Hepatitis is the inflammation of the liver (hepa-liver; itis-inflammation). Inflammation is the response and damage caused in the body due to any injurious agent.
For the liver, the injuring agent can be infectious organisms like bacteria, viruses, parasites, and fungi, or noxious substances like alcohol, tobacco, certain medicines/drugs, and toxins. Sometimes too much deposition of some dietary components like fats, or even iron and copper can cause long-term injury to the liver. Injury can also be caused when there is a lack of blood (oxygen) supply, or rarely when the body’s own immune system mistakenly attacks the liver (autoimmune disorder).
Inflammation can occur over a short period of time (acute hepatitis) or over a long period of time (chronic hepatitis) causing long-term liver damage and loss of function.
CAUSES
- Infections: Caused most commonly due to Hepatitis virus types A,B,C,D,E
- A and E spread by contaminated water/food. Hepatitis A is more common in children, but can rarely affect adults also in whom it causes more severe disease. Hepatitis E affects young adults and can lead to complications including death in pregnant women.
- B and C spread through blood contact by infected needles, blood transfusion, sexual contact, and mother to child at birth). Hepatitis D virus only causes co-infection with B virus.
-
- Other infections: parasitic (malaria, leishmaniasis-kala azar, toxoplasmosis), bacterial (typhoid, TB, liver abscess), other (non-hepatotropic) viral infections (like yellow fever, dengue, chikungunya, CMV, HSV and EBV) and rarely fungal infections can also cause hepatitis
- Alcoholic liver disease (ALD): It is caused by the consumption of high quantities of alcohol over many years. This leads to chronic liver inflammation progressing to scarring (fibrosis) and ultimately cirrhosis.
- Metabolic associated fatty liver disease (MAFLD) or Metabolic dysfunction- associated steatotic liver disease (MASLD): This starts with the deposition of fat in the liver (fatty liver – steatosis) that over time causes inflammation and fibrosis (scarring). It is seen more in people with risk factors like diabetes, obesity, high BMI, gastric bypass surgery, high fats (blood cholesterol and triglycerides), or family history of MAFLD. Around 5-10% progress from the stage of fat deposition (fatty liver – steatosis) without inflammation, to the stage of inflammatory damage (steatohepatitis), with some of them progressing to fibrosis and cirrhosis. MASLD or MAFLD, formerly known as NAFLD (Nonalcoholic Fatty Liver Disease), is a broad term encompassing both simple fatty liver (steatosis) and a more severe form called MASH (Metabolic Dysfunction-Associated Steatohepatitis), which involves inflammation and potential liver damage
- Drugs, Metals, and Toxins – This includes liver damage caused by certain medicines (DILI: drug-induced liver injury) and other toxic substances. Genetically inherited conditions called hemochromatosis (iron accumulation) and Wilson’s disease (copper accumulation), if not treated and controlled meticulously, can cause damage to various organs including the liver, leading to inflammation and cirrhosis over a period of time.
- Autoimmune hepatitis: It is caused due to attack by the body’s own immune system.
- Ischemic (hypoxic) hepatitis: It occurs because of interruption or lack of adequate blood supply leading to oxygen deprivation. This can occur due to an injury, shock, sepsis, heart failure, or obstruction by a blood clot (thrombosis).
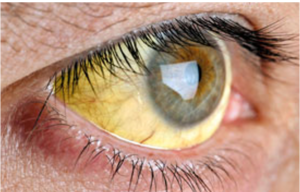
- Cholestatic Liver Disease: Cholestasis is the reduced flow of bile and can be caused by a liver infection, gallstones, cancer, and certain drugs. Stasis (congestion and accumulation of bile) leads to liver inflammation with symptoms like intense itching, dark urine, yellowing of eyes and skin (jaundice), nausea, lack of appetite, and light-color stools. Primary biliary cholangitis is a chronic inflammatory, autoimmune disease that is characterized by cholestasis, inflammation, and elevation of liver enzymes. Primary sclerosing cholangitis is characterized by progressive extrahepatic and intrahepatic bile duct fibrosis, cholestasis, and persistent inflammation and obstruction of the bile flow system due to scarring and strictures.
TYPES
Acute Hepatitis
Duration: Usually lasts a few weeks (<6 months).
Symptoms: Fever, body ache, nausea, jaundice (yellowing of the white of the eye, and skin), dark urine, pain in the upper right part of the abdomen, loss of appetite
Common causes – Viral (Hepatitis A and E), other infections of the liver, bile stasis, drugs/toxins, ischemia (lack of oxygen/blood supply).
Recovery in acute viral cases is usually spontaneous though rarely it can cause complications like liver failure (seen more in adults); Hepatitis E can especially be serious and even fatal in pregnant women.
Chronic Hepatitis
Duration: Persists for > 6 months
Symptoms: Initially weight loss, weakness, body aches, and decreased appetite. Often there are no specific symptoms, and diagnosis is made on routine lab tests.
Common causes – Viral (Hepatitis B, C, D), long-standing alcohol abuse (ALD), Non-alcoholic steatohepatitis (NASH), autoimmune hepatitis, cholestatic liver disease (CLD), and certain medicines/toxins.
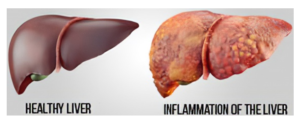
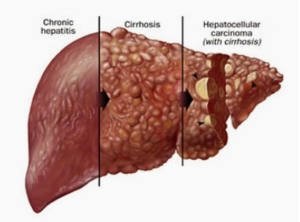
Cirrhosis
Chronic liver inflammation leads to scarring (fibrosis) of the liver. When the fibrosis leads to the loss of the recognizable normal structure of the liver due to being replaced by scar tissue thereby compromising liver function, it is called cirrhosis.
The most common causes of cirrhosis are chronic viral hepatitis (B, C), alcoholic liver disease (ALD), MAFLD (metabolic associated fatty liver disease), and chronic exposure to harmful agents/drugs/toxins.
Chronic hepatitis and cirrhosis also increase the risk of developing liver cancer (hepatocellular carcinoma)
MANAGEMENT OF HEPATITIS
Vaccines
Preventive vaccines are now available for viral hepatitis A and B and are regularly given to children as part of the immunization schedule. Adults prone to needle injuries like doctors and lab workers should be given the hepatitis B vaccine.
A vaccine for hepatitis E is available in China and is likely to soon be available in other countries. Vaccine for hepatitis C is still in the research stages.
Diagnosis
There are specific antigen and IgM/IgG antibody tests available for hepatitis viruses that help establish the causative virus, and also the stage of the disease. There are also blood tests available for malaria, typhoid, and other infections causing hepatitis.
Liver function tests (LFT) are blood tests that help to assess the amount of liver inflammation and the functioning of the liver, and also help to monitor disease progression/improvement. These include liver enzymes (SGOT or AST, SGPT, or ALT, and ALP, GGT, the latter 2 being especially increased in CLD), bilirubin, proteins (albumin and globulin), and prothrombin time (PT-INR).
Blood tests including those for fasting and postprandial sugar, complete blood counts including platelets, lipid profile, thyroid, and renal function, may also be performed.
Based on tests, risk scores are also assessed. For example, MAFLD risk score based on age, BMI, impaired fasting glucose, albumin, AST-ALT, and platelet count is an indirect marker for the amount of liver damage and fibrosis.
Fibroscan
Fatty liver (steatosis), inflammation due to fatty deposition (steatohepatitis), and fibrosis/cirrhosis is usually diagnosed by an ultrasound test called FibroScan, and it is confirmed and staged by performing a liver biopsy. Since there are usually no specific symptoms in the early stages of chronic hepatitis, people with the mentioned risk factors for MAFLD, and alcohol history, should be screened by FibroScan.
The FibroScan measures 2 parameters:
- LSM: liver stiffness by transient elastography measurement (indicates and grades the amount of fibrosis- measured in kPa). Normal values for liver stiffness range from 2-7 kPa, while in cirrhosis it can go to 15 or more up to a maximum of 75kPa.


