Currently, conventional cancer treatment includes surgery, chemotherapy and radiotherapy and these are the cornerstones and most widely recommended in modern medicine.
CONVENTIONAL THERAPIES
Surgical removal of the entire cancer and some normal surrounding area for good margin, is the ideal cancer treatment for the best chance of cure, and minimizing recurrence risk. Surgery is an option only with timely diagnosis and is not possible if the cancer has spread through the blood to various other organs (metastasis).
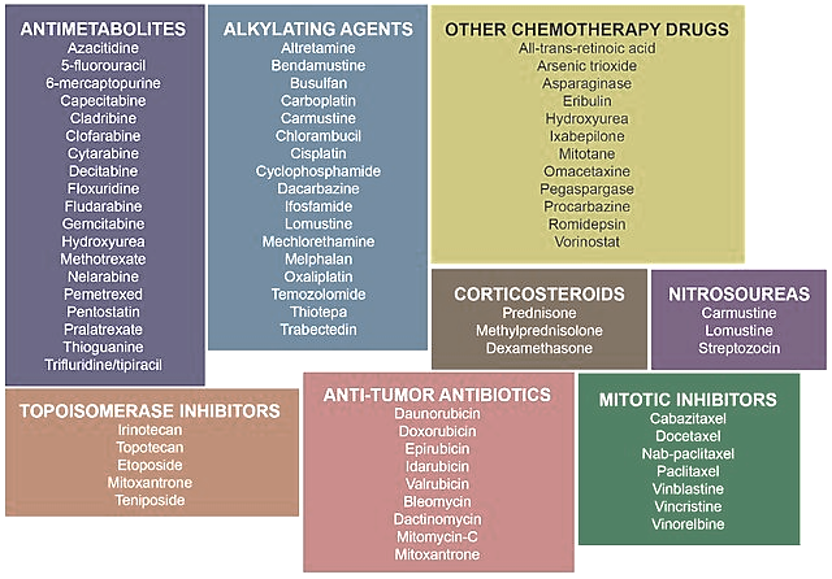
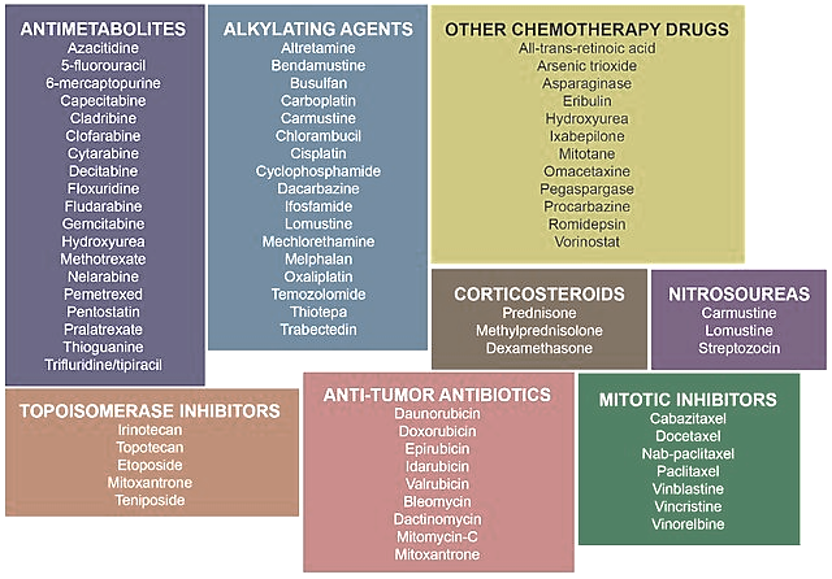
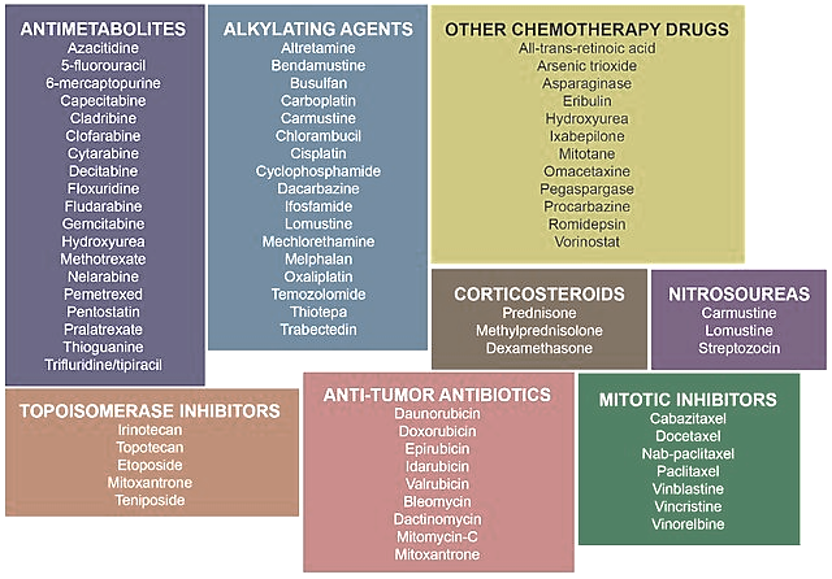
Chemotherapy (anti-cancer drugs) and radiotherapy are also used to kill cancer cells. Newer, more effective, and specific chemotherapy drugs are increasingly available for many cancers, while radiotherapy techniques have been continually refined. However, side effects like hair loss, gut intolerance (nausea, vomiting, bowel changes), and increased susceptibility to infections due to the immune-suppressive effects, are always concerning.
TARGETED THERAPY
Monoclonal antibodies: These are large biological immune system proteins created in the lab and available as injections. They bind to specific targets on cancer cells. MAbs work by directly killing cancer cells, by attaching to cancer cells and marking them, signaling the immune system to destroy them, or by blocking proteins on cancer cells that are necessary for their growth and spread. Another type of MAb, called an antibody-drug conjugate, carries a toxic drug directly to the cancer cells. Examples of mAbs and their targets/uses include:
- Trastuzumab and Pertuzumab: Targets HER2, used for HER2+ breast cancer and stomach cancer.
- Rituximab and Ibritumomab target CD20, and Alemtuzumab targets CD52, used for non-Hodgkin lymphoma and chronic lymphocytic leukemia.
- Bevacizumab (Avastin): Blocks vascular endothelial growth factor (VEGF) to stop tumor blood vessel growth, used for various cancers.
- Cetuximab and Panitumomab: Targets the epidermal growth factor receptor (EGFR), used for head and neck cancer and colorectal cancer.
- Ipilimumab: Targets CTLA4 and is used for melanoma.
- Daratumumab: Used to treat multiple myeloma by targeting CD38 proteins on the surface of cancer cells
- Brentuximab vedotin: Targets CD30, used for Hodgkin’s lymphoma and anaplastic large cell lymphoma.
Antibody-Drug Conjugates: These drugs combine an antibody that targets a specific cancer marker with a chemotherapy drug. Examples include ado-trastuzumab emtansine for HER2+ metastatic breast cancer.
Ciclibs drugs: These are small molecules that enter cells to target and inhibit cyclin-dependent kinases (CDK4/6 inhibitors), thereby halting cancer cell growth by interfering with the cell cycle. While MAbs are large, extracellular, and immune-focused, ciclibs are small, intracellular, and cell-cycle focused. The Ciclibs (Palbociclib, Ribociclib, and Abemaciclib) are used to treat HR+ (hormone-receptor-positive) and HER2- (human epidermal growth factor receptor 2 negative), advanced or metastatic breast cancer.
PARP inhibitors: These are a type of targeted cancer therapy that works by blocking the PARP enzyme, which is crucial for repairing single-stranded DNA breaks in cells, so these drugs are particularly effective against cancers with mutations that impair DNA repair (such as BRCA gene mutations in breast cancer, where the cancer cells become dependent on PARP for survival). By preventing DNA repair, PARP inhibitors (olaparib, niraparib, rucaparib, and talazoparib) cause cancer cells to die through a process called synthetic lethality, and they are approved to treat ovarian, breast, prostate, and gynecologic cancers.
Hormonal therapy: This involves the use of agents that block hormones that fuel hormone-sensitive cancers, like certain breast cancers (hormone receptor positive -HR+) and prostate cancers. This treatment can be given before or after surgery or radiation to shrink tumors or prevent recurrence. It is most commonly used for estrogen (ER+) and/or progesterone receptor (PR+) positive breast cancers and some prostate cancers. The medicines include anti-estrogen drugs (selective estrogen receptor modulators – SERMs – tamoxifen, fulvestrant that block estrogen receptors on breast cancer cells), aromatase inhibitors (letrozole, anastrozole that block estrogen synthesis), and androgen deprivation therapy (ADT – for prostate cancer that lowers androgen levels – like GnRH agonists and anti-androgen agents bicalutamide, flutamide, and nilutamide).
Some cancers may not be amenable to targeted therapy and therefore require conventional therapy, like the aggressive triple-negative breast cancer (TNBC), where the cancer cells lack estrogen receptors, progesterone receptors, and HER2 protein.
Immunotherapy is a futuristic way of cancer treatment that involves modifying or empowering the immune system in various ways to fight and destroy cancer cells. Such treatments are also called targeted therapy. Here are some of the new treatments of cancer that are being tried and researched, and can be promising for the future:
- PD1 immunotherapy – Some monoclonal antibodies (MAbs) mark cancer cells so that they will be better seen and destroyed by the body’s immune system. PD-1 (programmed cell death protein 1) on immune cells is used by cancer cells to “hide” from the immune system. Drugs called immune checkpoint inhibitors (pembrolizumab, atezolizumab, durvalumab, and nivolumab) are PD-1 inhibitors, enabling immune cells to recognize and destroy cancer cells more effectively.
- CAR T-cell therapy: It consists of taking specific T lymphocyte cells (type of white blood cell) from the patient and in the laboratory, adding to it the gene for a special receptor that binds to a certain specific cancer antigen (protein) which is not present on normal body cells. The special receptor is called a chimeric antigen receptor (CAR). Large numbers of the CAR T cells are grown in the laboratory and then injected into the patient. CAR T-cell therapy is used to treat certain blood cancers, and it is being studied in the treatment of other types of cancer.
- Gene editing: In this, a gene from the T cells that encode a protein called PD-1 that tumor cells can use to evade an immune attack, is removed using a technology called CRISPR. This can further enhance CAR T-cell therapy.
- Gene transfer: It is a new treatment modality that introduces new genes into a cancerous cell or the surrounding body cells to cause cell death or slow the growth of the cancer.
- Personalized Cancer Vaccines: By comparing the DNA sequences of the tumor and of healthy cells, cancer mutations can be identified especially the ones more likely to stimulate a strong reaction from the immune system. The vaccines are given in the form of messenger RNA (mRNA- similar technology has been used in some COVID vaccines), which gives cells the instructions to create a particular cancer antigen that trains the immune system against the tumor. Such personalized vaccines could be particularly useful for certain cancer that often carry high numbers of mutations, such as lung and bowel cancer.
- Microbial therapy: Specific bacteria and viruses have been studied which live and thrive in the oxygen-deprived environment of cancer cells. Therefore, these microbes cannot directly harm the human cells but can eat through most of the mass of a tumor. They also alert and stimulate our immune system by making the cancer more visible to the immune cells to destroy it.
Also read:
Reference:

