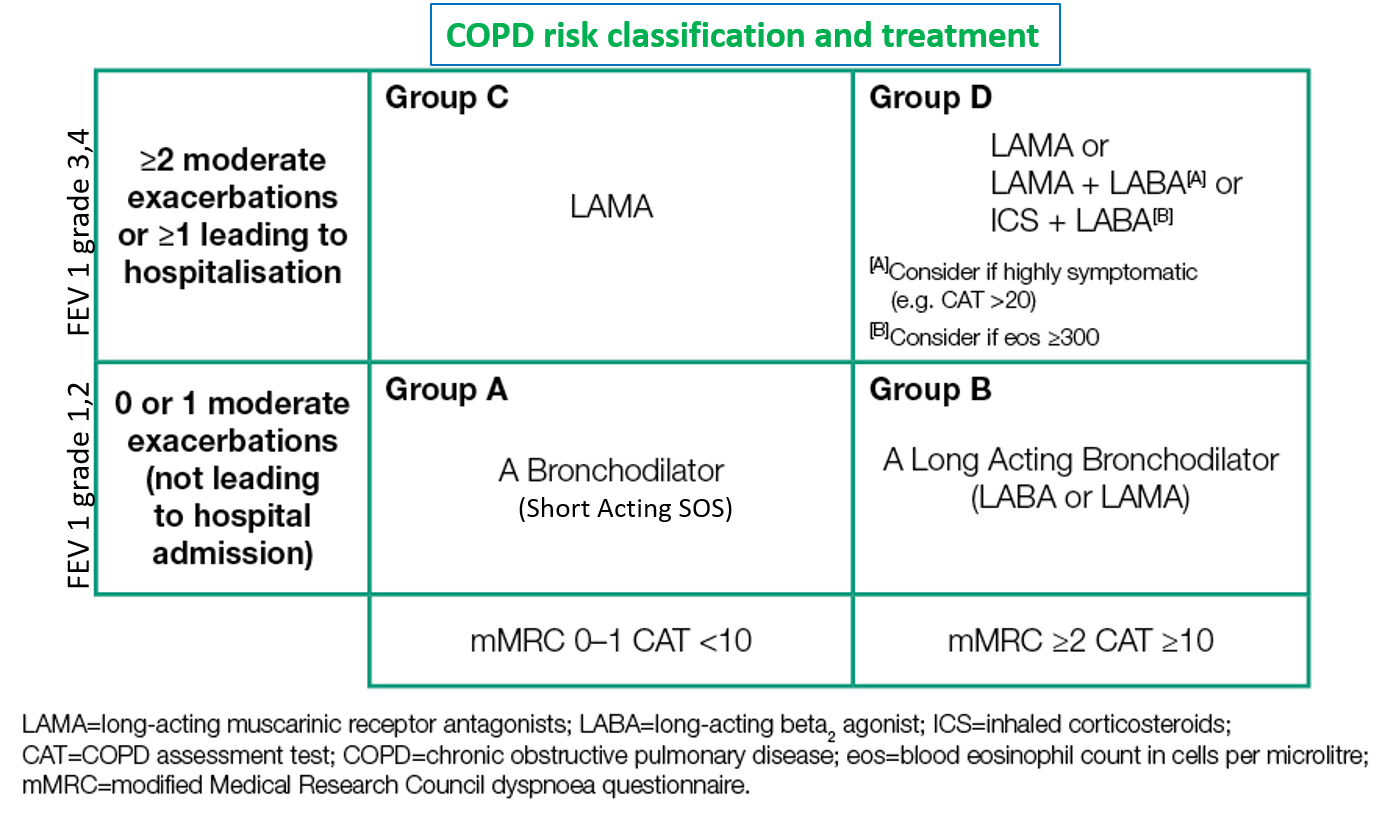
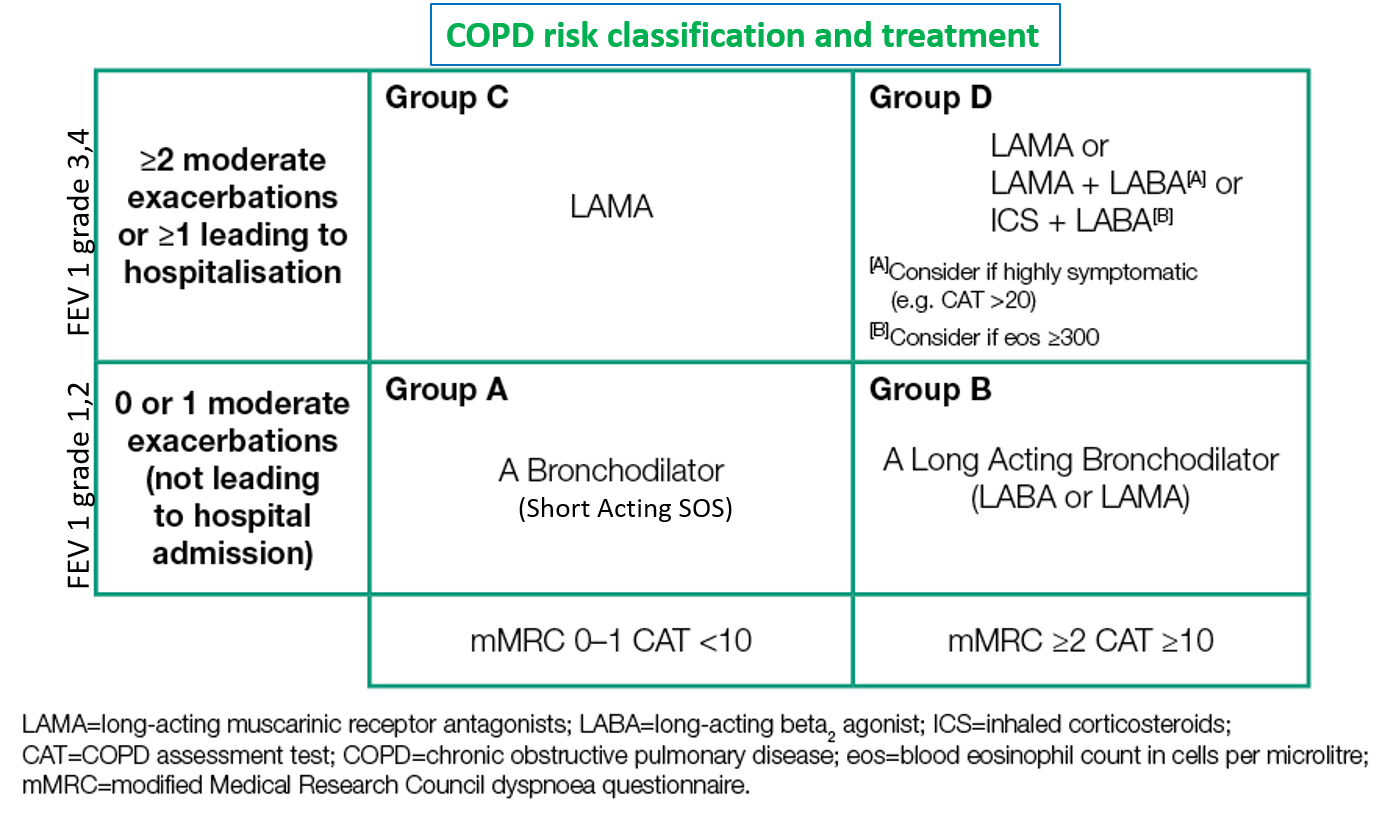
The FEV1/FVC ratio is an important value for diagnosis and grading the severity of airway disease. COPD (Chronic Obstructive Pulmonary Disease) and asthma severity are classified based on this value, along with other factors like symptom/exacerbation frequency and interference with daily life activities. The severity grading helps in deciding the appropriate treatment course. (see below for classification, severity grading, and treatment of asthma and COPD)
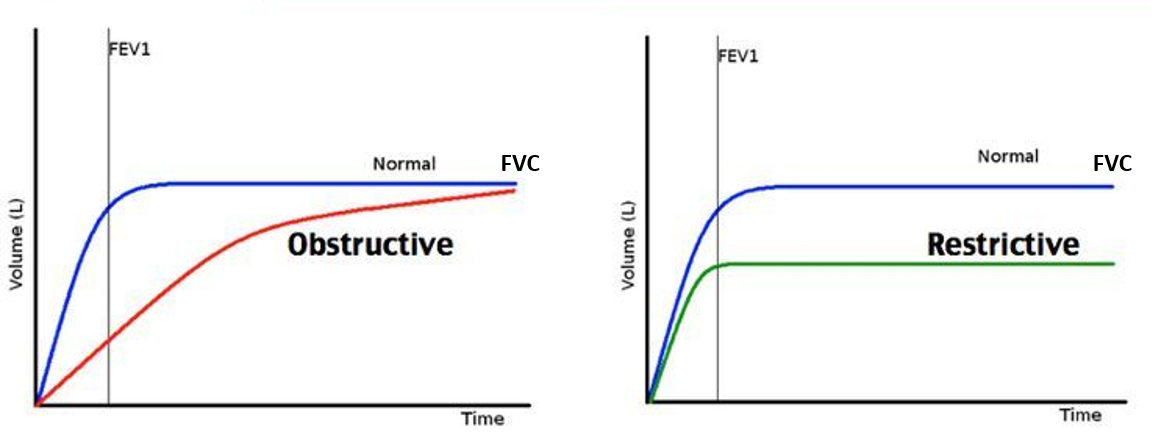
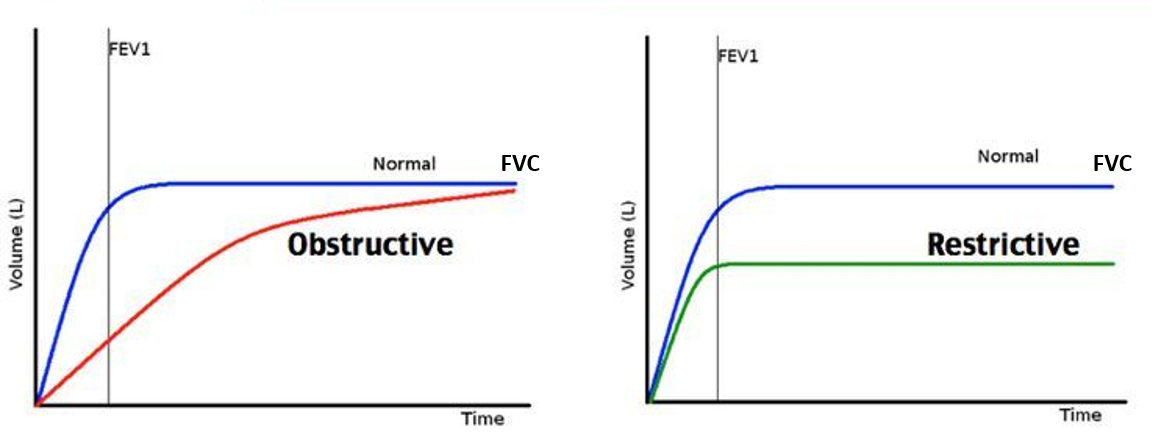
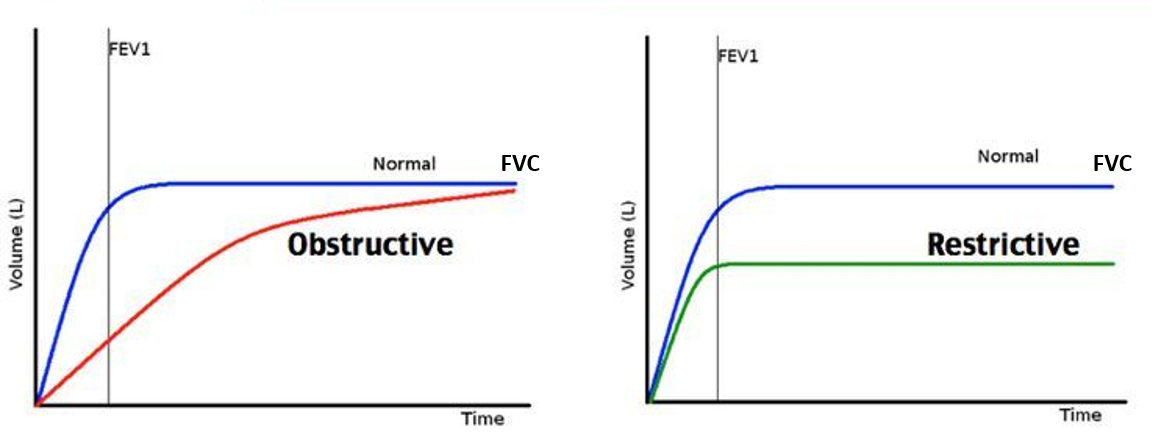
In diseases that reduce airway flow (obstructive) like asthma and COPD, the FEV1, FEF and PEFR reduce significantly, while the FVC is not affected or maybe slightly reduced in advanced disease. Therefore, a reduced FEV1/FVC ratio is the hallmark of obstructive airway diseases. In asthma, this ratio may increase after bronchodilator medication.
Whereas in restrictive lung diseases like (interstitial lung disease and pneumonia), the FVC is decreased significantly as the expansion capacity of the lung is reduced. The FEV1 and other parameters like PEFR or FEF are relatively less affected. Therefore an increased FEV1/FVC is the hallmark of restrictive lung disease. This is also seen with neuromuscular or bony (backbone/ribcage) abnormalities that restrict the expansion capacity of the chest wall and lungs.
DIFFUSING CAPACITY OF GASES
This test helps to check how much gas from the air is actually absorbed by the lungs. While lung volumes and capacity determine the expansion of the lungs, gas diffusing capacity helps to determine the ability of the lungs to absorb and transport oxygen into the blood and remove carbon dioxide.
This test is done with the help of the gas carbon monoxide (CO) that is inhaled from the spirometry mouthpiece. So, the test is also called diffusing capacity of the lung for CO (DLCO test). The difference in the amount of CO in the inhaled and exhaled air indicates how much of the gas was absorbed by the lungs.
DLCO is decreased in lung conditions like ILD, pneumonia, and advanced COPD causing emphysema (emphysematous COPD), but is not affected in asthma. In the absence of lung disease, DLCO can be low in anemia, carbon monoxide poisoning (carboxyhemoglobinemia), and in heart failure causing increased pressure in the lung (pulmonary hypertension)
INTERPRETATION ALGORITHM OF PFT
ASTHMA GRADING SEVERITY AND CLASSIFICATION
COPD GRADING SEVERITY AND CLASSIFICATION
Also read:
Interstitial Lung Disease (ILD) – Types, Risks, and Health Measures
REFERENCES

