What is asthma?
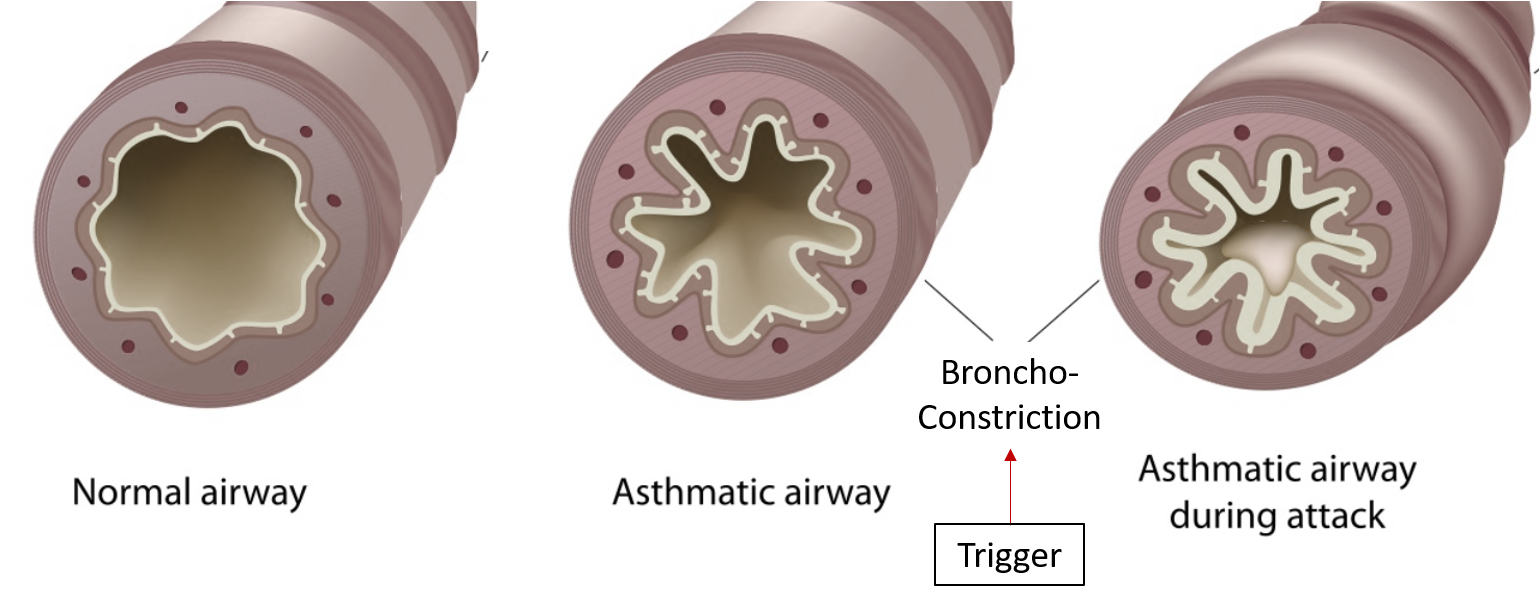
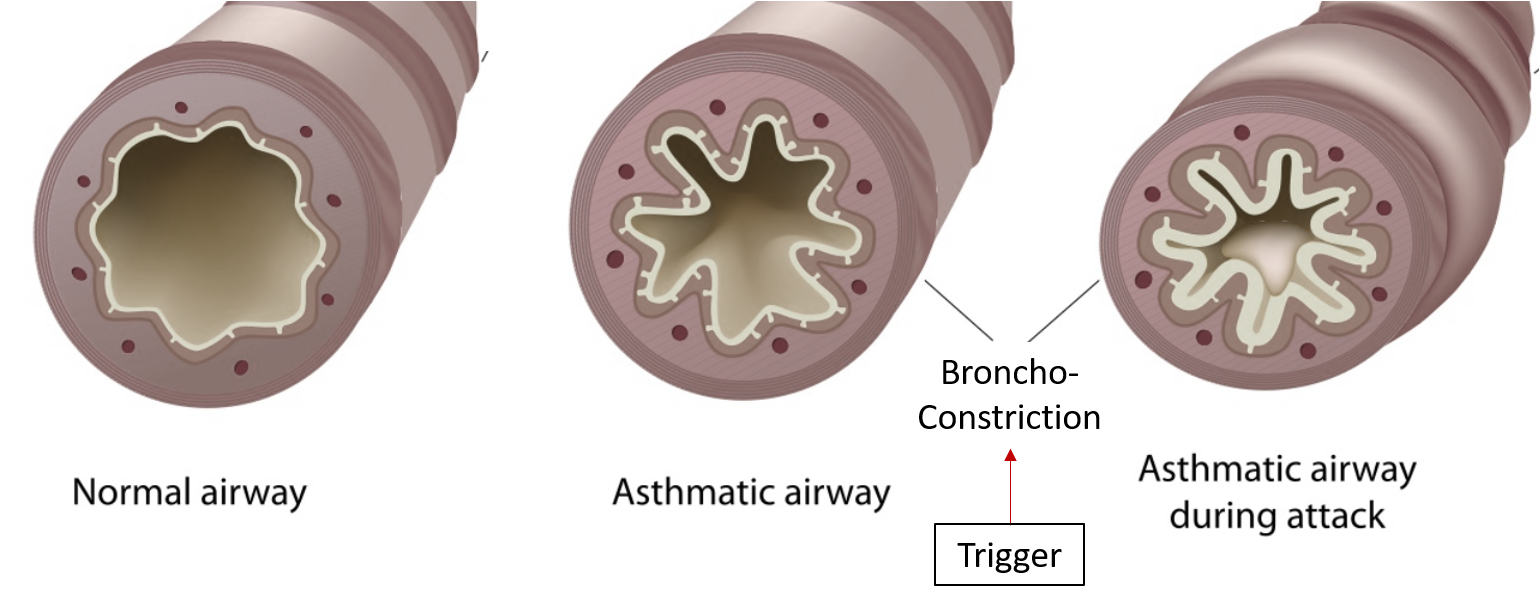
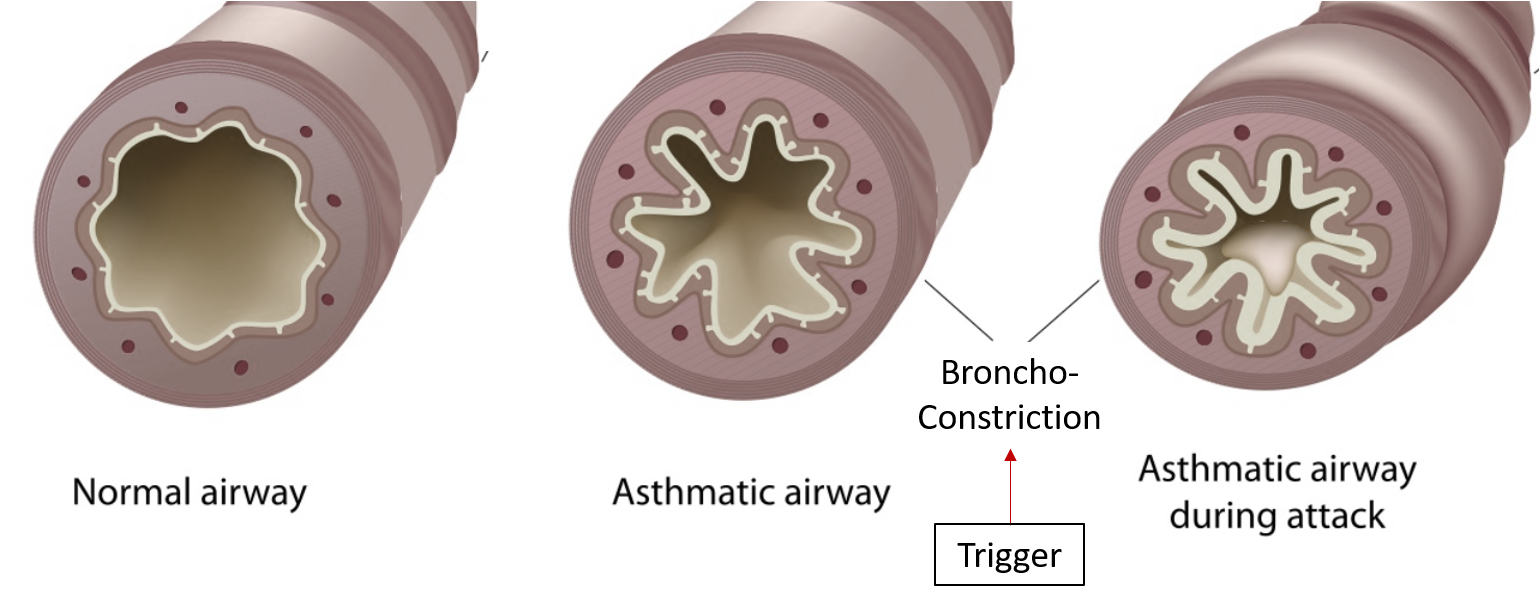
Asthma is a chronic inflammatory disease in which the lower airways, i.e. breathing passage, swell up and get narrowed thereby causing breathlessness (difficulty in breathing). This happens in response to specific triggers. It is characteristically associated with wheezing (whistling sounds coming from the chest) and sometimes coughing.
What are the types of asthma?
- Allergic asthma: This is the most common type, accounting for almost 60% of all cases, and the majority of asthma starting in childhood. Various environmental allergens (both indoor and outdoor) can trigger an asthmatic attack. These include dust (house dust mite -HDM), pollen, food items, fungus, animal parts like fur, hair, etc.