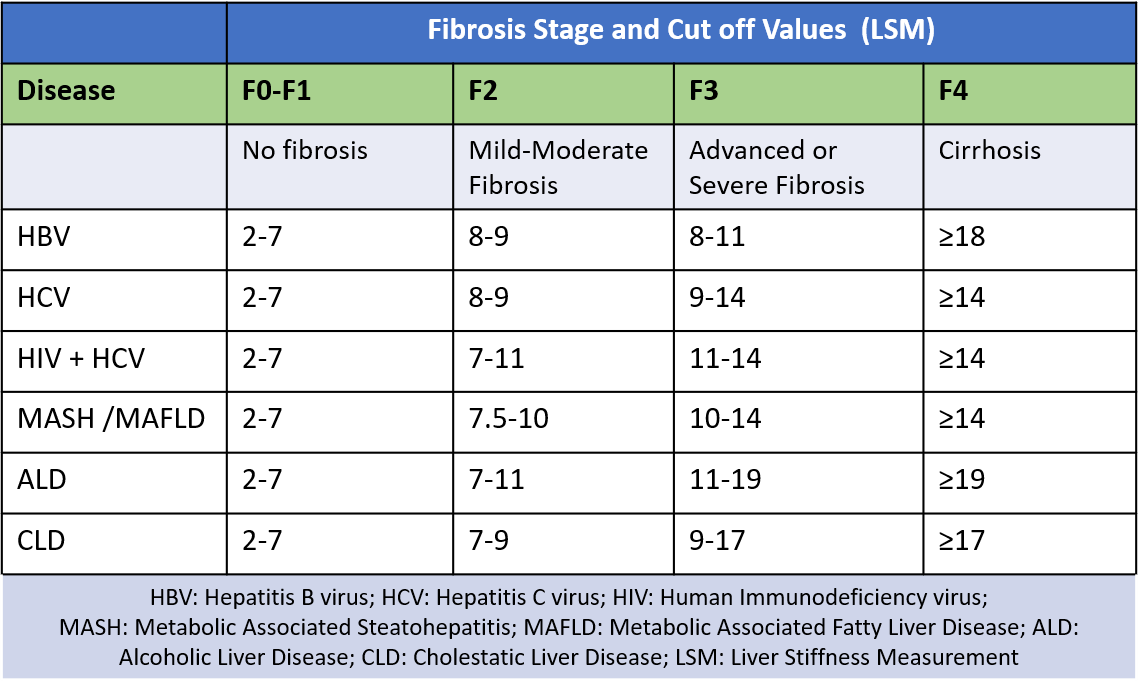
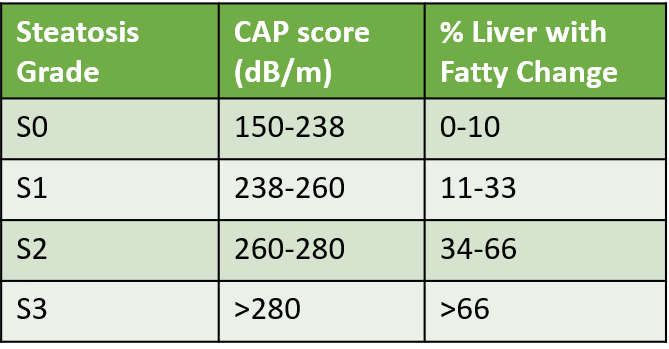
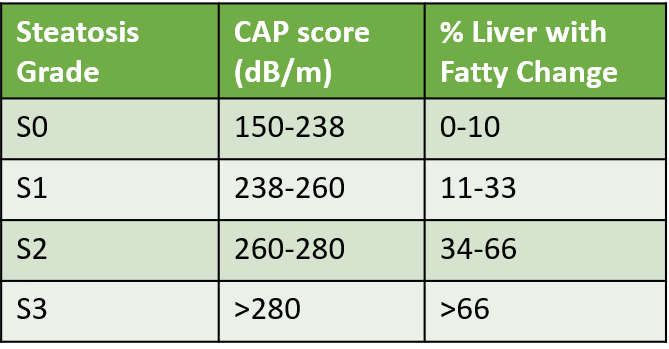
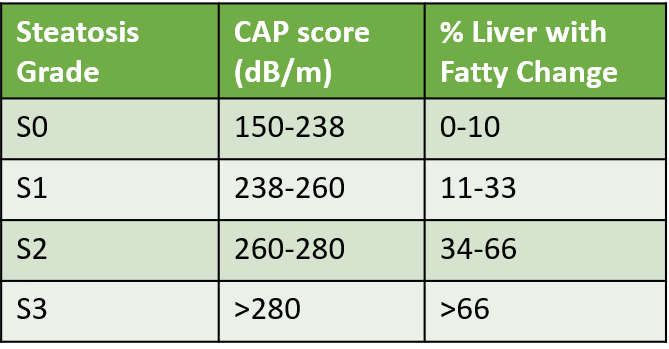
- CAP: controlled attenuation parameter (indicates and grades the amount of fat deposited in the liver – measured in dB/m) and CAP score grading is based on the amount (%) of liver involved.
