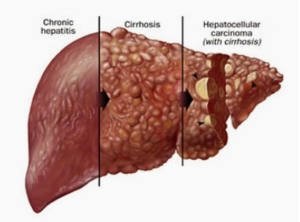
Cirrhosis occurs when chronic liver inflammation (hepatitis) either due to infective hepatitis, alcoholic liver disease (ALD), Non-Alcoholic Steato Hepatitis (NASH), or other causes, leads to scarring (fibrosis) of the liver. When fibrosis leads to the loss of the recognizable normal structure of the liver due to replacement by scar tissue, thereby compromising liver function, it is called cirrhosis.
Cirrhosis always develops as a result of long-standing inflammation (chronic hepatitis) of the liver. The causes of cirrhosis are:
- chronic viral hepatitis (B, C)
- alcoholic liver disease (ALD)
- NAFLD (non-alcoholic fatty liver disease),
- chronic exposure to harmful agents/drugs/toxins
- autoimmune diseases
- hypoxia (ischemia) – lack of proper blood supply (hypoxia or ischemia)
- Cirrhosis always develops as a result of long-standing inflammation (chronic hepatitis) of the liver.
Chronic hepatitis and cirrhosis also increase the risk of developing liver cancer (hepatocellular carcinoma)
PORTAL HYPERTENSION
Blood from the entire digestive (gastrointestinal) tract flows through the portal vein into the liver, and thereafter from the liver to the heart through the hepatic veins. Cirrhosis causes restriction of this flow, leading to back pressure in the portal and