WHAT IS ILD?
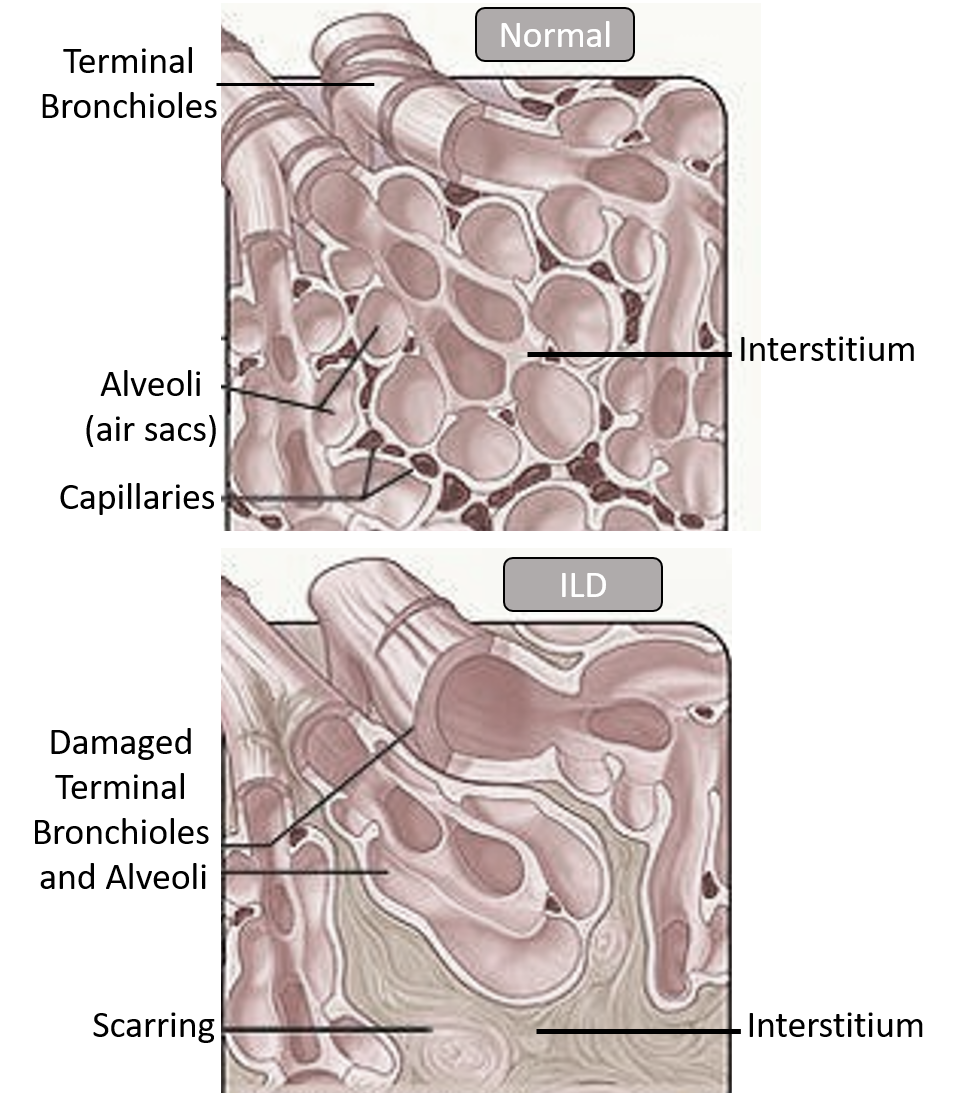
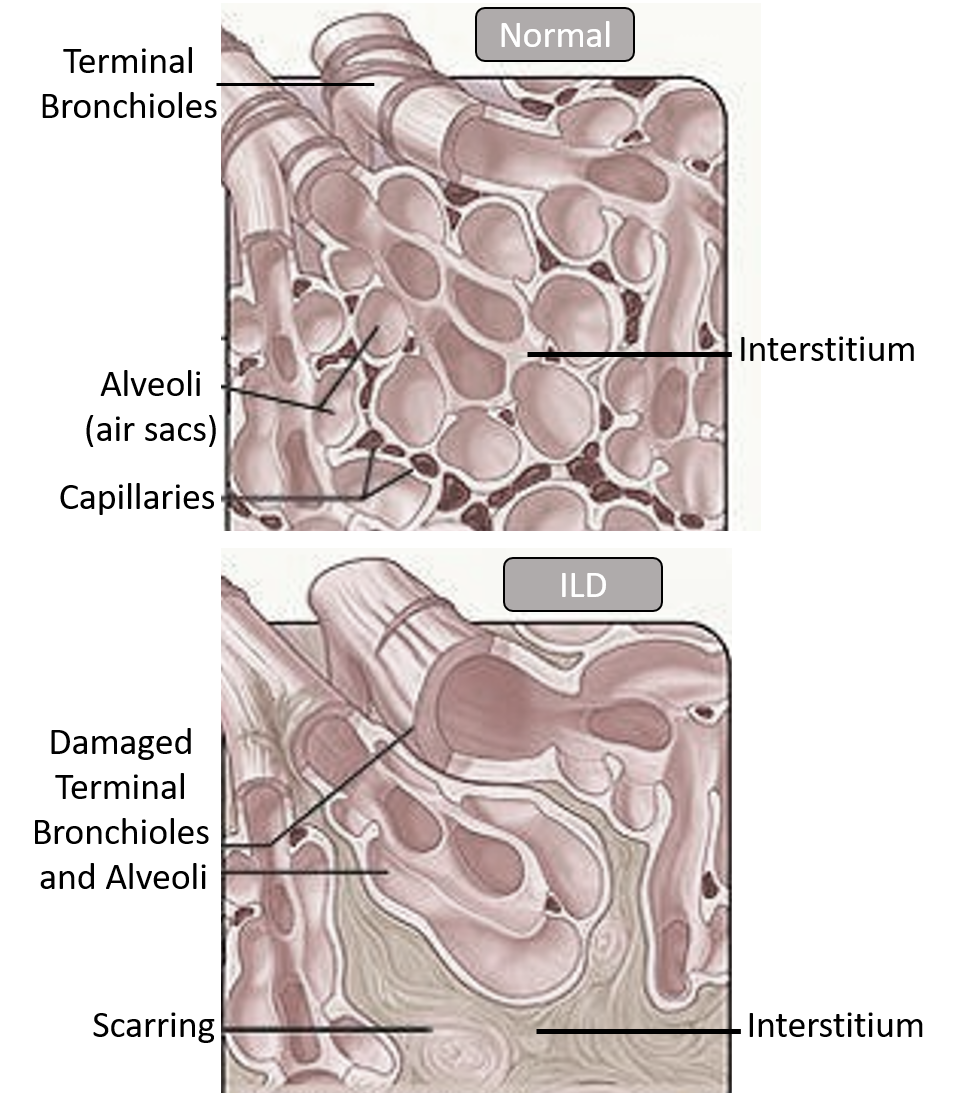
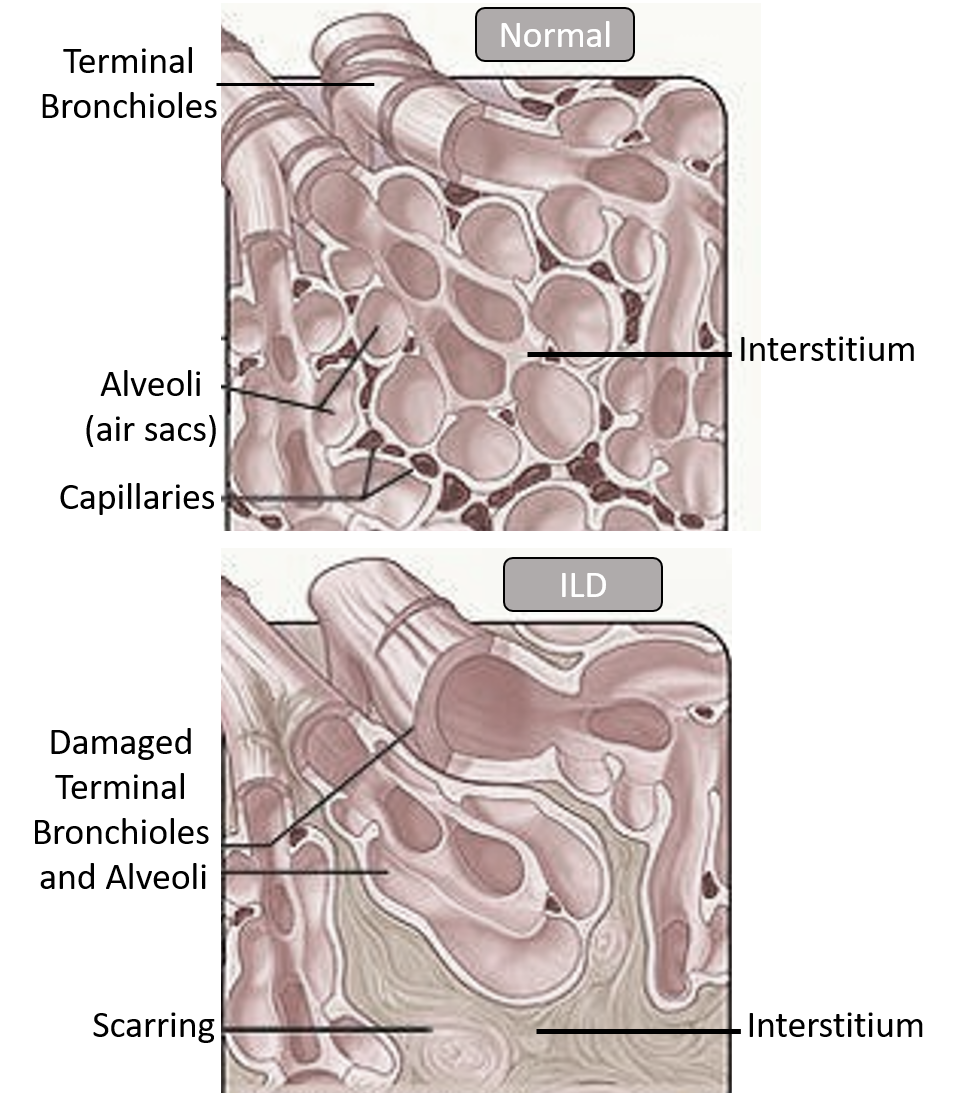
Interstitial lung disease (ILD) is a group of conditions that cause scarring (fibrosis) of the interstitial part of the lung (interstitium). The interstitium is the area in between the air sacs (alveoli – where the gaseous exchange takes place). The interstitial tissue provides support and flexibility to the air sacs so that they can expand with air permitting effective delivery of oxygen across the walls of the alveoli into the blood capillaries in exchange for carbon dioxide.
Scarring of the interstitium makes it stiff and inflexible, thereby restricting the capacity of the alveoli to expand. Progressive scarring also slowly damages the terminal bronchioles (small lower airways leading to the air sacs) as well as the walls of the alveoli, thereby decreasing gaseous exchange.
SYMPTOMS
ILD may be silent for years. The symptoms are a gradually decreasing work capacity and fatigue, increasing breathlessness progressing from after exertion to even at rest, and sometimes a dry cough. Sometimes there may be accompanying joint and muscle pains along with weight loss.
Often by the time a diagnosis is made, there is usually significant and irreversible scarring and damage. People with ILD are at risk of higher hospitalization and worse prognosis after lung infections like TB and COVID.