APRI
The APRI score estimates the amount of fibrosis in the liver by dividing the AST level by the upper limit of normal for AST, then dividing that result by the platelet count. An APRI score above a certain threshold (0.7) suggests significant fibrosis. A higher APRI score generally indicates more severe fibrosis. APRI is used as a screening tool to identify individuals who may need further evaluation for liver fibrosis, particularly those with chronic liver diseases like hepatitis C or non-alcoholic fatty liver disease.
Fib4
The FIB-4 index is a simple non-invasive approach using selected laboratory measures (AST, ALT, platelet count PLT) in combination with patient age to assess if an individual is at higher risk for advanced liver fibrosis (F3-F4). 4
The formula for FIB-4 is: Age ([yr] x AST [U/L]) / ((PLT [109/L]) x (ALT [U/L])(1/2)).
Treatment
Acute hepatitis (mainly due to HVA and HVE common with water and food contamination), is managed with rest, adequate fluids, dietary fat and alcohol restriction, and no drugs/medicines. It usually shows a full recovery in 3-4 weeks. Rarely it may present as a severe form spiraling quickly into liver failure. Adults especially the migrating population, and pregnant women are most at risk for complications and fatality due to hepatitis A and E.
Chronic hepatitis if due to HVB or HVC is managed with medicines now available (tenofovir and entecavir for hepatitis B, and sofosbuvir, ledipasvir, daclatasvir and velpatasvir for hepatitis C). Usually, treatment continues for several months with regular monitoring and lab tests in order to effectively control the infection and prevent the development of cirrhosis. Even after long-term treatment and recovery, monitoring continues for life as the increased risk of developing liver cancer remains.
Autoimmune hepatitis is managed with immunosuppressive medicines. For DILI treatment rests on recognition of the disorder and stopping of the incriminating drug along with supportive care. Specific antidotes like N- Acetylcysteine (NAC) in Paracetamol poisoning exist in a few settings
ALD and MAFLD currently have no specific medicines, though supportive therapy with tonics, nutritional supplements, and antioxidants is often prescribed. Research on specific drugs is in progress. Saroglitazar has recently been approved in India as a specific drug for NASH. Resmetirom a drug that helps to reduce fat production, increase the breakdown of fatty acids, and decrease liver fat content, was approved by FDA in March 2024 for MASH and liver scarring due to steatosis. Antidiabetic drugs and vitamin E are also used in managing various stages of MAFLD. Treatment and management of underlying risk factors is the cornerstone.
Cholestatic liver disease is treated by firstly addressing the cause, like changing medicines, treating infection with appropriate antibiotics or antivirals, and using procedures like endoscopy (ERCP. – Endoscopic retrograde cholangiopancreatography) to remove blockages and bile duct stones, and open up narrowed passages with stents. In chronic cases, lifestyle-diet changes with medicines like ursodeoxycholic acid (UDCA) and cholestyramine which help relieve bile stasis, are used.
Once cirrhosis is advanced, liver transplant should be considered.
For any query, additional information or to discuss any case, write to info@drvarsha.com, and be assured of a response soon.
References
Also read-
Fatty Liver – 5 Important Points of Awareness and Understanding
Water-Borne Diseases, Contaminated Food and Gastrointestinal Infections