- Non-Allergic asthma: Also known as “Intrinsic asthma”, this form of asthma is not triggered by any allergen. It is more commonly seen in adults. Genetic and some environmental factors like cold / flu, humidity, stress, smoke irritants, and air pollution are responsible for non-allergic asthma.
- Exercise-induced asthma: Symptoms occur immediately or soon after exercising or playing, especially in cold weather. Patients will experience sudden onset breathlessness, wheezing, coughing, and chest tightness within a few minutes of strenuous activity.
- Occupational asthma: An attack after exposure to a particular trigger in the workplace. The common job-related agents include paints, chemicals, aerosols, and wheat (bread industry).
- Cough variant asthma: A dry, non-productive cough is the main symptom. There are no other “classic” symptoms of breathlessness and wheezing. It is usually seen in children, and night-time coughing is prominent due to nocturnal narrowing of airways and increased airflow resistance during sleep.
What are the triggers of asthma?
The different factors responsible for setting off an asthmatic attack (exacerbation or worsening) include exposure to:
- House dust, molds/fungi (usually found on seepage in damp walls)
- Cigarette (tobacco) smoke
- Pollen from flowers, trees, and grass
- Fur/feathers from pets
- Strong smells (paints) and sprays (perfumes)
- Air pollution
- Sudden changes in weather
- Viral upper respiratory tract infections (colds and flu)
- Particular food items
- Exercise and physical strain
- Emotional upsets and mood swings
- Certain medications (especially painkillers)
In more than half of the patients, the disease manifests early during childhood after being exposed to any of the aforementioned triggers.