CAUSES AND RISK FACTORS
The exact cause and pathological processes are still elusive, but ILD seems to occur due to an abnormal and exaggerated repair and healing process that causes scarring, in response to lung injury by environmental insults and irritants over a period of time. Often there may be an abnormal immune and inflammatory response which explains the association of ILD with autoimmune diseases.
The following are risk factors for ILD as they increase lung injury or are associated with an abnormal immune response:
Occupational exposure: Long-term and regular exposure to substances that cause lung injury can occur due to working in such industries and factories. These include silica dust, asbestos fibers, steam, radiation, grain dust, cotton dust, animal/bird droppings, molds, and other substances inhaled in mining (coal dust), farming and construction sites.
Smoking: Tobacco and smoke are established agents causing lung injury. They increase the risk of a number of lung conditions like ILD, COPD, and lung cancer.
Medicines: Certain treatments like radiation and cancer chemotherapy drugs (bleomycin, methotrexate cyclophosphamide, methotrexate, azathioprine, procarbazine, mitomycin, etc.), some heart medications (amiodarone, propranolol), antiarthritic medicines (rituximab, sulfasalazine), and antibiotics (nitrofurantoin, ethambutol, sulfonamides, amphotericin B), can cause lung injury when used for prolonged periods.
Autoimmune diseases: These are a group of conditions occurring due to the body’s abnormal immune response and ‘self’ recognition of certain proteins. These conditions are associated with ILD and include rheumatoid arthritis, and other rarer ones (scleroderma, polymyositis, dermatomyositis, Sjogren’s disease, and mixed connective tissue disease). These conditions present with other symptoms therefore such patients can be monitored for the development of ILD. Other rare conditions proposed to also have an autoimmune basis are sarcoidosis (collection of immune cells forming lumps called ‘granulomas’ throughout the body), and histiocytosis (abnormal increase in immune cells called histiocytes – monocytes, macrophages and dendritic cells).
Hypersensitivity: ILD can be caused by an allergic or hypersensitivity to inhaled bacterial, fungal, and animal proteins, or chemicals (hypersensitivity pneumonitis) and sometimes abnormally high number of immune cells called eosinophils to appear (eosinophilic pneumonia) in lung and blood.
Others: These include rare conditions like fibrosis seen with inflammation of blood vessels (vasculitis), after a lung hemorrhage (diffuse alveolar hemorrhage -DAH), abnormal growth, and multiplication of muscle tissue lining the airway and lung blood vessels (LAM – lymphangioleiomyomatosis).
Age: Increasing age signals a longer duration of exposure to irritants, reduced tolerance of the lung, and hampered healing mechanisms.
Often no cause, exposure or specific risk factor apart from age is found. In such cases, the term used is ‘idiopathic’. Such conditions are grouped under idiopathic interstitial pneumonia, among which the most common is idiopathic pulmonary fibrosis. Other idiopathic varieties may be labeled in accordance with their appearance on biopsy and histopathology (non-specific, cryptogenic, acute, desquamative, lymphocytic, respiratory bronchiolitis, etc.)
COMORBIDITIES
There may be some coexisting conditions that may cause worsening of the ILD itself, needing timely detection and management. These include gastroesophageal reflux disease (GERD), sleep apnea, osteoporosis, cardiovascular disease, thrombosis, and pulmonary embolism, heart failure, and anxiety/depression.
CLINICAL COURSE AND COMPLICATIONS
ILD is usually a progressive condition, with the rate of progression varying depending on the person’s lifestyle, associated risk factors and comorbidities, and the time of diagnosis.
Complications that cause worsening and ultimately death include increased pressure in the lung blood vessels (pulmonary hypertension-PH) causing right-sided heart failure (cor pulmonale), and respiratory failure when the oxygen levels in the blood are not enough to sustain the functioning of vital organs.
DIAGNOSIS
A history and physical examination can create clinical suspicion for ILD. Breathlessness on a 6-minute walk test and timing the appearance of breathlessness helps in diagnosis of ILD and PH, and is also useful to monitor response to treatment.
Pulmonary function tests (PFT) are performed to assess the functional impairment of the lung, and establish the diagnosis of restrictive lung disease. Pulse oximetry helps to assess blood oxygen levels. Imaging by chest X-ray and CT scan can confirm the diagnosis of ILD.
Bronchoscopy involves the insertion of the tube through the airway into the lung. It is done to take a biopsy (a piece of lung tissue) and to do a bronchoalveolar lavage (BAL- where cells are suctioned out after stimulation with saline injection through the bronchoscope).
Surgical biopsy through incisions in the space in between the ribs, under anesthesia may be performed in some cases.
Blood tests are done to assess general health, and for markers of causative autoimmune or inflammatory conditions.
Echocardiography is also performed to assess the functioning of the heart and the presence of pulmonary hypertension.
TREATMENT
This involves lifestyle measures, oxygen therapy, and medicines.
Nutritious diet, along with guided physical exercises and breathing techniques are recommended.
Medicines
Drugs to reduce inflammation and suppress the abnormal or exaggerated immune response are used in treating ILD. These are corticosteroids, and other immunosuppressants like methotrexate, mycophenolate, azathioprine, etc.
Antifibrotic drugs may be useful in slowing disease progression. There are two drugs available (pirfenidone and nintedanib) that reduce pulmonary fibrosis. The newest FDA-approved drug is nerandomilast approved in October 2025, shown to slow the decline of lung function in patients with IPF.
Both anti-inflammatory immunosuppressive drugs and antifibrotic drugs have side effects, and may not be tolerated well in some people, which limits their usefulness. Sometimes intravenous immunoglobulins have been tried.
Biologicals (monoclonal antibodies MAbs) are being evaluated for ILD associated with autoimmune conditions. Tocilizumab has been approved for slowing the rate of decline in pulmonary function in adults with systemic sclerosis-associated interstitial lung disease (SSc-ILD).
Antioxidant supplements may also be advised to slow down inflammation and improve general health.
Acid suppressants are prescribed to manage associated acid reflux disease.
Pulmonary hypertension (PH) is a complication of severe and long-standing ILD, that can worsen symptoms and increase the risk of heart failure. Not all the medicines used to treat PH are effective in ILD-PH. The prostacyclin group of drugs (inhaled/infusion) have shown beneficial effects of improving exercise capacity, breathlessness, heart function, and quality of life. Recently an inhalational form of treprostinil was given FDA approval to specifically treat ILD-PH. If heart failure is evident, then diuretics may be added.
Oxygen therapy can be given with the help of home oxygen concentrators or cylinders. Oxygen therapy does not reduce lung damage or disease progression but helps to improve blood oxygen levels, improve work capacity and sleep, and reduce/delay
Lung transplantation becomes imperative for severe progressive disease.
Palliative and supportive care are advised in patients with poor general health and significant comorbidities that rule out surgery.
Also read:
Tuberculosis (TB): Awareness, Diagnosis, Treatment, and Prevention
For any query, additional information or to discuss any case, write to info@drvarsha.com, or leave a message in box below, and be assured of a response soon
REFERENCES


