Human papillomavirus (HPV) is the most common sexually transmitted infection (STI), an infection that causes genital warts and cancer of the cervix (the lower part of the uterus that connects to the vagina). Many people don’t develop any symptoms but can still infect others through sexual contact.
CERVICAL CANCER
Screening
HPV infections cause almost all cervical cancers. Type 16 and 18 are the most common high-risk types, accounting for most of cervical cancers. Cervical cancer may take 20 years or longer to develop after the initial infection. Getting vaccinated against HPV infection is the best way to protect against cervical cancer.
The HPV infection and early cervical cancer typically don’t cause symptoms, so screening is the main-stay of diagnosis Current guidelines for screening recommend that:
- Women ages 21 to 29 have a test that checks cervical cells for cancer, called a Pap test, every 3 years. Pap test involves scraping cells from the cervix with a swab, and examining under the microscope for any abnormality.
- Women aged 30 to 65 are advised to keep having Pap tests every 3 years, or a Pap test every 5 years along with a test for the genetic material of the virus (HPV DNA test). PAP-HPV co-testing is not routinely recommended or done in low-income countries unless indicated as the expense is very high.
- Women over 65 can stop testing if they’ve had three regular Pap tests in a row, or two HPV DNA and Pap tests with no irregular results.
Interpreting the Pap test
- Atypical squamous cells of undetermined significance (ASC-US) and low-grade squamous intraepithelial lesion (LSIL) are both abnormal Pap test results that indicate early changes in the cervical cells.
- The most common abnormal Pap test result, ASC-US indicates changes in the cervical cells that are suggestive of an HPV infection.
- ASC-US is less severe than LSIL, and patients with ASC-US often achieve total remission (resolution) in follow-up Pap smears.
- HSIL (high-grade squamous intraepithelial lesion) indicates high-risk of cervical cancer.
- CIN (Carcinoma in situ) was the term used in the past. LSIL (Low-grade Squamous Intraepithelial Lesion) is generally equivalent to CIN 1, indicating mild dysplasia, while HSIL (High-grade Squamous Intraepithelial Lesion) can be CIN 2 or CIN 3, representing more severe dysplasia (abnormality of cells).



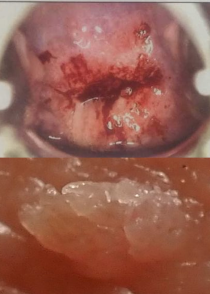
Colposcopy
When Pap smear shows any abnormality, and the HPV-DNA test is positive, then a colposcopy is done. A colposcopy is a medical procedure that uses a special magnifying instrument called a colposcope to examine the cervix, vagina, and vulva. It is typically performed after an abnormal Pap smear and/or positive HPV-DNA test, or if there are visible lesions on the cervix. The procedure helps in detecting cervical cancer and precancerous changes. Acetic acid (vinegar) or iodine solutions may be applied to the cervix to highlight abnormal areas. If abnormal areas are identified, a biopsy (tissue sample) may be taken for further examination under a microscope.
PAP-LSIL
If the colposcopy is normal, repeat PAP and HPV testing after 1 year. If HPV testing shows low-risk HPV strains, then no other intervention is done, and follow-up is done after 1 year with PAP-HPV testing. In most cases, there is spontaneous resolution. However, if the patient seems immunocompromised, then a course of antivirals may be given by some doctors. If the HPV test is negative, then a routine follow-up is after 3 years.
PAP-HSIL
Post colposcopy, excision biopsy where the area is surgically removed (large loop excision of the transformative zone), or an ablative procedure (thermal/cryotherapy) is done to destroy the affected tissue.
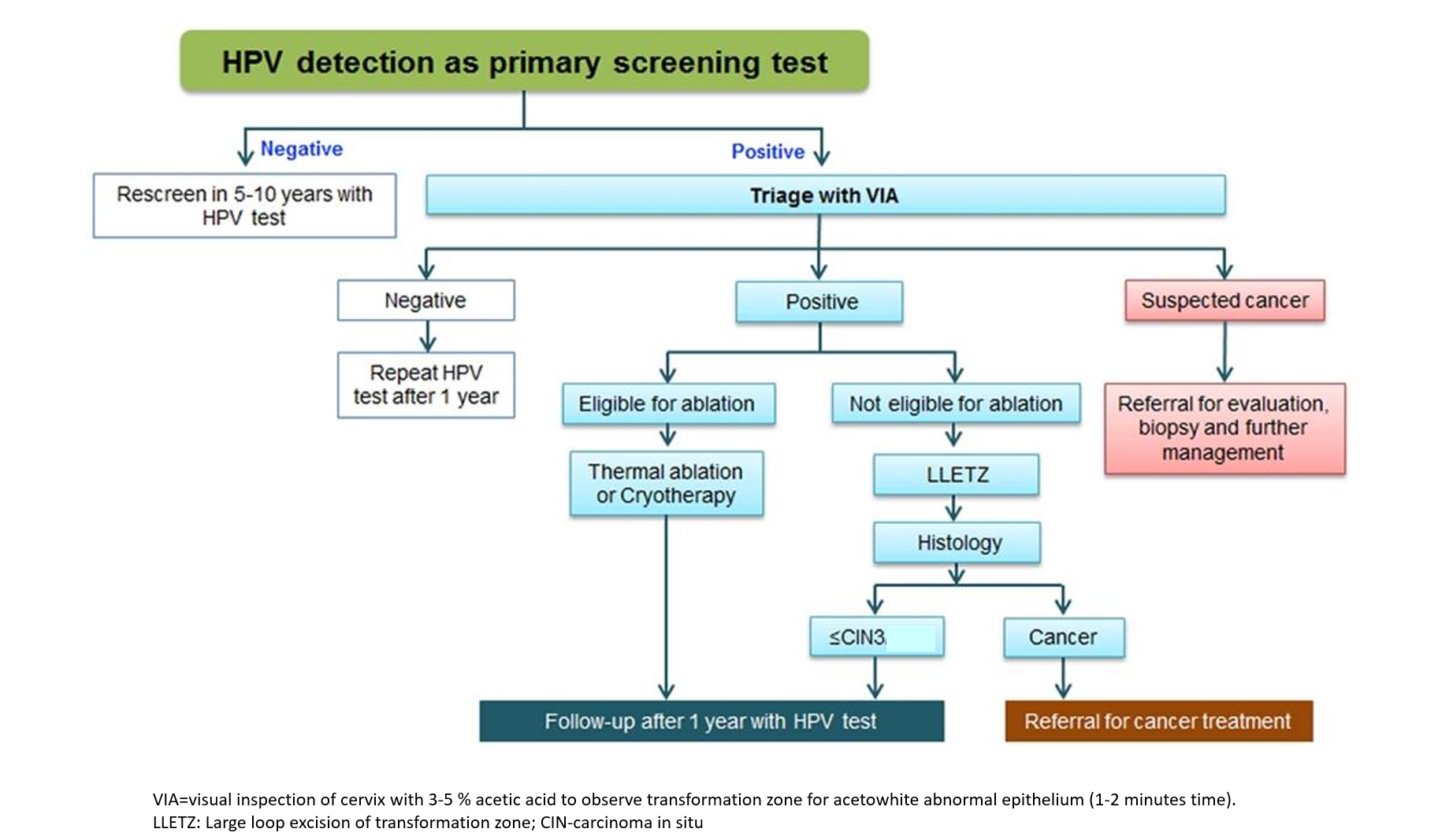
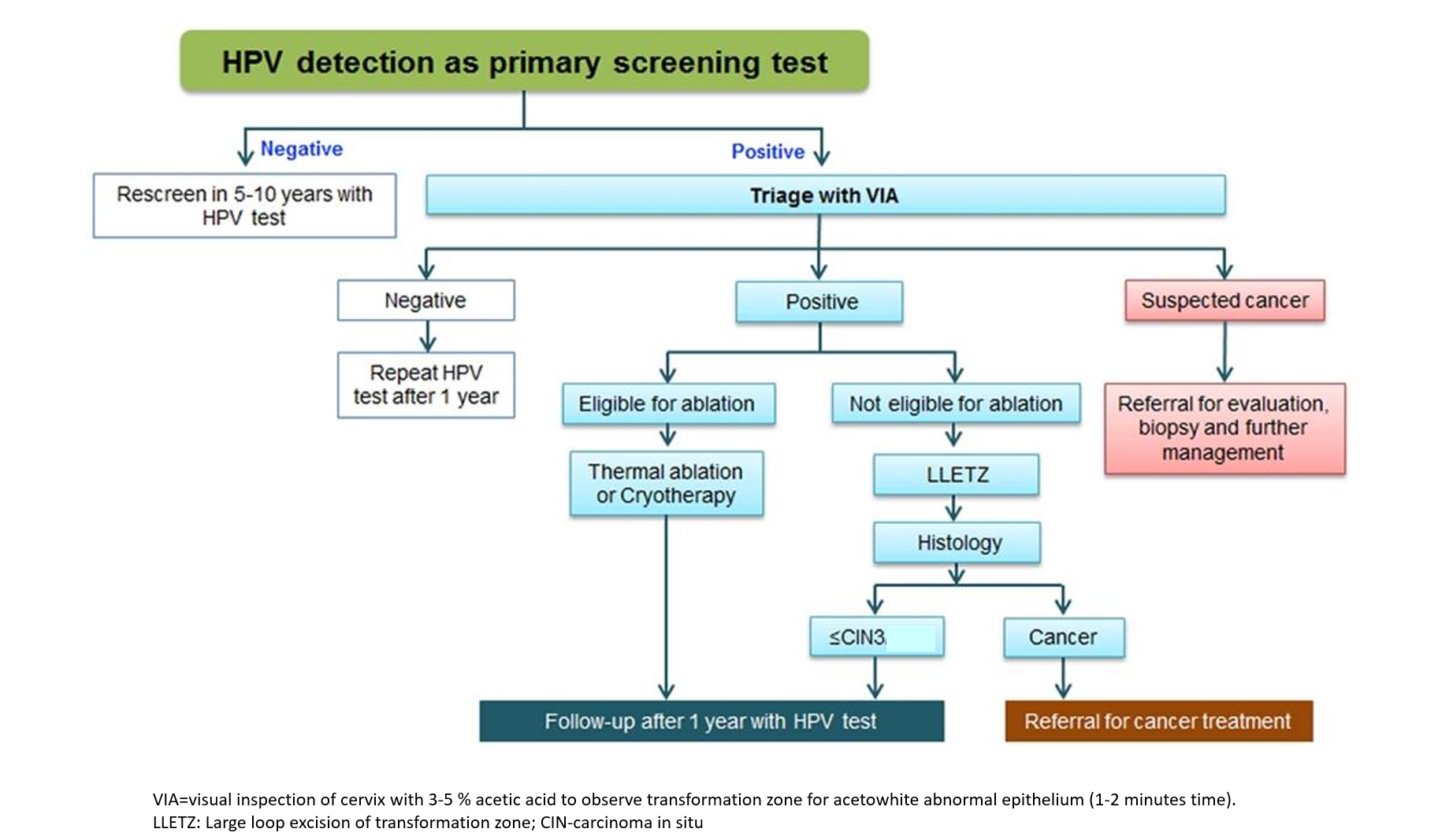
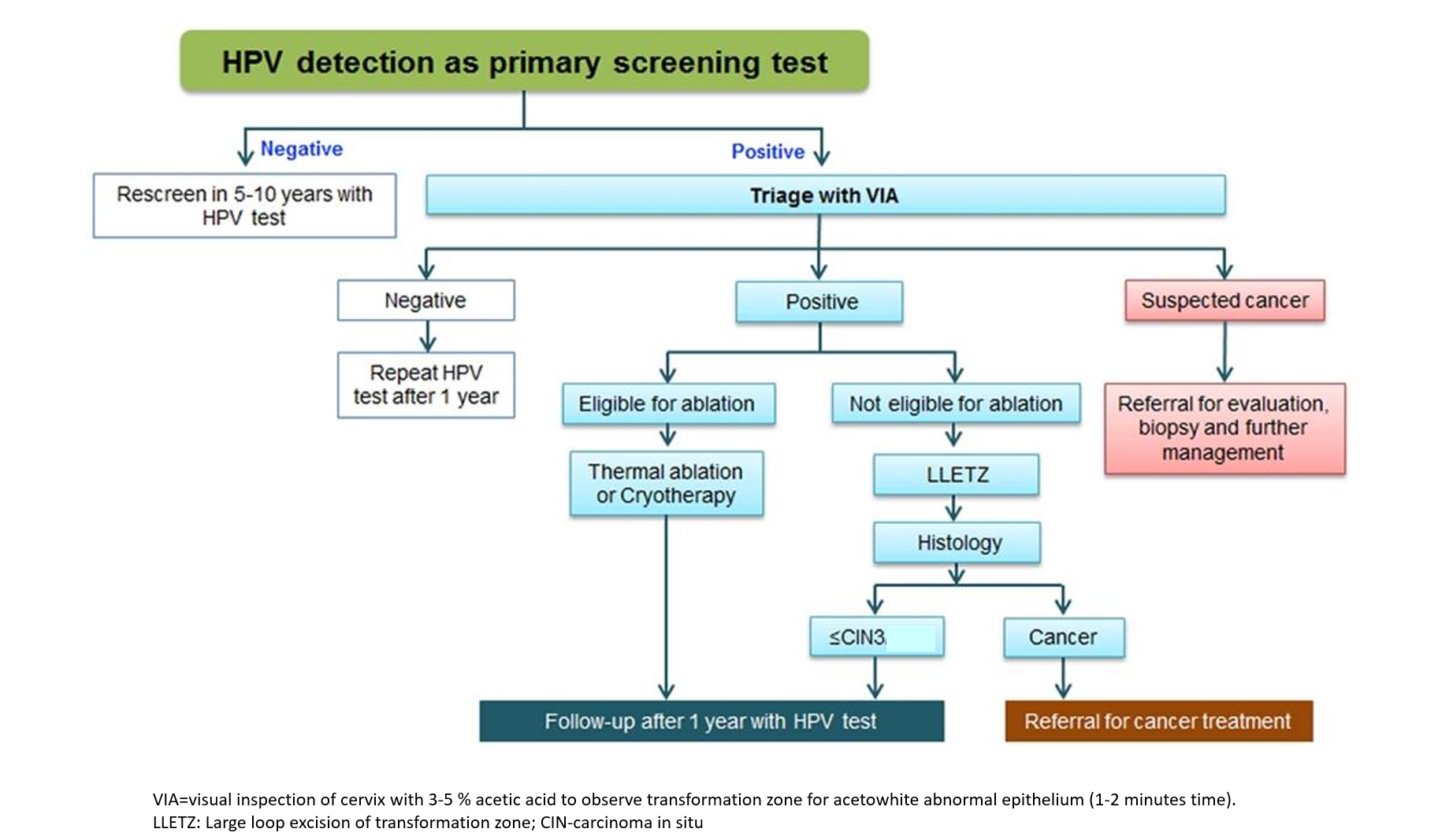
WHO has now recommended HPV testing as the preferable primary screening test worldwide. Most developed and high-income countries have done away with Pap and are doing HPV testing as the first test. If the HPV test is negative, then the woman can wait 5-10 years for her next screening test (5 years if risk factors present). Even in India, most big hospitals have also switched to this protocol. It helps skip double testing Pap+HPV and can also reduce the frequency of testing from 3 years (Pap) to 10 years (HPV) in the normal post-30-year old adult woman population. Also, now home-based self-collection cervical sample kits are being made available that can be used for HPV and triage.
GENITAL WARTS
Genital warts appear as small, flesh-colored, or gray bumps, sometimes clustered like cauliflower, in the genital or anal area. While often painless, they can cause itching, discomfort, or bleeding. Genital warts are caused by the Human Papillomavirus low-risk types mainly 6 and 11, and sometimes 1, 2, 4.
Warts can be treated through various methods including topical medications, cryotherapy (freeing), electrocautery (localized burning), laser surgery, or surgical removal. Topical Medications include creams/solutions of drugs like imiquimod, podophyllotoxin, sinecatechins and trichloroacetic acid (TCA). Sometimes, interferons (antiviral medications) may be injected into genital warts. Treatment aims to remove visible warts, but the underlying HPV infection usually resolves on its own within 1-2 years.
Prevention includes practicing safe sex, condom use, and getting the HPV vaccine.
HPV VACCINE
Vaccination is the best and safest way to prevent HPV infection and is of use in the years of adolescence and early adulthood. After the age of 25 years, in most women natural HPV infection may occur.
There are three types of vaccines available. All the below vaccines are effective in preventing cervical cancer, while quadrivalent and 9-valent vaccines also protect against genital warts in addition to cervical cancer. The 9-valent further protects against some cases of vaginal, vulvar, anal, and oropharyngeal cancers. Different countries have their own recommended vaccines in the immunization program depending on cost and access. The HPV vaccine is given as 2 doses 6 months apart in the 9-14 years age group, and as 3 doses at 0,2, and 6 months in the 15-26 years age group, after which it is not recommended or of much benefit.
- Bivalent – protects against HPV types 16 and 18, responsible for approximately 70% of cervical cancer cases globally
- Quadrivalent – protects against four HPV types that is 16 and 18 are responsible for most cervical cancers, and types 6 and 11 causing most of the genital warts.
- 9valent – protects against nine different types of HPV: 6, 11, 16, 18, plus 31, 33, 45, 52, and 58.
Also read:
Gynecological Infections – Vaginitis and Pelvic Inflammatory Disease