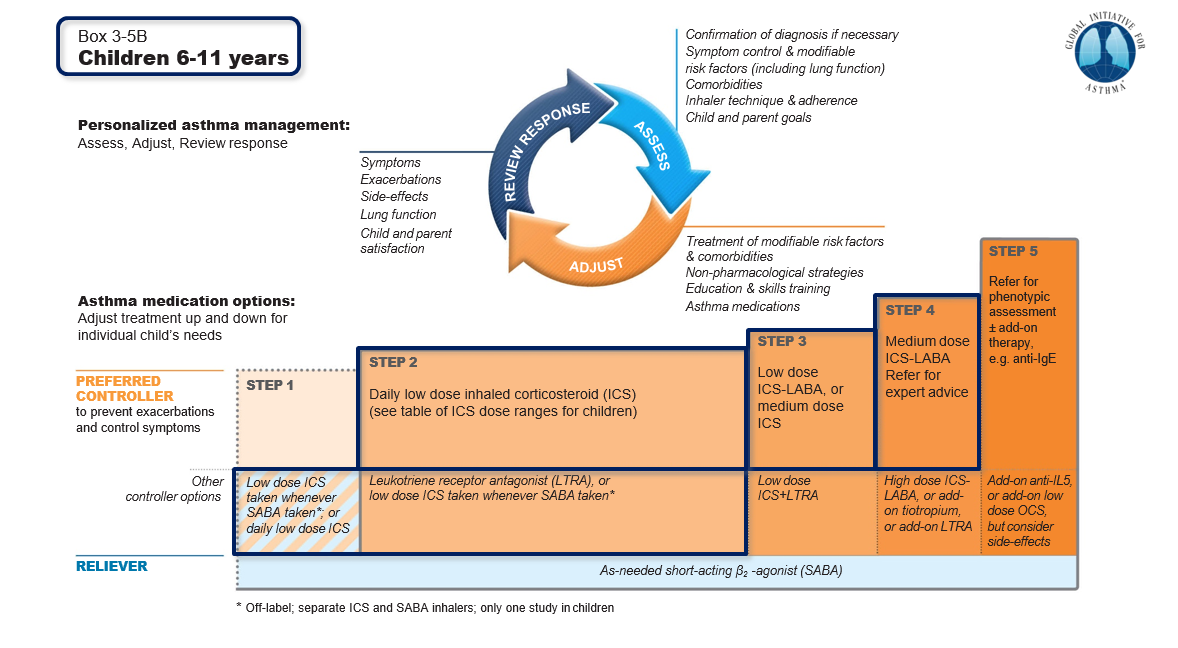
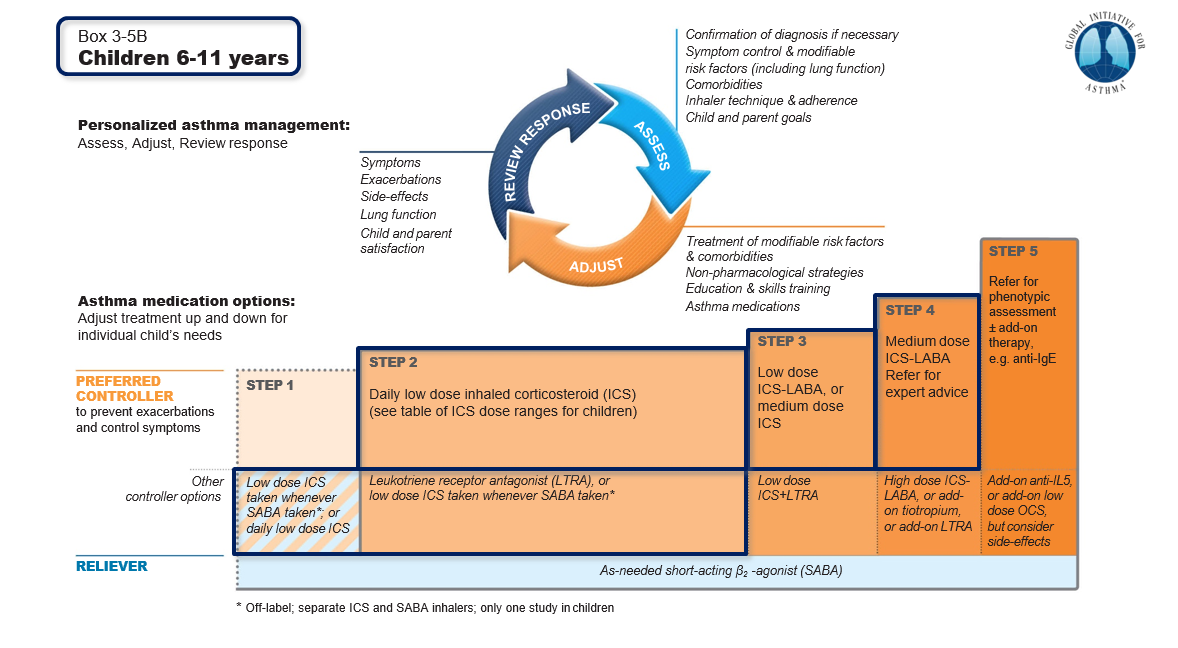
What is the treatment for asthma?