gastrointestinal veins (portal hypertension). This leads to many of these veins and their smaller connections (collaterals) becoming dilated and tortuous (varices) as seen in the lower esophagus, stomach, and rectum. These varices can rupture and cause massive bleeding, manifesting as vomiting blood (hematemesis), or a rectal bleed.
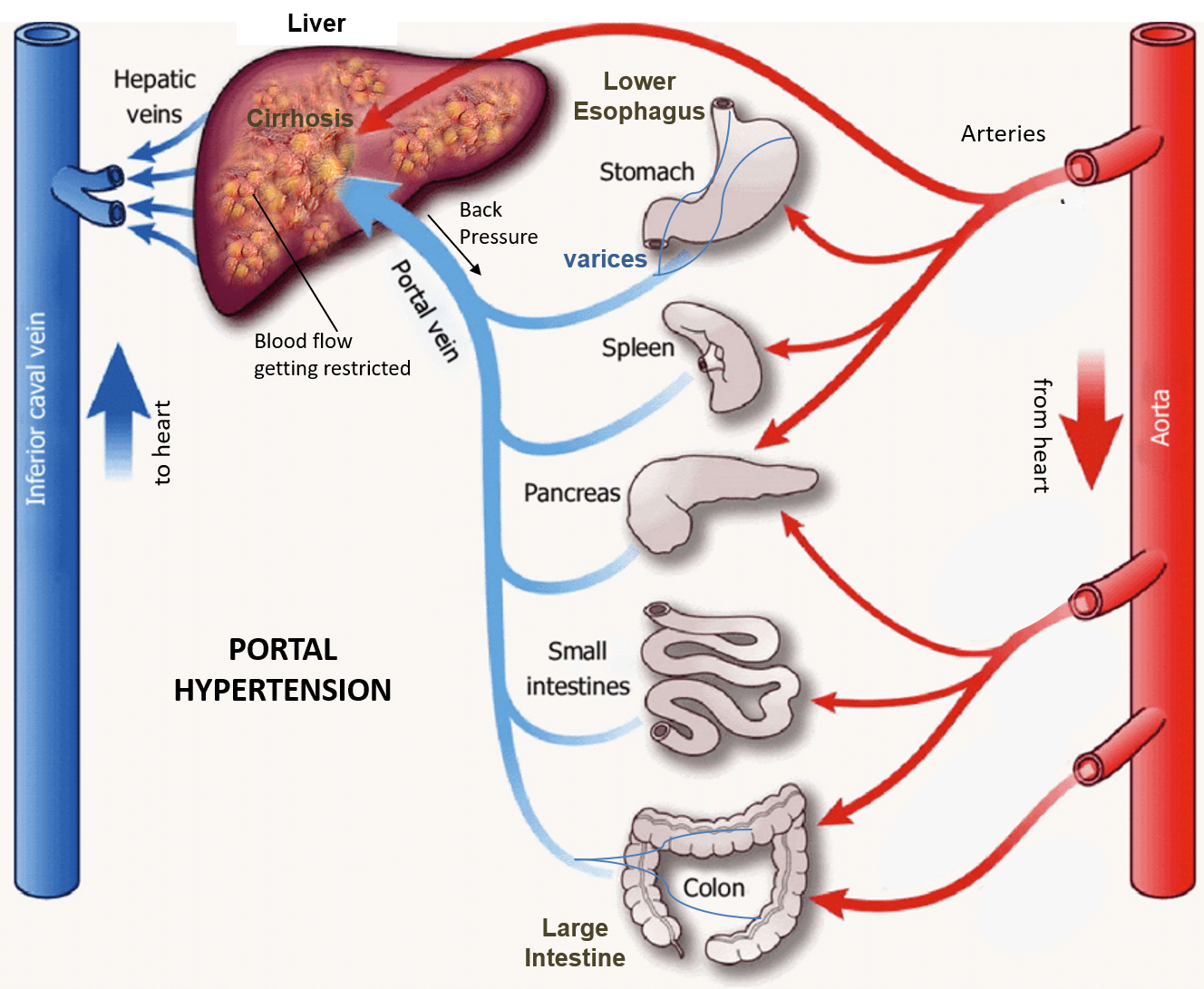
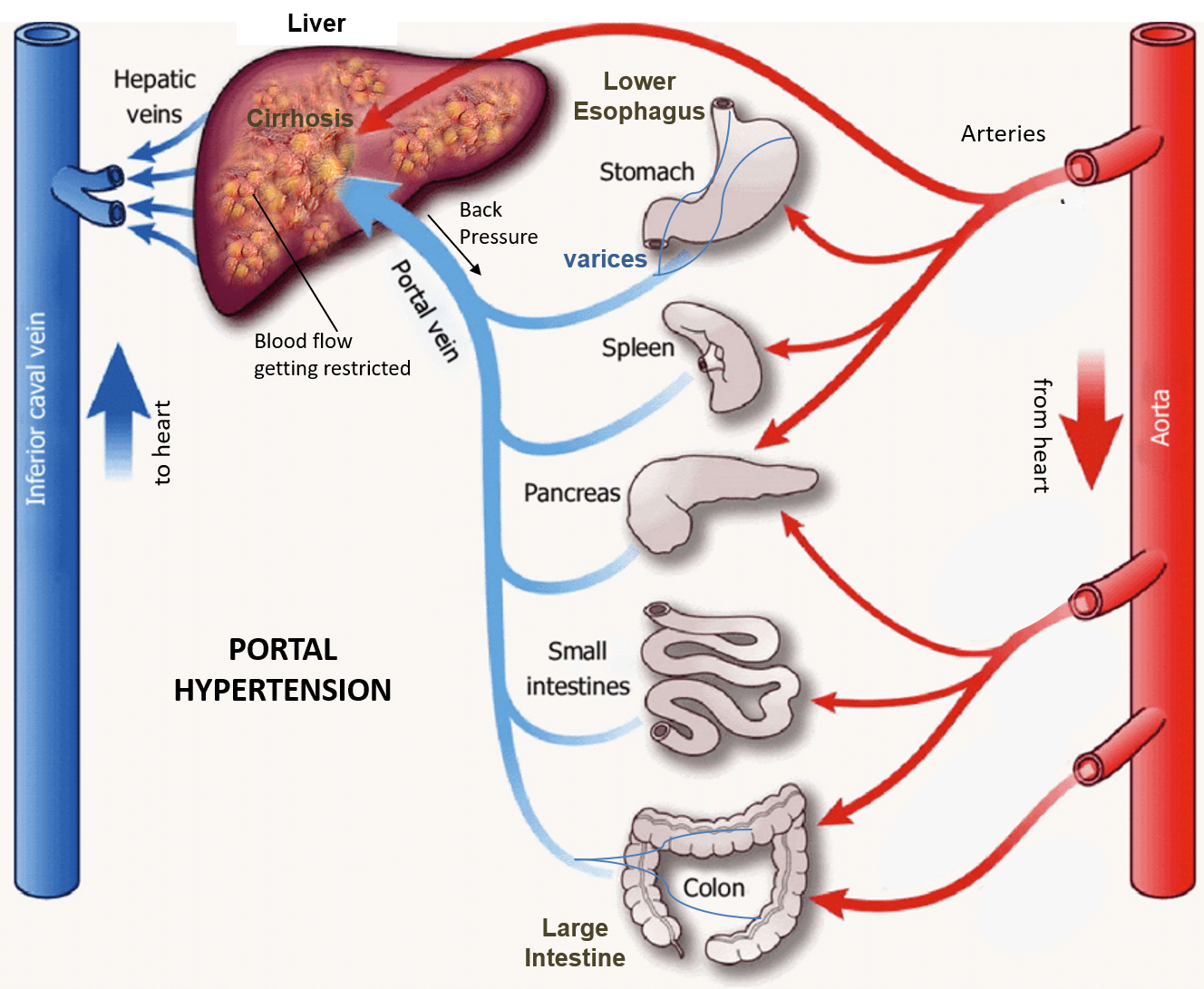
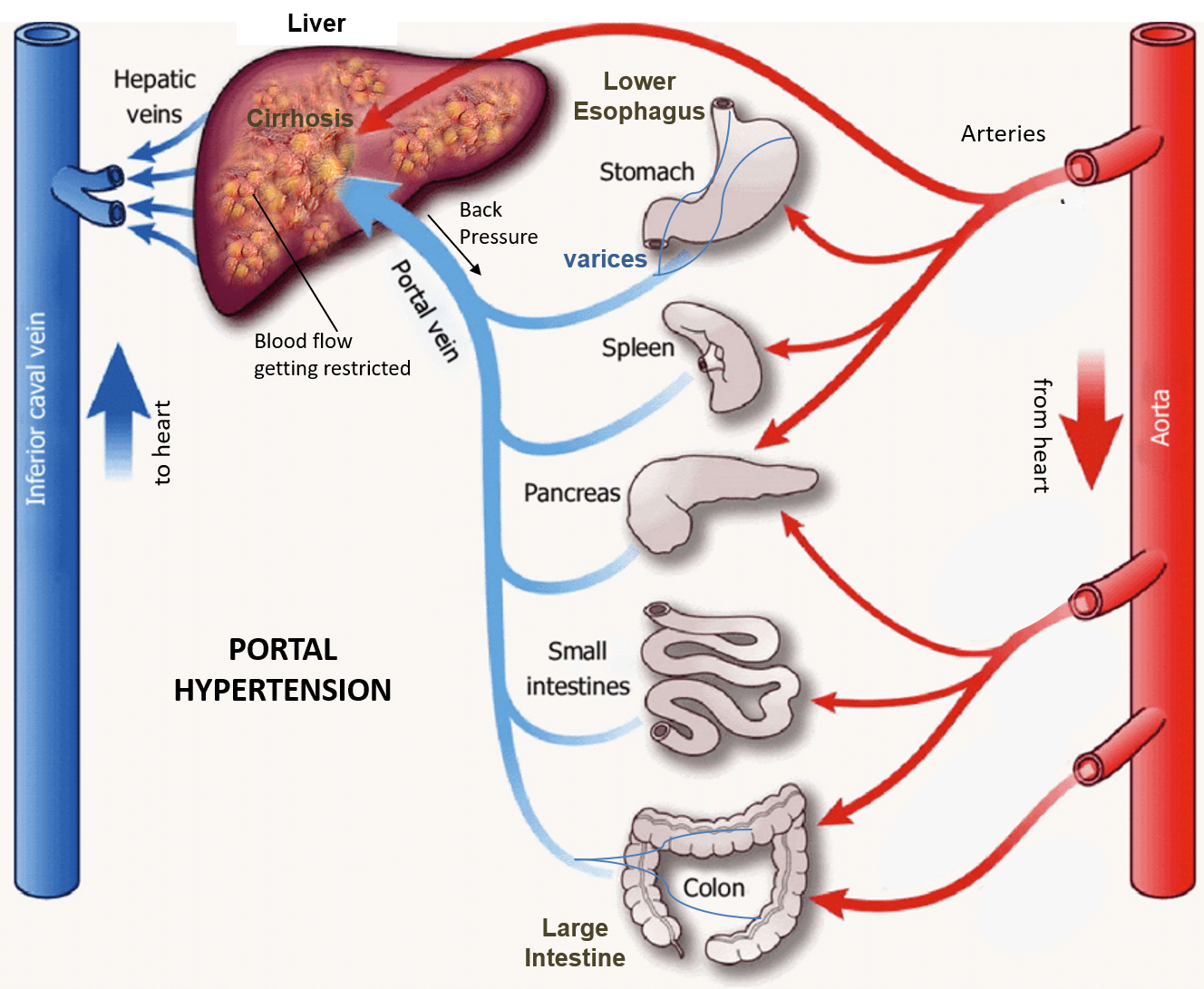
Ascites (fluid collection in the abdomen) occurs as a result of high pressure in the abdominal veins due to portal hypertension as well as low blood levels of the protein albumin due to compromised liver function.
The liver is the organ detoxifying a lot of harmful substances in our body like ammonia that starts to rise with advanced cirrhosis affecting the functioning of many other organs.
Hepatic encephalopathy (HE) refers to compromised brain function and altered mental state due to ammonia exposure, inflammation, and swelling in patients with cirrhosis. This manifests as confusion, drowsiness, flapping tremors, personality changes, slurred speech, disorientation, and impaired muscle coordination. HE can be precipitated by the following factors:
- gastrointestinal bleed
- infections (especially like abdominal – peritonitis, or blood infection-sepsis)
- electrolyte imbalance like low sodium or salt (hyponatremia)
- dehydration
- low blood albumin
- constipation
- compromised kidney function
- agents that suppress the central nervous system (alcohol, and drugs like opioids, benzodiazepines, antidepressants, and antipsychotics),
- surgical procedures like shunts
Decompensated Cirrhosis is the term used when signs of portal hypertension appear clinically like the presence of ascites, bleeding varices, or encephalopathy.
Cirrhosis can also result in compromised kidney function and kidney failure (called hepatorenal syndrome).
Cirrhosis eventually causes chronic liver failure.
Signs of chronic liver failure
- Jaundice (yellowing of skin/eye)
- Skin rash with spider angiomas (or spider nevi- red spots on the skin with a central dilated blood vessel radiating outward like spider legs), superficial bruising/bleeding spots, and severe itching (pruritus).
- Reddening of palms and bulging club-like fingers
- Fluid in the abdomen (ascites)
- Prominent tortuous blood vessels around the umbilicus (caput-medusae)
- Bleeding from vessels of food pipe and stomach (esophageal /gastric varices) that manifests as blood in the vomit (hematemesis).
- Bleeding from rectum (melena) or the formation of hemorrhoids (piles)
- Dark urine and pale stools
- Severe fatigue and weakness
- Swelling of feet and ankles
- Sweet fecal odor in the breath (due to ammonia)
- Hepatic encephalopathy and altered mental status
- Progression to coma



MANAGEMENT
Diagnosis
Liver function tests (LFT) are blood tests that help to assess the amount of liver inflammation and the functioning of the liver, and also help to monitor disease progression/improvement. These include liver enzymes (SGOT, SGPT, ALP, GGT), bilirubin, proteins (albumin and globulin), and prothrombin time (PT-INR).
Blood tests include those for sugar, lipid profile, thyroid, blood counts and renal function may also be performed.
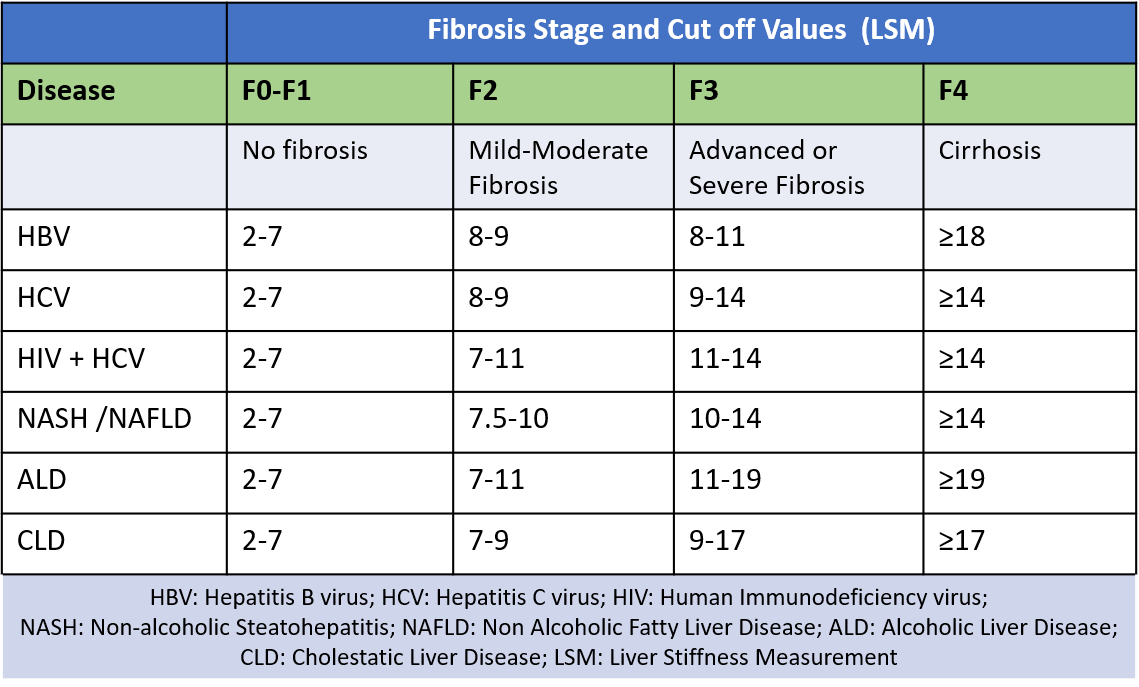
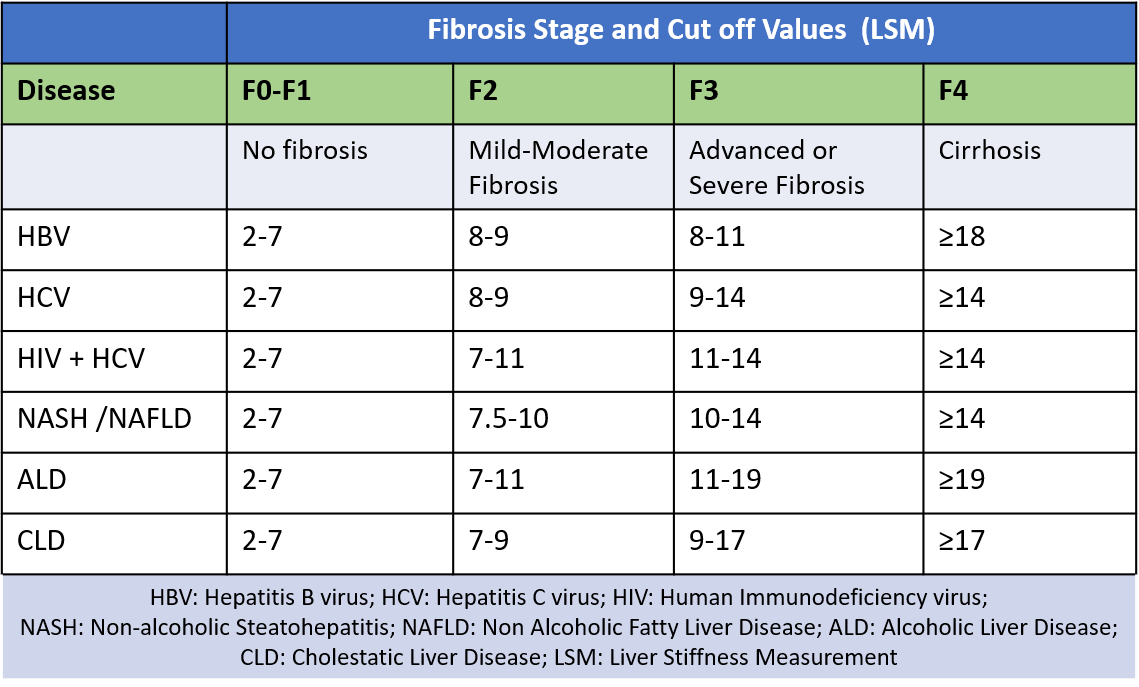
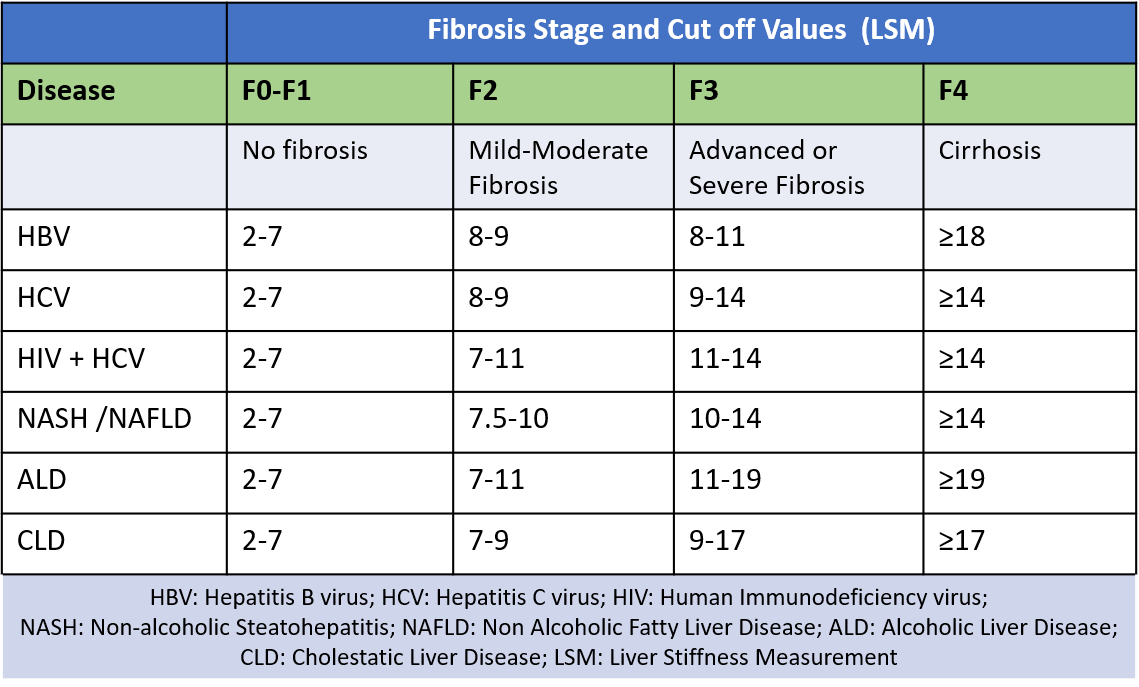
Cirrhosis is diagnosed by FibroScan and histologically staged by liver biopsy. The FibroScan measures LSM (liver stiffness measurement ) that indicates and grades the amount of fibrosis (measured in kPa). Normal values for liver stiffness range from 2-7 kPa, while in cirrhosis it can go to 15 or more up to a maximum of 75kPa.
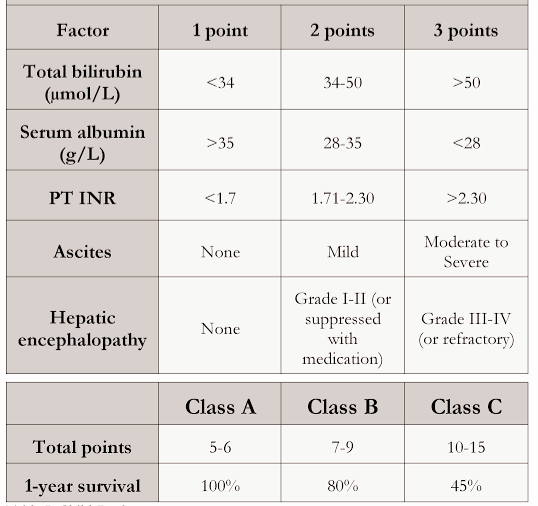
The risk of mortality due to cirrhosis is assessed by the Child Pugh Score below.
Treatment
Cirrhosis when diagnosed indicates advanced and often end-stage liver disease. It requires regular monitoring for liver function, progression, and signs of liver failure.
The patient is registered for liver transplant and advised precautionary procedures like endoscopy and banding of varices (dilated tortuous blood vessels of the food pipe) to prevent bleeding. Sometimes an interim shunt surgery called transjugular intrahepatic portosystemic shunt (TIPS) may be performed to ease out the back pressure in the portal vein and protect against gastrointestinal bleeding.
Medicines for cirrhosis are given mainly to reduce and detoxify ammonia that builds up as the liver cannot convert it to urea. Such medicines include-
- gut antibiotics like rifaximin to control ammonia-producing gut bacteria.
- laxatives like lactulose or lactitol that maintain bowel function and produce an acidic gut milieu inhibiting ammonia-producing bacteria.
- probiotics that increase friendly gut bacteria and reduce ammonia-producing bacteria.
- amino acids like LOLA (L-ornithine L-aspartate) that divert ammonia to form glutamine
- BCAA (branched-chain amino acids – leucine, isoleucine, and valine) which regulate protein synthesis and turnover, increase ammonia uptake from blood, and maintain glutamate-glutamine levels.
- diuretics to reduce fluid accumulation and swelling.
- terlipressin and octreotide to treat variceal bleeding
- beta blockers to reduce portal hypertension, and prevent variceal bleed.
- electrolyte imbalance if present should be corrected.
- infections may need appropriate antibiotics
Also read:
Fatty Liver – 5 Important Points of Awareness and Understanding