Allergen avoidance is the first and foremost step that should be taken by all asthmatics. However, this is not always possible. Should symptoms suggestive of asthma occur for the first time, it is essential to consult a specialist doctor who would ask specific questions about the disease and suggest a few tests (pulmonary function tests – PFT). Once the diagnosis is confirmed, the treatment prescribed would comprise tablets/syrups for immediate short-term relief and inhaled medications for long-term usage.
Administration of medicines via the inhaled route is the mainstay of therapy. This can be in the form of metered-dose aerosolized inhalers, dry powder capsules, and nebulized respules.
- “Controller” (preventive) medicines: these have to be taken every day in order to avoid getting an asthmatic attack. The main type is the inhaled corticosteroids (ICS). Since the medication is directly deposited into the airways by the inhalational route, there are hardly any of the side effects that are mainly seen with the long-standing usage of steroids taken as tablets (oral corticosteroids -OCS) or injections. Usage of a spacer device and rinsing the mouth after taking the inhaled medicines help in decreasing drug deposition in the mouth.
- “Reliever” medicines: these inhaled medications are prescribed on an SOS basis and should be taken whenever an attack occurs in spite of taking the regular preventer inhaler. The most common reliever medication is a short-acting beta-agonist (SABA) like salbutamol.
Can asthma be cured?
Although symptoms may be controlled with regular treatment taken over a period of time, the disease per se is incurable. If the “controller” medications are not taken regularly (patients tend to discontinue the treatment after complete relief is obtained), permanent airway damage can occur with progressive deterioration of the PFT over years. To avoid this, the “controller” medications should be taken regularly without fail in order to keep the airway inflammation from worsening.
What are the warning signs of an asthma attack?
- increased usage of reliever medication (usually should be less than 4 times a month)
- sleep disturbance due to cough, wheezing, or breathlessness
- absenteeism from school/college/work due to asthma
- requiring extra effort to perform daily chores and activities
What if the asthma attacks keep recurring despite regular treatment?
Many times patients with asthma have associated allergic rhinitis and sinusitis i.e. allergic inflammation of the nasal passages and the paranasal sinuses. In order to obtain optimal control of asthma, allergic rhinosinusitis should also be evaluated and simultaneously treated with intranasal corticosteroid sprays. Another important co-morbid condition is the presence of gastro-esophageal reflux disease (GERD) which presents as acidity and burning sensation in the chest after meals.
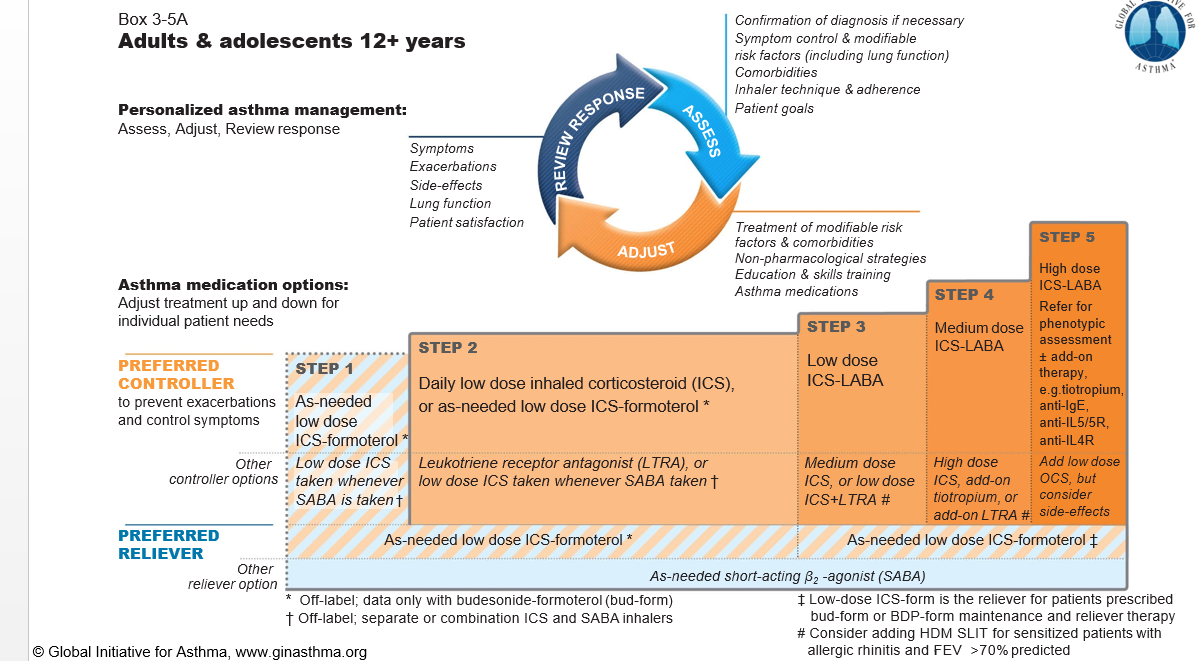
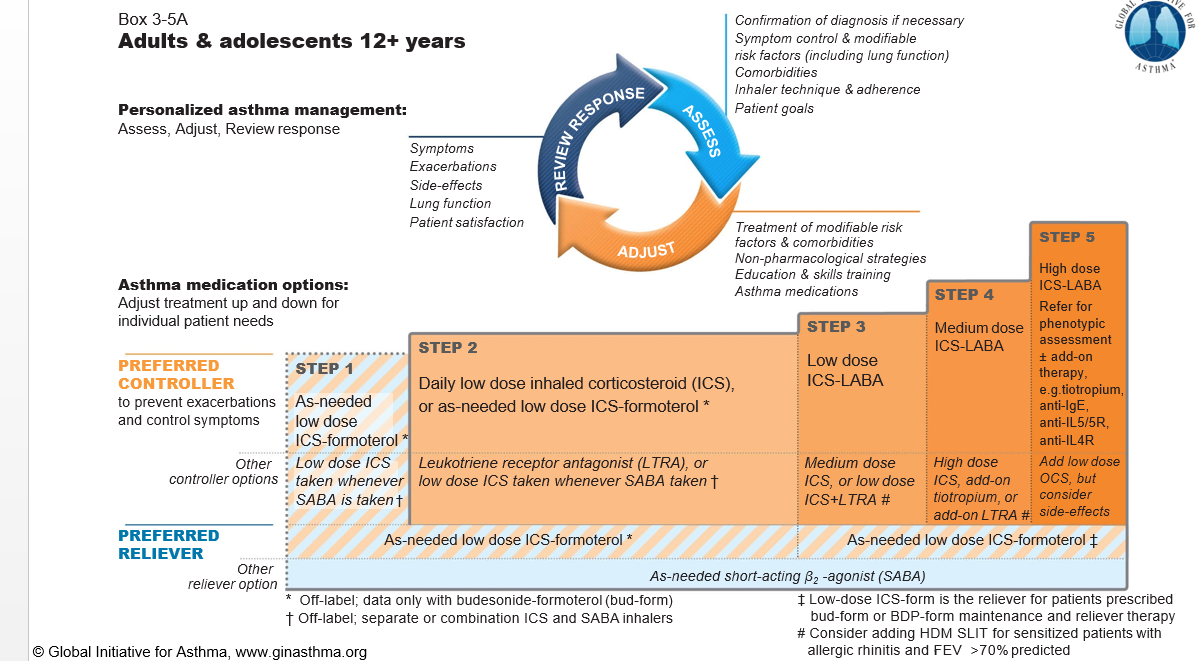
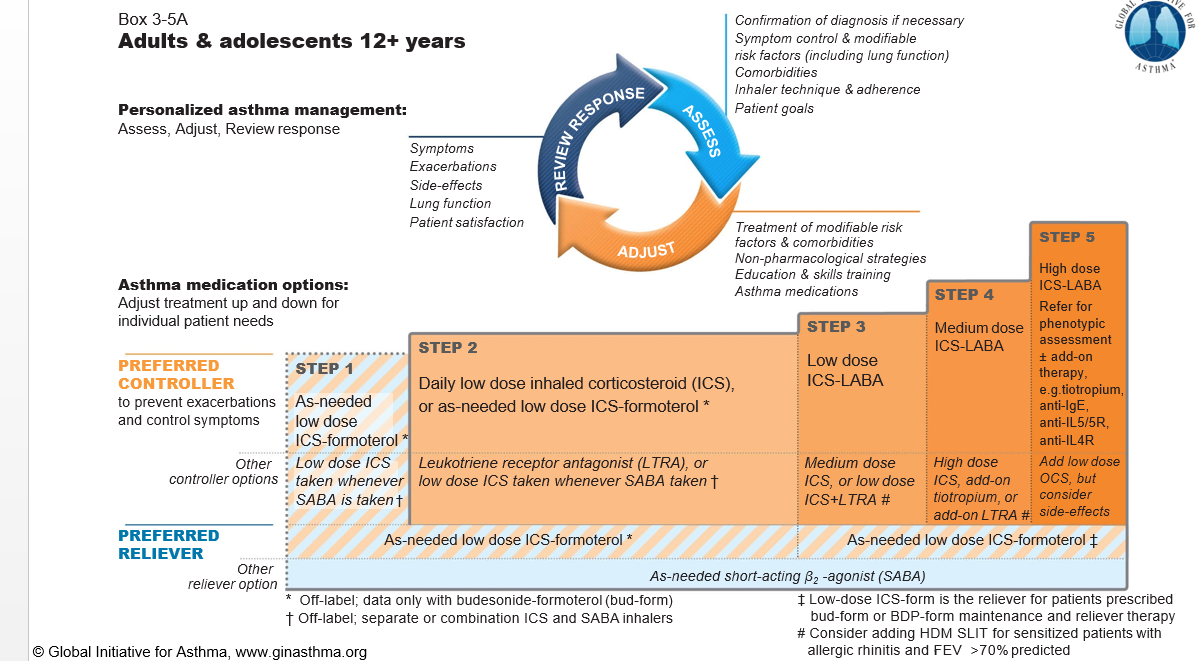
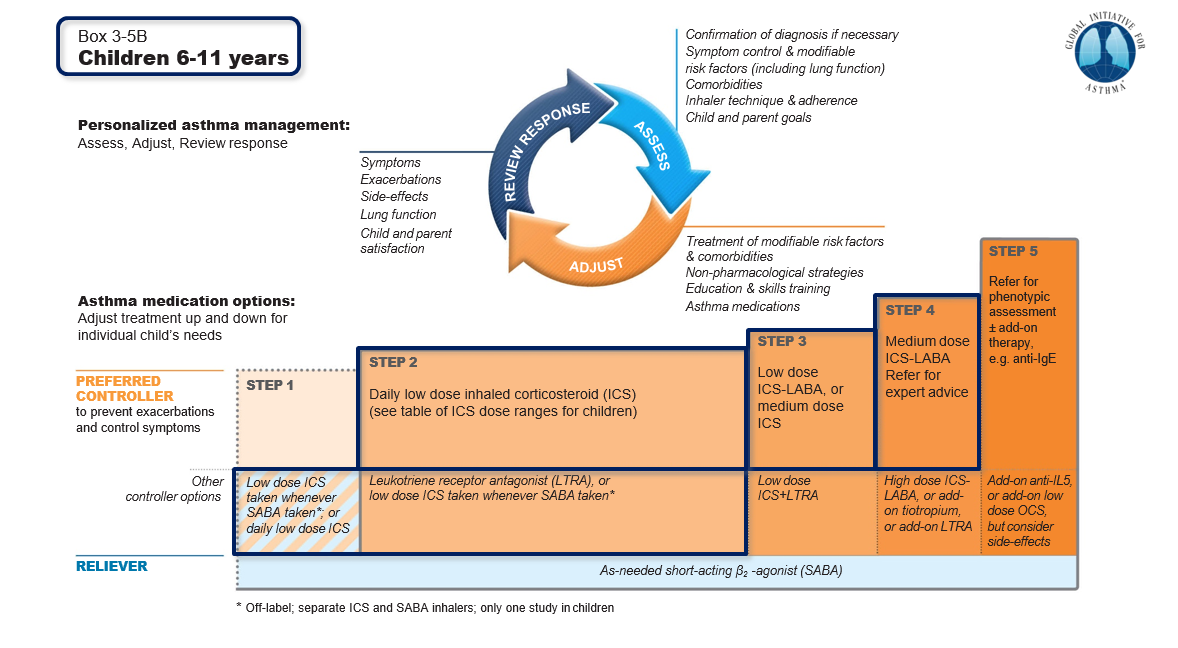
Global Initiative for Asthma (GINA) 2020 – Treatment Update
- Inhaled SABA has been the first-line treatment for asthma for 50 years. This dates from an era when asthma was thought to be a disease of bronchoconstriction. Patient satisfaction with, and reliance on, SABA treatment is reinforced by its rapid relief of symptoms, its prominence in emergency departments and hospital management of exacerbations, and low cost. Patients commonly believe that “My reliever gives me control over my asthma”, so they often don’t see the need for additional treatment.
- Studies have now shown that regular or frequent use of SABA is associated with adverse effects. Other associated issues include Beta2-receptor downregulation (reduced sensitivity), decreased broncho-protective effect and bronchodilator response, rebound hyperresponsiveness, and increased allergic response and eosinophilic airway inflammation.
- Higher use of SABA is associated with adverse clinical outcomes. Dispensing of ≥3 canisters per year (average 1.7 puffs/day) is associated with a higher risk of emergency department presentations. Dispensing of ≥12 canisters per year is associated with a higher risk of death.
- GINA emphasized poor adherence with maintenance controller therapy as a modifiable risk factor for exacerbations (as it exposes the patient to risks of SABA-only treatment).
- GINA found no evidence to support a Step 1 SABA-only recommendation. In 2014, as an interim safety measure, GINA restricted SABA-only treatment to patients with symptoms less than twice a month and no risk factors for exacerbations.
- For safety, GINA now no longer recommends SABA-only treatment for Step 1. This decision was based on evidence that SABA-only treatment increases the risk of severe exacerbations, and that adding any ICS significantly reduces this risk.
- GINA now recommends that all adults and adolescents with asthma should receive symptom-driven or regular low dose ICS-containing controller treatment, to reduce the risk of serious exacerbations.
Key points:
|
Key points:
|
COVID-19 considerations in asthma
- Advise patients with asthma to continue taking their prescribed asthma medications, particularly ICS and OCS if prescribed. Asthma medications should be continued as usual. Stopping ICS often leads to potentially dangerous worsening of asthma.
- For patients with severe asthma: continue biologic therapy (like omalizumab), and do not suddenly stop OCS if prescribed
- Make sure that all patients have a written asthma action plan with instructions about:
- increasing controller and reliever medication when asthma worsens.
- taking a short course of OCS for severe asthma exacerbations when seeking medical help.
- Avoid nebulizers where possible:
- nebulisers increase the risk of disseminating virus to other patients and to healthcare professionals.
- pressurised metered dose inhaler via a spacer is the preferred treatment during severe exacerbations, with a mouthpiece or tightly fitting face mask if required.
- COVID-19 vaccines are usually safe to give in asthmatics; however, they should be administered in healthcare settings where anaphylaxis (severe allergic reaction) can be treated if it occurs.
Dr. Chandramani Panjabi, M.D. (Respiratory Diseases) is a Senior Consultant Chest Specialist and Head of Pulmonology & Respiratory Allergies, as well as Nodal Officer for COVID-19 at Mata Chanan Devi Hospital, Janak Puri, New Delhi. He is also the Director, Breathe Easy – The Lung Clinic, Janak Puri, New Delhi. His area of interest includes Asthma and Chronic Obstructive Pulmonary Disease (COPD) in which he has acclaimed work and publications.
Also read: